1. Background
As the coronavirus disease 2019 (COVID-19) pandemic has progressed, healthcare professionals have become the most crucial resource in providing care to patients on the frontlines in the battle against the disease worldwide (1). In this context, the strict use of personal protective equipment (PPE) and adherence to standard precautions (SP) in the healthcare team can contribute to the reduction of occurrences of COVID-19 and infections related to healthcare-associated infections (HAI) (2).
The idea of SP is to ensure minimum infection prevention practices in healthcare, and despite significant preparedness and improvements following the experience of previous epidemics, adherence to ideal practices remains insufficient overall among healthcare professionals (3). In this regard, a study pointed out that 72% of the infections affecting healthcare professionals with COVID-19 were related to the exposure of a co-worker or patient source of infection, and most of these infections were associated with a reason for non-full adherence to recommended PPE (4).
The countries most affected by non-adherence to SP are low- and middle-income countries, where infectious diseases are on the rise, leaving professionals more susceptible (5). Adherence to SP is below what is recommended in a hospital environment and in primary health care (PHC), where the perception of risks is reduced, contributing to this deficit and resulting in a lack of knowledge, attitudes, and potential facilitators (5).
Therefore, adherence to SP is a global public health problem that is still suboptimal (6). For example, in a study carried out with 81 transferred nursing professionals, the adherence rate to using PPE in a university hospital was 72.9% (7). In the context of the COVID-19 pandemic crisis, nursing can lead in designing and implementing programs that not only enhance care quality but also foster teamwork through interprofessional collaboration (8).
Educational programs play a strategic role in care innovation. A review study assessing the impact of interventions on professional behavior concluded that strategies involving collaborative training, along with the use of auditing and feedback, are effective in modifying health professionals' behavior (9).
A review of the literature showed that several studies have explored adherence to standardized rules among both professionals and nursing students (9-12). Notably, these studies employed multivariate approaches to examine different educational strategies. For example, a study with nursing students compared the effectiveness of conventional lecture programs to flipped learning (z); however, another study investigated the impact of educational videos versus reading standard operating procedures on the understanding of standard practices (12). Despite these findings, the results of these studies have sometimes been contradictory or even inconclusive, particularly in terms of the effectiveness of these methods when used in isolation or in direct comparison (9-12).
This inconsistency in the results underscores the necessity for the current research. This study aimed to fill the knowledge gap by examining the combined effect of educational strategies. This study proposes a new multimodal intervention comprising five stages, integrating a validated educational video with a problematizing discussion based on a quiz (true or false). By combining these strategies, which were previously explored separately or juxtaposed in earlier research, the present study sought to provide a more comprehensive understanding of effective educational practices in nursing.
Health education is a crucial means of improving professional knowledge. In this regard, the implementation and evaluation of multimodal educational strategies are imperative to determine their effects on the adherence of professionals working in COVID-19 care sectors, especially in a pandemic scenario.
2. Objectives
This study aimed to measure the self-reported adherence of nursing professionals to SP before and after an educational intervention during the COVID-19 pandemic period.
3. Methods
3.1. Study Design
This was a quasi-experimental, before-and-after study. Quasi-experimental studies involve an intervention applied to the experimental group, with results compared without using randomization. The study was conducted within February to June 2022 and involved the development of an educational intervention without randomization.
3.2. Setting and Sampling
The study was conducted in the municipality of Três Lagoas, located in eastern Mato Grosso do Sul, Brazil, which has a population of 123 281 inhabitants (13). The hospital where the study was conducted is currently a reference in the state of Mato Grosso do Sul due to the wide regionalization of care it provides. The hospital serves 10 municipalities in the state and has a total of 166 beds, of which 90% (151) are allocated to care in the Unified Health System (SUS) (11).
The study encompassed 129 nursing professionals. However, 30 nursing professionals who were not in direct contact with patients during the data collection period were excluded. These excluded subjects were professionals who occupied managerial rather than caregiving roles. Consequently, the final sample comprised 99 participants. The sample power was calculated using G*Power software, considering a total of 99 individuals, an error (alpha) of 0.05, a two-tailed distribution, and an effect size of 0.40. After the project, an analysis power of 97.2% was obtained. The research instruments were applied in various sectors, including the hospitalization unit, intensive care unit (ICU), emergency room, hemodialysis, and others not reported by the professionals. The study specifically targeted professionals who worked in the studied sectors during the pandemic period. Furthermore, the study was conducted during the institution's period of lowest turnover.
