1. Background
Multiple sclerosis (MS) is the most common non-traumatic disabling chronic disease of the nervous system among young people (1), with a wide range of symptoms facing the life of patients with many challenges (2). Patients have to deal with the complexity of the disease, increased limitations in functioning and disease progression, and reduced life expectancy (3). Recurrence, progression, and symptoms are unpredictable in this disease, which creates fears about the future for many patients and uncertainty in their lives and affects their adaptation and well-being (4).
Fear of Progress (FOP) is introduced as an emotional and non-neurological reaction. The fear is caused by the internal experience of an unpredictable and life-threatening illness. It can be placed along a spectrum of “dysfunctional” and “functional” fear (5). The fear about the progression and recurrence of the disease is described by the fear of dying and the fear of becoming a burden on the family and appears to be an important meta-diagnostic construct related to distress and challenges (6, 7).
According to researchers, FOP is one of the common symptoms of discomfort in patients with cancer and other chronic conditions (8), such as patients (9). However, high levels of fear of disease progression can affect well-being, social functioning, and, finally, quality of life (8). Also, researchers have reported that FOP is strongly associated with anxiety and depression (6).
Various treatments have been proposed to deal with FOP, including cognitive-behavioral treatments (10), client-centered supportive treatments (11), and education based on acceptance and commitment (12). It seems that collaborative care can also be an effective strategy.
Collaborative care is defined as a logical and regular process of dynamic and effective interaction between the clients and the health care providers in order to understand better and recognize the needs, problems, and expectations in the disease control process. In this model, unlike the traditional approach, the focus is not solely on the nurse as the primary caregiver. Instead, it emphasizes the importance of group participation in the caregiving process, which is designed and implemented in 4 stages: motivation, preparation, involvement, and evaluation (13, 14).
Researchers have shown the positive effect of the collaborative care model in different contexts, such as depression (15, 16), diabetes (17), HIV (18), heart failure (19, 20), cancer (21), mental illnesses (22), and hyperactivity (23). However, in some studies, this model has not shown a significant effect (24, 25). The chronic, progressive, and unpredictable nature of MS can have significant biological, social, and psychological effects on the patients and their families, which can intensify the constant fear of disease progression.
2. Objectives
Due to conflicting results and the lack of a similar study, this study was designed to determine the effect of the collaborative care model on the fear of disease progression in MS patients.
3. Methods
3.1. Study Design
This randomized controlled trial was performed at the Multiple Sclerosis Clinic affiliated with Rafsanjan University of Medical Sciences from July 2021 to January 2022 in Rafsanjan, Iran, on 300 MS patients who had medical records.
3.2. Sample and Sampling Methods
The sample size was estimated at 34 patients and their main caregivers in each group based on previous studies (26), with a standard deviation of 7.2, the minimum expected difference of 4 between the groups for the FOP score, Type 1 error of 0.05, and power of 99%. Considering the possibility of dropout, 79 patients and their main caregivers were assigned into study groups (42 patients and their caregivers in the intervention and 43 in the control group). The caregivers were one of the patient’s family members.
First, sampling was done purposefully based on the inclusion criteria. Then, the eligible subjects were assigned to study groups using the random minimization method (27) by the primary researcher. The assignment was based on the types of MS, which were categorized into 4 groups: Clinically Isolated Syndrome (CIS), Relapsing-remitting MS (RRMS), Secondary Progressive MS (SPMS), and Primary Progressive MS (PPMS) (28). The first samples were assigned into the different categories by lottery, and for assigning subsequent samples, the sum of samples in each group and category was considered, so the total number of samples in each category of different groups was equal.
The inclusion criteria for patients were having a definite diagnosis of MS based on the information in the patient’s medical record, at least 18 years old, at least 6 months of MS history, no serious mental disorder, no use of psychoactive drugs, no addiction, not suffering from other incurable diseases at the same time, including neurology, hematology, oncology, infectious, and kidney diseases and diseases requiring special care, no history of cognitive disorders, and no mental illnesses. Inclusion criteria for caregivers were the age range of 18-75 years, the ability to read and write, being the main caregiver, and not having a mental illness. Exclusion criteria for patients and their caregivers were moving or absence from more than one session of each stage and unwillingness to continue participating in research.
