1. Context
Women’s sexual health and well-being stand as critical concerns in the realm of reproductive and sexual health (1). A pivotal facet of this domain is sexual satisfaction, denoting the experience of pleasure and contentment among partners within a marital relationship (2). It holds substantial significance, as heightened sexual satisfaction correlates with increased marital contentment, fortifying the foundation of families and fostering stronger relationships (3). Conversely, a lack of sexual pleasure can precipitate separation and emotional distancing between partners, potentially contributing to elevated divorce rates (4), a global issue that has seen a surge in recent decades (5), including in Iran from 1988 to 2018 (1, 6). Surveys indicate that 68.4% of women and 66.7% of men seeking divorce attribute their decision to a lack of sexual satisfaction (7). Unfortunately, some women face barriers to receiving adequate counseling and care due to feelings of shame, fear of sexual stigma, or lack of access to appropriate resources (3).
In the era of information technology, there has been significant growth and progress in medical services, health care, therapy, and teleconsultation, including applications of mobile health (m-Health), electronic health (e-health), and electronic consultation (e-consultation) on smartphones (8-12). Feedback and education, prevention, treatment, and self-care have had a great impact, making healthcare more accessible and convenient (12). Until the 1980s, traditional approaches were used to treat sexual disorders. However, a paradigm shift occurred with the introduction of computer-based interventions for the treatment of sexual problems. Previous studies suggest that internet-based sex therapy may be more accepted than face-to-face therapy (8, 12-14).
The COVID-19 pandemic has accelerated the adoption and expansion of telemedicine and consultation methods (15, 16). Telemedicine includes online examinations, surgery, education, and consultations via telephone, smartphones, email, websites, and health applications (16, 17). These methods are not only used to maintain and improve people’s health but also to improve the quality of service delivery by professionals (11, 12, 18). This method is characterized by convenience, affordability, availability, and confidentiality. It has no geographical restrictions and eliminates the need to travel, making it non-judgmental and helping to continue treatment (2, 3, 10, 19). Telemedicine has the potential to increase sexual knowledge, promote sexual health, provide related services, and even prevent sexually transmitted infections (13).
2. Objectives
This study aimed to comprehensively explore the challenges and opportunities inherent in telemedicine as it pertains to enhancing women’s sexual satisfaction. A nuanced understanding of these aspects is crucial for mitigating potential drawbacks, amplifying the benefits, and ultimately enhancing the overall quality of telemedicine service provision in the context of sexual health.
3. Data Sources
This research is based on the recommended systematic review and meta-analysis checklist, the newest version of PRISMA 2020 (20). Additionally, it has been formally registered with PROSPERO under the code CRD42023479693.
A comprehensive search of articles was conducted without time restriction until January 1, 2023, in Scopus, Web of Science (WOS), and PubMed databases. To ensure a comprehensive review, the reference list of the identified articles was also manually searched.
The PICO (Patient, Intervention, Comparison, Outcome) technique was employed to develop the search strategy and select appropriate keywords aligned with the study’s object. The study aimed to explore the relationship between sexual satisfaction as a problem (P) and telemedicine as an intervention (I). For the outcome (O), a vast range of keywords was used to cover all potential outcomes. The comparison concept was not considered in this study to maintain search comprehensibility. The review incorporated all studies, irrespective of their outcome, study design, and type. Synonyms, related terms, and keywords associated with these concepts were identified.
To search, the terms were combined using “OR” within each group, while “AND” was used to connect the different groups of terms to ensure a comprehensive search. These terms were derived from prior research and the MeSH (Medical Subject Headings) database. Keywords, study titles, and abstracts were considered to identify appropriate terms and improve the effectiveness of the search strategy. Table 1 shows the concepts, keywords, and their combinations used. The search strategy related to each database is provided in Appendix 1.