3.3. Instruments
Initially, the nursing professionals who agreed to participate in the study completed a sociodemographic characterization instrument (including gender, age, professional category, time working in the hospital, and working hours per week) (14). Compliance with Standard Precautions Scale (CSPS) was used to verify compliance with SP. This instrument was validated for nursing professionals (15) and was developed in China by Lam (16) to evaluate compliance with SP among nursing professionals. It consists of 20 items with 5 dimensions, including the use of PPE, disposal of sharps, disposal of waste, decontamination of used articles and spills, and prevention of cross-infection.
3.3.1. Compliance Scale with Standard Precautions
The Compliance scale with standard precautions (CSPS) is a Likert-type scale, ranging from 1 (never) to 4 (always), with a total of 20 items. For the CSPSS questionnaire, each response option "always" is assigned a score of "one," and for the options "often," "rarely," or "never," the assigned score is "zero." For the inverted questions, the option "never" confers a score of "one," and for the others, a score of "zero." The maximum score is 80 points; the closer the score is to this value, the greater the adherence to SP (15). This scale underwent translation, cultural adaptation, and reliability. The Brazilian version of the CSPS scale presented an excellent level of understanding, with a Cronbach’s alpha and the intraclass correlation coefficient of 0.61 and 0.85, respectively (15).
3.4. Multimodal Educational Intervention
This study was organized based on Seki's study (17) and consisted of five phases. These phases included strategies, such as the use of a validated educational video (18) and quizzes with true or false questions, focusing on topics with lower correct response rates (cut-off point below 70%) (2).
3.4.1. Phase 1 - Initial Approach and Application of Instruments
Initially, nursing professionals providing direct assistance were approached. They were informed about the study and gave their consent through the Informed Consent Form (ICF). After obtaining consent, sociodemographic characterization instruments and the CSPS were administered. These instruments were self-reported by the professionals. Data collection for this phase occurred within February to March 2022. An educational intervention followed in April, with a second round of questionnaires in May and June 2022. It is important to note that during this period, despite the World Health Organization (WHO) declaring a pandemic, there were no social isolation requirements, masks were not mandatory, and there was a decrease in deaths and serious cases alongside an increase in vaccination rates.
3.4.2. Phase 2 - Analysis of Responses and Construction of Educational Intervention
The multimodal intervention was based on Centers for Disease Control and Prevention (CDC) recommendations regarding precautionary measures. The intervention focused on questions with a lower percentage of correct answers in phase 1 (cut-off value < 70%). A validated educational video, reviewed by 13 experts using the Delphi technique, was used to encourage adherence to SP (18). Prior to the intervention, a meeting with the medical and nursing coordination of the Hospital Infection Control Committee and the institution's management was held. This phase lasted 20 days in April 2022.
3.4.3. Phase 3 - Application of Educational Intervention
The intervention occurred in April 2022 and covered all shifts at the institution. It lasted 3 days, with 30-minute sessions for groups of up to 10 professionals.
3.4.4. Phase 4 - Application of the Instrument to Verify Adherence to Standard Precautions
After the educational intervention, the questionnaires were readministered over a period of 30 days in May 2022.
3.4.5. Phase 5 - Comparative Data Analysis
This phase involved a comparative analysis of adherence before and after the educational intervention, conducted over 30 days in June.
3.5. Statistical Analysis
The Statistical Package for the Social Sciences (SPSS) software version 20.0 was used. Categorical variables were represented by absolute and relative frequencies. The scores before and after the intervention were represented by mean and standard deviation. The Wilcoxon test evaluated significant differences; however, the Mann-Whitney and Kruskal-Wallis tests assessed rank differences between independent numerical variables, along with the Komolgorov-Smirnov normality test. A Spearman correlation analysis was conducted between scores before and after the questionnaires and sociodemographic characteristics. Cochran's Q test assessed differences in the proportion of each questionnaire item. The McNemar-Bowker test evaluated differences in responses before and after the intervention.