3.3. Instruments
The data were collected using a two-part questionnaire. The first part measured demographic characteristics (age, gender, education level, marital status, job, and type of MS), and the second part represented the Fear of Progression Questionnaire-short form (FOP-Q-SF) (29). Herschbach and Dinkel designed this scale in 2005 for chronic diseases (29). They revised it in a short form in 2013, with 12 items answered on a 5-point Likert scale from 1 (never) to 5 (always) and a total score ranging from 12 to 60. The higher scores indicate a greater fear of disease progression. The reliability (Cronbach’s α > 0.7) and validity of this scale (with coefficients 0.77- 0.94) were confirmed (30). The scale was approved for cancer patients in Iran by Hasannezhad Reskati et al. in 2022 (31). The questionnaires were filled out twice before and immediately after the study by self-reporting. For illiterate cases, it was filled by the researcher through a face-to-face interview.
3.4. Interventions
For the intervention group, in addition to routine care, the collaborative care model was implemented in four stages: Motivation (in the first week in a 90-120-minute session), preparation (in the second week in a 90 - 120-minute session), engagement (in two collaborative care training sessions in the third and fourth weeks and two follow-up visits, with two weeks apart and the second training session in 90 - 120 minutes), and evaluation (before and after each session and finally at the end of week 9 from the beginning of the intervention) (32). The personalized (for each patient and their caregiver together) collaborative care model was compiled in simple language and according to the educational, cultural, and socioeconomic conditions of the patients and caregivers by the first author, the responsible nurse, and the physician of the clinic. The training classes were held at the MS clinic located in Ali Ibn Abitaleb Hospital for three months (according to the model structure). For the control group, the previous routine procedures were continued, and at the end of the study, an educational booklet was provided to them.
Before the study, the conditions of the research were explained to the patients and their main caregivers; then, written informed consent was obtained from the patients and their families, and the FOP-Q was completed. At the beginning of the study, an initial health assessment was done in order to identify patients’ health problems, and their care needs were listed by doctors and nurses who were members of the collaborative care team. The team members included a doctor, two nurses, patients, and one of the patients’ main caregivers. It should be noted that the patients and caregivers were unaware of the kind of study group.
Data analysis was done using SPSS software (version 22) with the Shapiro-Wilk test, descriptive statistics (mean, standard deviation, and frequency), chi-square test, Fisher Exact test, paired t-test, and independent t-test at a 95% confidence level.