| Main Concept | Keywords |
|---|---|
| Population/subject: Sexual health | Sexual dysfunction OR sexual disorder OR sexual difficult OR sexual problem OR sexual complaint |
| Intervention: Mobile technology | “Mobile app” OR “mobile apps” OR smartphone OR “mobile health” OR “mHealth” OR “m health” OR “m-health” OR “smart phone” OR “Cellular phone” OR “Cell phone” OR “Cellphone” OR “cellular telephone” OR tablet OR PDA OR iPad OR “Application Softwares” OR “Applications Software” OR “Mobile Applications OR “telemedicine OR “mobile health” OR “mHealth” OR “m health” OR “m-health” |
| Outcome: Aim of the interventions | Satisfaction OR management OR Education OR training OR consultation OR promotion OR enhancement OR care OR change OR empowerment |
4. Study Selection
The inclusion criteria for this review required the articles to meet the following criteria:
(1) Articles that focused on the utilization of telemedicine techniques to enhance sexual satisfaction.
(2) All electronically published RCTs or quasi-randomized studies in peer-reviewed journals.
(3) Published articles available up until October 30, 2022.
(4) The target population consisted of females who engage in sexual activity consistently.
(5) The availability of article abstracts in the initial search.
The studies were excluded for the following reasons:
(1) Non-English language: Studies conducted in languages other than English were excluded from the review.
(2) Literature types: Books, review articles, conference papers, theoretical essays, editorial and commentary letters, opinion articles, and gray literature were not included in the review.
(3) Specific demographics: Studies that focused solely on telehealth methods tailored to the specific needs of homosexuals and bisexual individuals were excluded.
(4) Unrelated purposes: Studies where telehealth methods were utilized for purposes unrelated to sexual satisfaction and health were excluded.
5. Screening Method and Removing Irrelevant Articles
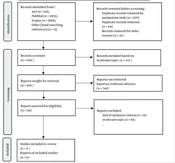
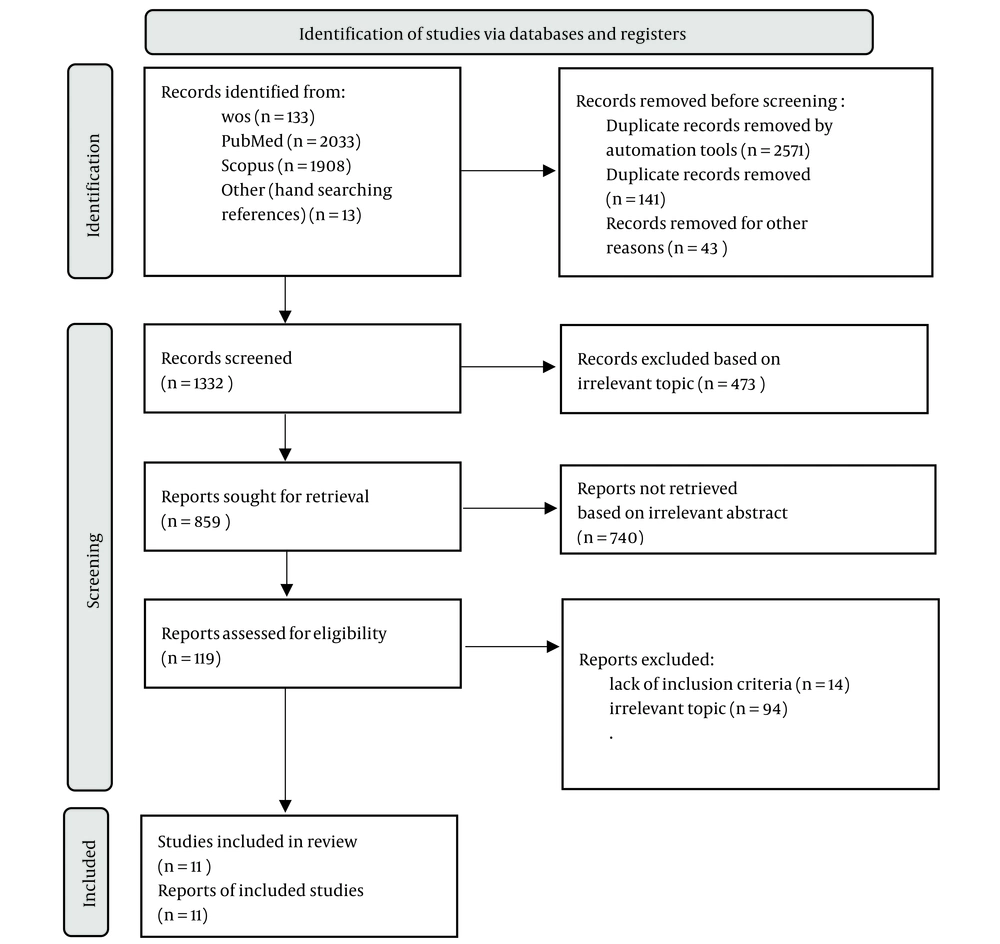
A total of 4 087 records (133 from WOS, 2033 from PubMed, and 1908 from Scopus) were retrieved. Additionally, 13 more articles were identified through the examination of references in the retrieved studies. Among these studies, 2 571 duplicate articles were eliminated using automation tools (EndNote), and an additional 141 duplicate articles were removed after thorough re-examination by researchers (SA, EJ). The remaining 1 332 articles underwent a review process conducted by two researchers (SA, EJ), during which 43 titles were excluded due to not conforming to the article format but rather resembling a book or a speech presented at a conference or congress. This process resulted in 473 articles being considered for inclusion based on predefined criteria for titles and abstracts.
After applying the inclusion criteria, 740 articles were excluded, and the full-text eligibility of the remaining 119 articles was assessed by two researchers (SA, EJ). After the evaluation of full-text articles for eligibility, 108 articles were excluded based on exclusion criteria and irrelevant topics, ultimately leaving 11 eligible studies. The article selection procedure is summarized in Figure 1.