3.6. Ethical Considerations
The present study adhered to national and international guidelines for research involving human subjects. This study was approved by the Research Ethics Committee of the Federal University of Mato Grosso do Sul Foundation (UFMS) under Opinion no. 4,218,227. The research participants were assured of the confidentiality and privacy of the information collected and the preservation of their anonymity. Data collection occurred after the participants voluntarily provided their consent by signing the ICF.
4. Results
Among the 99 nursing professionals (nurses, nursing technicians, and nursing assistants) who comprised the final sample of the study, 77.7% were nursing technicians (professionals with a 2-year technical level course), 19.1% were nurses (professionals with a higher education degree from a 5-year program), and 3% were nursing assistants (technical-level professionals with a 1-year training course). The ICU had the highest representation, with 21.2% of the participants. Notably, approximately 88.8% of the nursing professionals reported having worked at the institution for a duration of 0 to 10 years (Table 1).
| Variables | No. (%) |
|---|---|
| Gender | |
| Female | 85 (85.9) |
| Male | 14 (14.1) |
| Professional category | |
| Nursing technician | 77 (77.7) |
| Nurse | 19 (19.1) |
| Nursing assistant | 3 (3.0) |
| Which department do you work in? | |
| ICU (Intensive Care Unit) | 21 (21.2) |
| Hemodialysis | 15 (15.2) |
| ER (Emergency Room) | 14 (14.1) |
| Inpatient units | 46 (46.5) |
| Other | 3 (3.0) |
| Age range | |
| 20 to 40 years | 69 (69.6) |
| 40 years or older | 27 (28.2) |
| Others | 3 (3) |
| Duration of employment at the hospital | |
| 0 to 10 years | 87 (87.8) |
| 11 to 20 years | 7 (7) |
| 21 to 30 years | 4 (4) |
| Uninformed | 1 (1) |
| Hours worked per Week | |
| Up to 44 hours | 70 (70.7) |
| More than 44 hours | 18 (18.1) |
| Up to 30 hours | 10 (10.1) |
| Uninformed | 1 (1) |
Sociodemographic Characterization Data of Nursing Professionals (Três Lagoas, MS, Brazil, 2022)
In Table 2, we can observe how adherence to PPE occurred by nursing professionals before and after educational intervention, and the items that obtained statistically significant changes in the result, with regard to the correct use of the sharps box (P = 0.023), the removal of PPE in designated locations (P = 0.034), covering wounds with bandages before contact with a patient (P = 0.003), exchanging gloves between one patient and another (P = 0.025), reusing disposable masks (P = 0.005), use of aprons/coats when exposed to body fluids (P = 0.004), and decontamination of surfaces and equipment after use (P = 0.033).
| Questions | Before the Intervention (Agreement with the Content of the Questions) | After the Intervention (Agreement with the Content of the Questions) | P-Value | ||
|---|---|---|---|---|---|
| Yes | No | Yes | No | ||
| 1- I wash my hands between patient contacts. | 93 (93.9) | 6 (6.1) | 97 (98.0) | 2 (2.0) | 0.157 |
| 2- I only use water to wash my hands. | 74 (74.7) | 25 (25.3) | 80 (80.8) | 19 (19.2) | 0.221 |