3.5. Ethical Consideration
In order to observe the research ethics, the proposal was approved by the research council of Rafsanjan University of Medical Sciences, and the code of ethics was obtained (IR.RUMS.REC.1400.039). While obtaining written informed consent, the researchers assured patients and families that participation or non-participation in the study would not have any effect on the quality and quantity of the center’s services.
4. Results
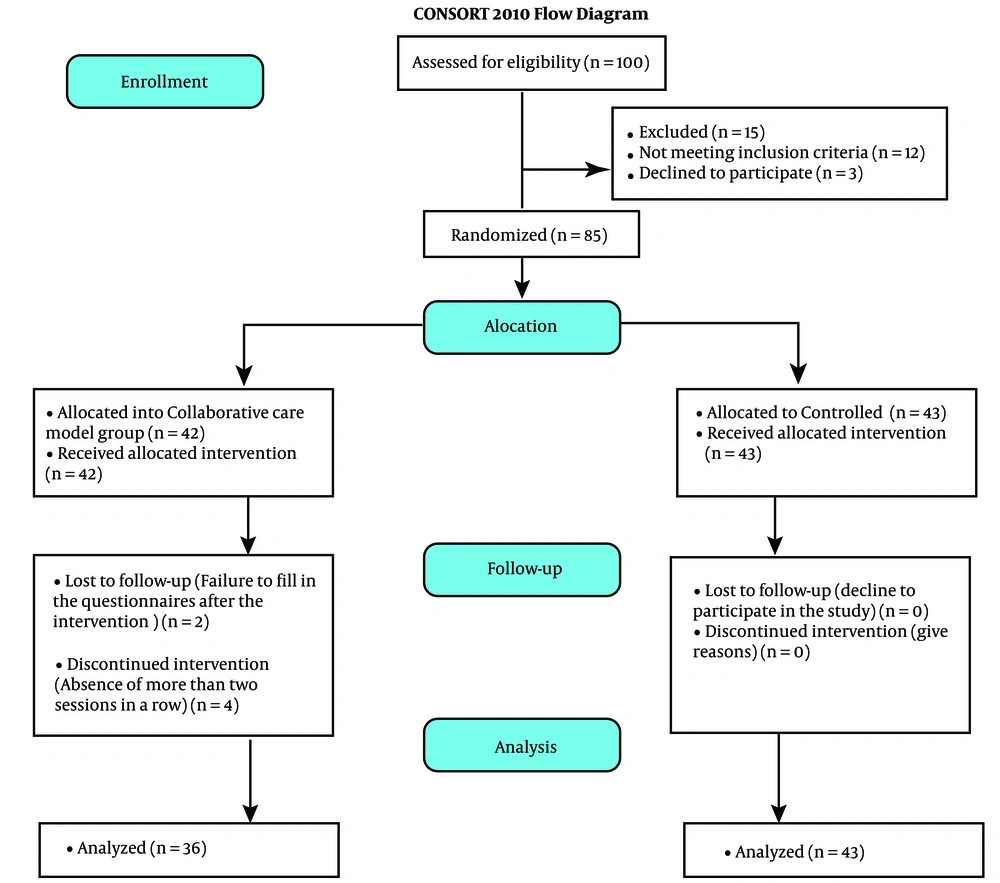
Finally, 79 participants were analyzed. The sampling process is shown in the CONSORT form in Figure 1.
The Shapiro-Wilk test results showed that the distribution of the quantitative variables was normal. The mean ± SD of patients’ age was 38.22 ± 9.24 with a minimum of 20 and a maximum of 66 years. There were 69 (87.3%) female patients and 57 (72.2%) male caregivers. The mean ± SD of the patient’s age was 40.25 ± 8.90 and 36.51 ± 9.34 in the intervention and control groups, respectively. Also, the mean ± SD of the caregivers’ age was 44.03 ± 13.2 and 43.95 ± 10.93 in the intervention and control groups, respectively. There was no statistically significant difference in the patients’ (P = 0.074) and caregivers’ (P = 0.978) ages between the studied groups. Table 1 shows that the study groups were also similar in terms of other demographic characteristics.
| Caregivers of Collaborative Care Group (n = 36) a | Caregivers of Control Group (n = 36) a | P-Value | Collaborative Care Group (n = 36) a | Control Group (n = 43) a | P-Value | |
|---|---|---|---|---|---|---|
| Gender | 0.3707 | 0.08 b | ||||
| Male | 28 (77.8) | 29 (67.14) | 34 (94.4) | 35 (81.4) | ||
| Female | 8 (22.2) | 14 (37.6) | 2 (5.6) | 8 (18.6) | ||
| Education | 0.054 | 0.330 c | ||||
| Illiterate | 2 (5.6) | 1 (2.3) | 1 (2.8) | 1 (2.3) | ||
| Under Diploma | 13 (36.6) | 13 (30.3) | 11 (30.6) | 8 (18.6) | ||
| Diploma | 15 (41.7) | 16 (37.2) | 17 (47.2) | 18 (41.9) | ||
| Academic | 6 (6.7) | 13 (30.2) | 7 (19.4) | 16 (37.2) | ||
| Job | 0.287 | 0.145 c | ||||
| Unemployed | 2 (5.6) | 16 (37.2) | 1 (2.8) | 4 (9.3) | ||
| Housewife | 5 (13.9) | 13 (30.2) | 29 (80.6) | 25 (58.1) | ||
| Self-employed | 21 (58.3) | 2 (4.7) | 2 (5.6) | 8 (18.6) | ||
| Employed | 8 (22.2) | 14 (32.6) | 4 (11.1) | 6 (14) | ||
| Marital status | 1.000 | 0.335 | ||||
| Single | 2 (5.6) | 2 (4.7) | 4 (11.4) | 8 (18.9) | ||
| Married | 34 (94.4) | 41 (95.3) | 32 (88.9) | 35 (81.4) | ||
| Type of MS | - | 0.743 c | ||||
| CIS | - | - | 23 (63.9) | 31 (72.1) | ||
| RRMS | - | - | 7 (19.4) | 5 (11.6) | ||
| PPMS | 1 (2.8) | 2 (4.7) | ||||
| SPMS | 5 (13.9) | 5 (11.6) |
Abbreviations: CIS, clinically isolated syndrome; RRMS, relapsing-remitting multiple sclerosis; PPMS, primary progressive multiple sclerosis; and SPMS, secondary progressive multiple sclerosis.