Two reviewers (SA and EJ) independently screened the identified articles and extracted the study data using a researcher-made form. In cases of disagreement between the authors, consensus was reached among them. If necessary, any disputes were further checked and resolved with the input of another researcher (Kh M).
6. Data Extraction
In this systematic review, a table incorporating general and technical information from the articles was meticulously designed for data extraction. This table encompasses key details for each article, including the first author’s name, year of publication, country of research, study design, problems, population, intervention details, challenges and opportunities identified, and a section for discussion. To ensure accuracy, any potential ambiguities during the data extraction process were systematically addressed through discussions within the research team. In instances where clarification was necessary, efforts were made to contact the authors of the respective studies. It is noteworthy that, in our study, the data extraction stage encountered no ambiguities, as all required information was explicitly stated in the articles.
7. Quality Assessment
The quality assessment of the articles was independently conducted by two researchers, SA and EJ. Any disagreements that arose between the reviewers were resolved through discussion between them and, if necessary, with the involvement of another author (Kh M). The quality assessment was done using the modified Jadad instrument, consisting of eight items (Table 2).
| Authors | Was the Research Described as Randomized? | Was the Approach of Randomization Appropriate? | Was the Research Described as Blinding? | Was the Approach of Blinding Appropriate? | Was There a Presentation of Withdrawals and Dropouts? | Was There a Presentation of the Inclusion/Exclusion Criteria? | Was the Approach Used to Assess Adverse Effects Described? | Was the Approach of Statistical Analysis Described? | Total Score |
|---|---|---|---|---|---|---|---|---|---|
| Brotto et al., 2022 (2) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 3 |
| Hummel et al., 2015 (21) | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| Brotto et al., 2017 (22) | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 2 |
| Hummel et al., 2019 (23) | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 5 |
| Hucker and Mccabe, 2015 (24) | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 6 |
| Hensel et al., 2022 (25) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Schover et al., 2012 (26) | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 5 |
| Hummel et al., 2017 (27) | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 5 |
| Schover et al., 2013 (28) | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| Reese et al., 2012 (29) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 3 |
| Classen et al., 2012 (30) | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 3 |
This instrument comprises eight questions, with a positive response earning 1 point and a negative response scoring 0 points. Consequently, each study could achieve a score ranging from 0 to 8 (31, 32). In this structured review, articles with lower scores were not excluded, as blinding the study was not feasible. Additionally, certain studies featured a limited sample size due to the specificity of the patient population, making randomization impractical.