| 3- I use alcohol-based hand sanitizer as an alternative if they are not visibly dirty. | 37 (37.4) | 62 (62.6) | 40 (40.4) | 59 (59.6) | 0.622 |
| 4- I recap used needles after giving an injection. | 82 (82.8) | 17 (17.2) | 79 (79.8) | 20 (20.2) | 0.549 |
| 5- I dispose of sharps in proper boxes. | 95 (96.0) | 4 (4.0) | 98 (99.0) | 1 (1.0) | 0.083 |
| 6- The sharps box is discarded only when it is full. | 14 (14.1) | 85 (85.9) | 26 (26.3) | 73 (73.7) | 0.023 |
| 7- I remove personal protective equipment (PPE) at a designated location. | 73 (73.7) | 26 (26.3) | 84 (84.8) | 15 (15.2) | 0.034 |
| 8- I shower in case of extensive splashes, even if I use EPI. | 41 (41.4) | 58 (58.6) | 42 (42.4) | 57 (57.6) | 0.869 |
| 9- I cover my wounds or injuries with waterproof dressings before contact with patients. | 67 (67.7) | 32 (32.3) | 82 (82.8) | 17 (17.2) | 0.003 |
| 10- I wear gloves when I am exposed to bodily fluids, blood, or derivatives and any patient excretion. | 97 (98.0) | 2 (2.0) | 98 (99.0) | 1 (1.0) | 0.317 |
| 11- I change gloves between contact with patients. | 94 (94.9) | 5 (5.1) | 99 (100.0) | 0 (0.0) | 0.025 |
| 12- I wash my hands immediately after removing gloves. | 94 (94.9) | 5 (5.1) | 94 (94.9) | 5 (5.1) | >0.99 |
| 13- I wear a surgical mask or, in combination with goggles and an apron, whenever there is a possibility of splashes or spills. | 80 (80.8) | 19 (19.2) | 89 (89.9) | 10 (10.1) | 0.072 |
| 14- My mouth and nose are covered when I wear a mask. | 94 (94.9) | 5 (5.1) | 91 (91.9) | 8 (8.1) | 0.317 |
| 15- I reuse a surgical mask or disposable PPE. | 61 (61.6) | 38 (38.4) | 80 (80.8) | 19 (19.2) | 0.005 |
| 16- I wear an apron/gown when I am exposed to blood, body fluids, or any patient excretion. | 69 (69.7) | 30 (30.3) | 84 (84.8) | 15 (15.2) | 0.004 |
| 17- I dispose of material contaminated with blood, body fluids, secretions, and excretions of patients in white plastic bags, regardless of the infectious status of the patient. | 85 (85.9) | 14 (14.1) | 89 (89.9) | 10 (10.1) | 0.218 |
| 18- I decontaminate surfaces and equipment after use. | 86 (86.9) | 13 (13.1) | 94 (94.9) | 5 (5.1) | 0.033 |
| 19- I use gloves to decontaminate equipment that has visible dirt. | 89 (89.9) | 10 (10.1) | 94 (94.9) | 5 (5.1) | 0.197 |
| 20- I immediately clean surfaces with disinfectant (alcohol) after spilling blood or other bodily fluids. | 89 (89.9) | 10 (10.1) | 92 (92.9) | 7 (7.1) | 0.439 |
Adherence Ratio According to Each Item of the Compliance with Standard Precautions Scale Before and After the Multimodal Educational Intervention
The scoring before and after the intervention was represented with mean and standard deviation. The Wilcoxon test was conducted to assess possible significant differences. The methodology employed in this study did not involve summing up points on the questionnaire. Instead, it focused on the frequency of correct answers. The analysis did not compute a cumulative score; rather, it tracked how often each question was answered correctly or incorrectly. For example, for the first question, 93 individuals answered correctly, representing 93.9% of the respondents.