a Values are presented as No. (%).
b Chi-square test.
c Fisher Exact test.
In the intervention group, the mean ± SD of the FOP score was 37.80 ± 12.22 before the intervention, which reached 34.86 ± 12.21 after the intervention; the paired t-test showed a significant reduction (P = 0.001). In the control group, the mean ± SD of the FOP score was 38.39 ± 11.41 before the intervention, which reached 40.20 ± 11.68 after the intervention. The paired t-test showed that the FOP score increased statistically significantly after the intervention (P = 0.001).
The between-group comparison showed that both groups were similar in terms of the FOP score before the intervention (P = 825). The independent t-test showed that although the mean score of FOP was lower in the intervention group than in the control group after the intervention, this difference was borderline and statistically insignificant (P = 0.051) (Table 2).
Abbreviation: FOP, fear of progression.
a Values are presented as mean ± SD.
b Independent t-test.
c Paired t-test.
5. Discussion
Overall, the results showed that the FOP score was reduced in the intervention group compared to the control group, which was close to the significance level.
Researchers have had limited focus on investigating the impact of collaborative care on FOP in patients with MS. However, the positive effect of the collaborative care model on other outcomes has been shown in MS patients. A study from Khuzestan, Iran, in 2018 showed that the collaborative care model promoted hope in patients with MS and their family caregivers (33). In another study from Washington (2018), the collaborative care model had a positive effect on depression and pain management in patients with MS (34). Also, the collaborative care models have been successful in reducing the severity of symptoms and increasing the quality of life in other chronic diseases in a review study in 2023 (35). The difference between the results of these studies and the current research can be attributed to the conditions of conducting the research, which coincided with the outbreak of COVID-19, the high stress load, and the fear of the disease progression at that time. It seems the biggest difference is in the measured variable because they did not assess FOP.
In another context, a review of preliminary data from several collaborative models shows that collaborative care programs for dementia patients have benefits such as reduced behavioral symptoms of dementia, improved function and quality of life, less use of acute medical services, and reduced caregiver burnout. Researchers concluded that these could facilitate the provision of highly effective dementia care while reducing associated medical costs (36). The results of another review also showed that collaborative care, with or without consideration of cultural/linguistic matching, is potentially effective in improving depression among racial/ethnic minorities, including those from low socioeconomic backgrounds (37). Recently, a systematic review reported that family-centered collaborative care reduced disease recurrence and re-hospitalization of patients with chronic mental illnesses (38). In general, it can be claimed that managing the symptoms of chronic diseases, especially for psychological conflicts, despite its challenges, has been successful in supporting these patients’ psychological issues (39, 40).
Based on the literature, it can be acknowledged that collaborative care has been used in different societies with different models and mechanisms. Because the design and strategy of collaborative care model implementations were not well defined, especially the family-oriented model, the findings of various studies may have limited application to the general population. In contrast, the limitations of research samples, especially in qualitative studies, and some methodological limitations cannot be ignored. Despite the fact that the present study tried to obtain results by matching the groups in terms of disease category and FOP scores at baseline, as well as double-blinding and regular and accurate following-up, the role of individual characteristics and mental state of subjects in understanding the FOP questions cannot be ignored. Also, the conditions in the COVID-19 period could have affected the quality of interpersonal relationships.
5.1. Conclusions
The study results showed that the collaborative care model was potentially an effective strategy for managing FOP in MS patients. Future research is necessary to determine the characteristics of therapeutic models.