8. Results
The study selection process is shown in Figure 1A total of 4 087 records were identified from the searches. No unpublished manuscripts were identified. After excluding 4 076 records, a total of 11 articles that met the inclusion criteria were included in the present systematic review. The characteristics and findings of the reviewed articles are summarized in Table 3.
| First Author | Study Design | Problem | Population | Tools of Telemedicine | Intervention | Challenges | Opportunities | Discussion |
|---|---|---|---|---|---|---|---|---|
| Brotto et al.: Canada: 2022 (2) | Quasi -experimental | Sexual dysfunctions | Women with SIAD | Website | Online mindfulness | Lack of adequate engagement of couples | Providing multimedia content, easy to use, adaptation of a face-to-face mindfulness program to online delivery | The usefulness and effectiveness of online mindfulness interventions |
| Hummel et al.: Netherlands: 2015 (21) | RCT | Sexual dysfunctions | Breast cancer survivors | Website | Online counselling + CBT | No | Privacy protection, patient-specific, patient-provider communication, engagement of couples | Effectiveness of internet-based CBT interventions |
| Brotto et al.: Canada: 2017 (22) | Quasi -experimental | Sexual dysfunctions | Colorectal and gynaecologic cancer survivors | Not explained | Psychoeducational program, including mindfulness meditation | The lack of a “live” component, being time-consuming, embarrassment to post questions in the group, Internet access problems | Easy to read and access (accessibility) the self-directed pace of the program, (easy to use) found accessible(accessibility) the mean level of technical difficulty was also very low, (easy to use) | Significant improvement in the scores of libidos, arousal, lubrication, satisfaction, and overall sexual performance after the intervention and 6 months later. |
| Hummel et al.: Netherland: 2019 (23) | Quasi -experimental | Sexual dysfunction | Breast cancer survivors | Via email | Briefly, the CBT by the psychologist/sexologist | No | Eliminate geographic access problems, eliminate problems related to embarrassment by raising sexual problems, Couple of interactions in the program, Couple Conflict, Communication with the patient’s provider, privacy protection | Improvement of intention-to-treat analyses of overall sexual function, sexual satisfaction, overall sexual satisfaction, and sexual satisfaction during Internet-based CBT |
| Hucker and Mccabe: Australia: 2015 (24) | RCT | Sexual dysfunctions | Women with Mixed Female Sexual Problems | Chat Groups/e-mail contact with a therapist/ Pursuing Pleasure (PP website) | Online CBT that included psychoeducation, sensate focus | No | Privacy protection, real-time, Patient-Patient Communication, Patient-Provider Communication | Significant improvement in libido, arousal, sedation, orgasm, and satisfaction in women who completed the PPP program compared to a waitlist control group |
| Hensel et al.: USA: 2022 (25) | Quasi -experimental | Not | Women | Website | OMGyes.com was designed as a resource for all individuals to gain information about ways to increase sexual pleasure. | No | No | Acceptability of resources focused on enjoyment as well as reading experience, positively changing the way women think and supporting sexual pleasure |
| Schover et al.: Texas: 2012 (26) | RCT | Sexual dysfunctions | Couples after localized prostate cancer treatment | Website | CAREss included exercises and, -CBT | Internet access problems | Providing multimedia content, privacy protection patient provider communication, tracking the online behavior of participants, affordability, improve patient provider communication, accessibility or easy to access | Significant improvement in female participants’ sexual dysfunction |
| Hummel et al.: Netherland: 2017(27) | RCT | Sexual dysfunctions | Breast cancer survivors | Telephone/e-mail | The internet-based CBT includes standardized information texts, homework assignments, a report to the sexologist, and feedback from the sexologist. | no | Privacy protection, providing patient-provider communication | Effect of internet-based CBT on sexual function, body image, and menopausal symptoms in BCS with sexual dysfunction |