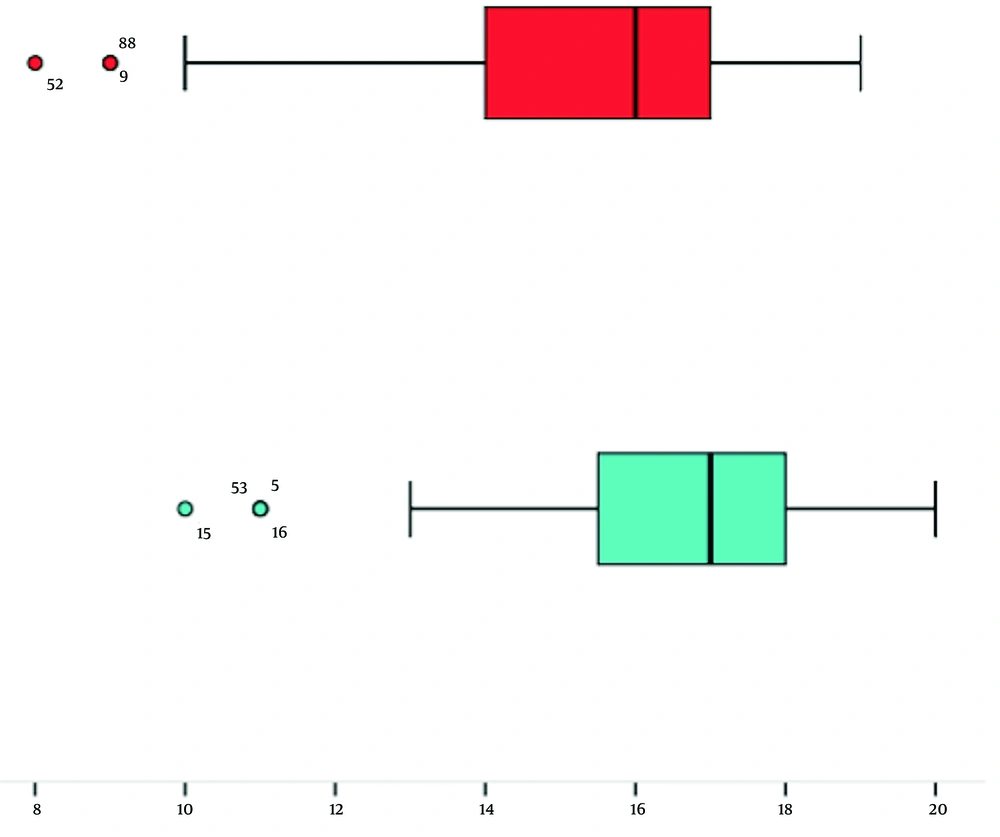
Figure 1 illustrates a significant difference in the performance of health professionals before and after the educational intervention. The scores before the intervention were 15.29 ± 2.23, and after the intervention, they improved to 16.48 ± 1.98 (W = -4.443; P < 0.05). This indicates not only an increase in the number of correct answers but also a reduction in variability and standard deviation across most questions. The score improvement was determined by comparing the total number of correct responses before the intervention to the total after the intervention.
Based on the analysis of the results, there was an increase in the percentile of self-reported adherence by nursing professionals after the educational intervention. A decrease in the standard deviation was observed, indicating less dispersed scores among health professionals.
5. Discussion
The use of a multimodal educational intervention, incorporating an educational video and a questionnaire focused on questions with a higher error rate (70%), resulted in a significant increase in adherence to SP among nursing professionals. The results of the present study align with those of similar studies conducted with nursing professionals in Bangladesh (19) and Iran and with students in China (20). Factors such as the duration, intensity, content, and pedagogical approach of the intervention, the prior experience of healthcare professionals, the organizational culture of the workplace, workload, and available resources might have influenced the intervention's success in various contexts. These factors should be taken into account when interpreting the results and planning future educational interventions (19).
The effectiveness of the current intervention is attributed to its comprehensive approach, combining diverse educational tools and addressing specific knowledge gaps identified during the pre-intervention phase. This issue aligns with previous studies, which have highlighted the benefits of incorporating elements, such as educational videos and targeted questionnaires, to enhance information retention and the practical application of acquired knowledge (21, 22). Furthermore, the prior identification of knowledge deficiencies among healthcare professionals is consistently emphasized as a critical step in developing effective interventions (22, 23).
Regarding subtopics, professional performance and the handling of sharp materials are particularly noteworthy. The difficulty in adhering to these practices persists even after the educational intervention, with 79.8% of respondents reporting the recapping of needles after use. Generally, the prevalence of needle recapping among nursing professionals ranges from 27.5% (24) to 41% (25). Factors such as study location, workload, and the classification of nursing professionals influence this prevalence, explaining the difference between the findings of the present study and the literature (26, 27).
Before the educational intervention, only 14.1% of professionals correctly stated that sharps disposal boxes should be discarded only when full. After the intervention, the percentage of correct responses increased to 26.3%. The literature commonly reports significant improvements in knowledge and safety practices following the implementation of targeted educational interventions for material disposal (28). Studies indicate that after receiving clear information and guidance on the safe disposal of sharps containers, nursing professionals can develop a better understanding of the consequences associated with improper disposal, such as risks of accidents with sharp objects and exposure to pathogens. This understanding might lead to stricter adherence to disposal guidelines (20, 29, 30).