| Schover et al.: Texas: 2013 (28) | RCT | Sexual dysfunctions | Women with cancer-related FSD | Website | Tendrils Web site includes text, graphics, animations, and multicultural | The usability of the website may also have been a limitation (usability issues) of using the site | Privacy protection, provide multimedia content, no need to visit for consultation-providing the non-face-to-face consultation | Significant improvement of sexual performance and satisfaction in women with sexual dysfunction with an Internet-based intervention |
| Reese et al.: USA: 2012 (29) | Quasi -experimental | Sexual dysfunctions | Couple with colorectal cancer | Telephone | The Intimacy Enhancement intervention behavioral skills for coping with sexual challenges. Techniques from both sex therapy and couple/marital therapy | Insufficient interaction with the content (lack of sufficient participation of couples in telephone intervention) | Eliminate geographic access problems, easy to use for remote patients | Effectiveness of a program to help patients with colorectal cancer and their partners in physical intimacy and sexual relationships by increasing skills to cope with the effects of cancer treatment. |
| Classen et al.: Canada: 2013 (30) | Interventional | Sexual dysfunctions | Women with gynecologic cancer | Website | GyneGals web-based support group-The psycho-educational material | Lack of tracking of the online behaviors of participants | Sharing experience, comfortable discussing sexual issues in a web-based support group, reducing stigmatization | The acceptability of the result of the intervention in the participating women |
Abbreviations: SIAD, sexual interest/arousal disorder; CBT, cognitive behavioral therapy; BCS, breast cancer survivor; FSD, female sexual disorder; RCT, Randomized controlled trials; FSD, female sexual disorder.
9. Details of Articles
9.1. Date and Country of Research
Eleven articles with a focus on different geographical regions were included in the selection of studies. Among these, three studies were conducted in Canada (2, 22, 30), three studies were centered on the Netherlands (21, 23, 27), four studies were conducted in the United States (25, 26, 28, 29), and one study was conducted in Australia (24). Notably, Asian countries did not contribute to the studies included in this review.
Regarding the timeframe of the selected studies, although no specific time limit was defined by the researchers of this review, the studies were conducted between 2011 and 2022.
10. Research Design
In terms of study designs, ten of the studies adopted a quantitative approach (2, 21, 23-30), while one study employed a mixed methods approach (22), integrating both quantitative and qualitative designs concurrently. Among the conducted studies, five were classified as clinical trials (21, 24, 26-28), while the rest were categorized as semi-experimental studies (2, 22, 23, 25, 29).
11. Target Groups in Studies
Seven studies specifically targeted women diagnosed with either breast or colorectal cancer who experienced sexual dysfunction and related issues after undergoing treatment (21-23, 27-30). Additionally, one of the studies focused on the wives of men undergoing prostate cancer treatment (26). Among these studies, two specifically investigated females with sexual dysfunctions (2, 24), while one study included females regardless of any issues or ailments (25).
12. Approaches Used in Interventions
The cognitive behavioral therapy (CBT) approach was used in five studies (21, 23, 24, 26, 27), and the mindfulness method was used in two studies (2, 22). Sensate focus was used in a study simultaneously with CBT (24). In one study, only education and improving the level of knowledge related to increasing sexual pleasure were investigated (25). In ten studies, the aim was to improve sexual function (2, 21-24, 26-30), while in only one, the goal was to increase satisfaction and pleasure (25).
13. Telemedicine Approach in Studies
In terms of the telemedicine approach utilized in the studies, seven studies were conducted through a website platform, enabling remote access and communication (2, 21, 24-26, 28, 30). One study employed telephone conversations as the primary mode of interaction (29). Another study utilized email communication as the main method of engagement (24). Additionally, one study employed a combination of email and telephone discussions simultaneously (27). Unfortunately, one study did not offer any details about the telemedicine approach used (22).
14. Challenges and Opportunities
In these studies, 38 opportunities were identified and classified into 14 categories:
(1) The increasing demand for telemedicine services: The Corona Pandemic-Advances in Science and the emergence of Internet-based methods.
(2) Ease of use: User-friendly interface, ease of applying mindfulness compared to face-to-face methods, clear and straightforward content, suitable design for users, customizable usage options, moderate complexity in content design and presentation.
(3) Involvement of couples in exercises: Integration of couples in therapy – specific module for sexual partners.
(4) Safeguarding patient privacy and confidentiality: User interface privacy - patient anonymity - site design with password protection–discussion forum with an anonymous username and password - personal user account with secure and password-protected email
(5) Facilitating interactive and accessible communication between the patient and the therapist: Phone communication with the therapist-two-way communication via email-unlimited email contacts with the therapist-email feedback-personal messenger for therapist communication
(6) Utilization of multimedia content: Incorporation of text, video, and animation.
(7) Recognizing the commonality of the issue: Providing forums for patient communication, facilitating opportunities for patients to share their sexual experiences, and offering online support groups.
(8) Fostering patient motivation: Active participation in the treatment process-fostering spontaneity.
(9) Eliminating the geographical barrier: Use of phone or email instead of unnecessary trips-the use of non-personal counseling methods-the use of non-personal training-a departure from traditional face-to-face interventions.
(10) Mitigating stigma-related concerns: Comfortable discussion of sexual issues in a group setting-sharing sexual experiences.
(11) Minimizing the financial burden of interventions: Lower consultation fees - no insurance compensation for in-person visits
(12) Availability: Convenient and fast access to services-accessibility regardless of distance - overcoming limitations of face-to-face and traditional counseling.
(13) Save time: Prompt responses from a consultant-flexibility in completing exercises
(14) Maintaining control over patient engagement: Monitoring the number of visits and interventions completed by the patient
In this systematic review, nine challenges were identified and categorized. These challenges highlight potential barriers and limitations associated with the implementation of telemedicine interventions for enhancing sexual satisfaction. It is important to address these challenges to optimize patient engagement and adherence to the prescribed interventions. By identifying and addressing these obstacles, healthcare providers can enhance the effectiveness and impact of telemedicine approaches in addressing sexual concerns.
(1) Lack of spouse participation
(2) Inadequate follow-up on patient behavior
(3) Requirement of technological skills
(4) Need for internet access
(5) Dependency on specific devices such as laptops, smartphones, or personal computers
(6) Lengthy and time-consuming exercises
(7) Interference with work hours and occupation
(8) Embarrassment and exercise avoidance
15. Discussion
This systematic review included 11 experimental and semi-experimental studies that met the inclusion criteria. The studies were conducted in Canada (2, 22, 30), the Netherlands (21, 23, 27), the United States (25, 26, 28, 29), and Australia (24). It is worth noting that no studies were conducted in Asian and African countries. This suggests that the use of telemedicine to address sexual issues has been on the rise in developed countries over the past decade. This trend is likely due to the widespread availability and development of the internet, as well as changing cultural attitudes towards the use of technology in various fields of healthcare and treatment. A systematic review conducted in the United States on telemedicine communication in healthcare has highlighted the significant expansion of this technology in recent decades (33). In contrast to the present systematic review, it was observed that the most significant growth of M-Health occurred in Africa. This is likely due to the difference in the focus of the study, which was maternal and child health in sexually transmitted diseases (e.g., HIV), which are more prevalent in Africa and require more intervention. A study was conducted on the opportunities and challenges of telemedicine during the COVID-19 pandemic (34). The results showed that the United States and China had the largest share of telemedicine services. This is likely due to the high number of COVID-19 cases in these areas and the need for non-face-to-face medical services.