In the current study focusing on the proper disposal of PPE, it was observed that before the educational intervention, 73.7% of professionals reported correctly disposing of PPE. This figure increased to 84.8% following the intervention. The data of the present study are supported by previous studies that have also highlighted the effectiveness of multimodal interventions in enhancing the proper disposal of PPE (22, 26, 28). Such interventions, which incorporate various educational tools, have proven more effective in addressing specific knowledge gaps previously identified during the baseline phase, thereby facilitating more effective learning.
In an earlier survey conducted among nursing staff at a public university hospital, the data were collected regarding the use of PPE. Despite potential exposure to blood splashes, body fluids, or secretions, only 55.6% of professionals reported using protective masks (7). Compared to the current survey, it is apparent that the educational intervention also led to satisfactory outcomes in reducing the reuse of surgical masks. Before the intervention, 38.1% of participants reported reusing surgical masks, a figure that fell to 19.2% post-intervention.
An increase was noted in the use of gowns or aprons when handling body fluids, with 84.8% of professionals adopting this practice after the intervention. This trend suggests that the knowledge imparted through the intervention positively influenced biosafety practices (31-33).
Remarkably, about 94.9% of professionals demonstrated awareness of the importance of surface decontamination in hospital settings after the intervention, a notably high figure that distinguishes the findings of the current study from those of other similar studies, which reported lower prevalence rates (34, 35). This success can be attributed to several factors that underscore the efficacy of the educational intervention, ranging from the clarity of the conveyed information to the emphasis on the practical significance of surface decontamination for patient safety.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has brought significant changes to global healthcare services, underscoring the importance of PPE and altering patient care behaviors (36-38). An increase was noted in the practice of changing gloves between patient care, with all professionals reporting this measure after the intervention, compared to 94% before the intervention. This high compliance can be attributed to enhanced awareness of the importance of infection prevention measures in the context of a global pandemic (22). The pandemic highlighted the necessity of stringent hygiene and personal protection practices, and educational interventions played a pivotal role in ensuring healthcare professionals are well-informed and motivated to adopt these practices.
Based on the findings of the present study, it is essential for future research to focus on exploring the long-term sustainability of similar educational interventions and their applicability in other healthcare settings. Moreover, there is an urgent need for an in-depth investigation into the specific components of multimodal educational programs that might contribute most significantly to their effectiveness.
Assessing the long-term sustainability of interventions is crucial to understand if the improvements observed in safety practices and adherence to healthcare guidelines are maintained over time. This issue will allow for determining whether these interventions have a lasting and continuous impact or if constant and periodic reinforcements are necessary (39).
The applicability of these interventions in various healthcare settings is due to the differences observed in work environments, which lead to unique challenges in terms of culture, resources, and the population served. Therefore, understanding how these interventions can be successfully adapted and implemented in different contexts is fundamental to expanding their reach and effectiveness (40).
5.1. Limitations
This study's limitations include reliance on self-reported data, which might not accurately reflect actual practices. However, the educational intervention emphasized the importance of adherence. The study was also limited to a single hospital institution, a reference center for 10 municipalities. A strength of this study is its combination of two educational strategies, assessing their impact on adherence to SP in a pandemic scenario.
5.2. Conclusions
The results of the present study demonstrated, in a pioneering manner, that the use of a multimodal educational strategy (combining different approaches such as the use of five moments, a validated video, and a question-and-answer quiz) had a positive impact on adherence by professionals who work in sectors caring for patients with COVID-19.
The positive impact of these strategies on self-reported adherence by nursing professionals has valuable and important implications for management in healthcare settings. This increase in adherence not only raises the quality of professional care practice but also plays a crucial role in patient safety and advancing the teaching-learning process. Therefore, the present study uniquely contributes by demonstrating the combined effects of various educational strategies, thereby providing a more holistic approach to improving adherence to SP.
Despite the limitations, it is recommended that future research delves into the factors and aspects influencing adherence to SP in the daily practice of healthcare professionals, exploring the long-term efficacy of such interventions, variations across different healthcare settings, and primarily the impact on patient outcomes. This understanding would provide deeper insights and guidance for the development of effective, evidence-based training programs in the healthcare sector.