The use of websites has emerged as the most common method of providing telehealth services in reviewed studies (3, 17, 20, 22, 24, 31, 32). This can be attributed to the longer history of using websites compared to mobile apps. However, a systematic review conducted in Iran on telehealth and diabetes found that the use of SMS to control diabetes is more effective (35). This variation could be attributed to differences in the type of intervention required to address the issue. For people with diabetes, a simple reminder to take medication is often enough, while for people with sexual disorders, a wider range of information is best provided through websites. A study on the challenges and opportunities of telemedicine during the COVID-19 pandemic found that the primary method of telemedicine delivery was through telephone conversations (34). This might be attributed to the rapid spread of the pandemic, as using the telephone remains the fastest way to deliver services.
Some of the significant opportunities identified in this systematic review include closer communication, the potential to monitor participants’ performance during treatment, improved communication with others, and the engagement of the patient’s sexual partner in treatment. In a study on the use of companion health to enhance the well-being of individuals with chronic diseases (14), the potential for personalized intervention in discussion forums and the involvement of sexual partners in improving sexual health were highlighted as opportunities.
In this systematic review, challenges were also found that should be identified and resolved to optimize the effectiveness of these interventions so that service providers can improve the quality of interventions.
Telemedicine for sexual problems faces challenges, including the non-participation of spouses and insufficient follow-up of patient behavior. These challenges were underscored in a systematic review concentrating on sexual issues in patients with chronic diseases (14). Furthermore, another systematic review focusing on telemedicine for sexually transmitted diseases (36), along with a third review examining the challenges and opportunities of M-Health (37), also brought attention to these issues. To address these challenges, we recommend mandatory participation of spouses in non-attendance interventions, as their active involvement can significantly improve sexual problems. Additionally, we suggest conducting needs assessment studies and producing exclusive and user-friendly content with an interactive nature, including multimedia content in non-face-to-face interventions, to increase participants’ adherence and monitor their activities.
The need for technological skills and access to the necessary tools and the Internet is another challenge that can limit the target community. This challenge was also mentioned in a study conducted in Pakistan and Australia (38, 39). While increasing internet penetration can reduce this challenge to some extent, designing non-face-to-face multimodal services that can be accessed through alternative means can increase the scope and expand the scope and reach of the intervention to a wider audience.
Consequently, by recognizing and addressing these challenges, service providers can transform them into opportunities to increase the effectiveness and accessibility of telehealth interventions aimed at improving sexual satisfaction and addressing sexual issues. While most of the studies in this systematic review highlighted the positive effects of the telemedicine approach, it is important to acknowledge that the results may not be fully generalizable to the entire gynecological population. Participants in these studies may have certain conditions or characteristics that affect the results. Therefore, more research studies are needed to examine the challenges and opportunities of using telehealth approaches in sexual health from the audience’s perspective.
It is essential to acknowledge certain limitations in our study that warrant consideration. Firstly, our search was confined to three databases—WOS, PubMed, and Scopus—potentially affecting the comprehensiveness of our search results. Additionally, our search strategy was restricted to English language studies, introducing a potential language bias. However, it is noteworthy that English is widely recognized as the universal language of science, and the majority of studies are published in this language. Importantly, gray literature was not incorporated into our study, representing another limitation.
15.1. Conclusions
After conducting this systematic review and analyzing studies in the field of sexual satisfaction and health, it was discovered that there are both challenges and opportunities associated with remote health interventions in this area. The features of telemedicine, such as user-friendliness, cost-effectiveness, and no time limit, contribute to its ease of use and accessibility for users. These factors make it easier for people to engage with a telehealth approach, leading to a greater likelihood of continued participation and adherence to interventions. In addition, the geographical dimension and distance from face-to-face services in the field of sexual health can create barriers to accessing counseling and education. With telemedicine, these barriers can be overcome, as people can receive healthcare services online, eliminating the need for physical proximity and travel. By eliminating the need for face-to-face counseling and providing the option of anonymity, people feel comfortable sharing their problems and concerns without fear of the stigma associated with seeking sexual health services. By gaining a deeper understanding of these challenges and opportunities, we can work towards improving sexual health services and making them more accessible and effective for everyone.