1. Background
On March 11, 2020, the World Health Organization (WHO) declared the outbreak of the novel coronavirus (COVID-19) a global pandemic of the century due to the increasing incidence of cases in many countries (1). The COVID-19 pandemic has caused almost unimaginable damage to the lives, health, and economy of many countries. Along with health and behavioral control actions, vaccination is the most successful method to control the epidemic of COVID-19 (2). The launch of the COVID-19 vaccine with different platforms in a short period of time was a turning point in the fight against this epidemic (3). Although vaccination is an effective way to reduce and eliminate diseases, its effect depends on the willingness of the community to receive the vaccine (4). Studies at the beginning of the COVID-19 outbreak estimated that 25 - 50% of Americans do not intend to receive the COVID-19 vaccine after the availability of the vaccine, which is a new challenge in health promotion (5). For this reason, WHO declared vaccine hesitancy as one of the ten global health threats (6). Despite the development of safe vaccines on different platforms (7, 8), a major challenge in vaccination planning and implementation is reluctance to vaccinate. According to the definition of WHO, vaccine hesitancy refers to non-acceptance or delay in accepting vaccination, despite its availability (9). Acceptance of a newly introduced vaccine is a complex behavior and the rate of acceptance in different societies is affected by context, culture, time, place, perceived behavior, geography, and socio-demographic factors (10). A study on the influenza vaccine showed that the knowledge and attitude of healthcare workers are related to the acceptance of the vaccine by the general population (11). Healthcare workers play a crucial role in bridging the gap between healthcare systems and patients. Research has shown that the degree of acceptance of the COVID-19 vaccine among healthcare workers directly affects their recommendation to patients. Consequently, individuals often rely on the guidance of healthcare professionals to ultimately decide whether to accept or reject the vaccine. Deferring or hesitating to vaccinate healthcare workers can hinder efforts to achieve herd immunity against COVID-19 and lead to elevated rates of illness and death. Additionally, negative attitudes pertaining to vaccination shared by healthcare workers can influence others in a detrimental manner (12-14).
According to a study conducted in America, it was found that only one-third of health workers choose to promptly uptake the vaccine, while the rest opt to delay their decision until there is publication of reliable scientific data within this area. Similarly, in other nations, a relatively low percentage of health workers express their willingness to receive the vaccine promptly. In Egypt, the figure stands at 21% (15), while in Qena it drops to 3.39% (16). On the contrary, Saudi Arabia exhibits a comparatively higher rate, with 50% (17) of health workers expressing their intention to receive the vaccine promptly. These studies show the huge difference among medical workers in different countries regarding their willingness to accept or not to accept the COVID-19 vaccine. The role of healthcare workers in convincing people and communities as reliable advisors to attract their participation to benefit from vaccination services is undeniable (18).
2. Objectives
Since qualitative research has the ability to discover the depth and complexities of a phenomenon and confirm knowledge through the experiences of people involved in the phenomenon, therefore, the qualitative content analysis approach was used to explain the understanding of care workers about the COVID-19 vaccination.
3. Methods
3.1. Type of Research and Study Setting
The current research is a qualitative study with a conventional qualitative content analysis approach. It was carried out from March 2021 to May 2021 in Khoy in the northwest of Iran. Qualitative content analysis gives the researcher the opportunity to analyze the explicit and descriptive content as well as the latent and interpretive content of the texts (19).
3.2. Sampling and Data Collection
According to qualitative research, purposeful sampling with maximum diversity was used (20).
The inclusion criteria in this study were those medical workers who were the first group in the country to receive the COVID-19 vaccine and were willing to express their experiences. In order to observe the maximum diversity in sampling, health workers of different ages, of both sexes, and from different professions such as doctors, nurses, midwives, pharmacists, laboratory staff, and radiologists were included in the research.
The data collection method was semi-structured interviews. The corresponding author approached the participants and after stating the purpose of the research, invited them for the interviews. Interviews were conducted before the start of the work shift or afterward as agreed and only by the corresponding author. The interviews were conducted in a private room in the hospitals, observing social distance, and wearing a mask. Open questions were chosen as interview guides, and follow-up questions were asked after them. The main question that was asked at the beginning of the interview was: “Please express your feelings as the first group of recipients of the COVID-19 vaccine?” Exploratory questions about feelings, beliefs, and concerns were asked after the initial answer. The duration of the interview ranged from 35 minutes to 45 minutes. After 16 interviews, no new information was obtained, and theoretical saturation was achieved.
3.3. Data Analysis Method
Simultaneously with collecting information, the process of data analysis was carried out using the conventional content analysis method of Graneheim and Lundman (21). After each interview, the researcher immediately listened to the audio file again. Then the conversation text was transcribed, and the interview text was reviewed several times by the researcher and colleagues. Next, meaning units were extracted from the participants' own statements in the form of primary codes. These codes were then classified based on semantic and conceptual similarity, aiming to keep them as concise as possible. Finally, the data were organized into broader and more conceptual main categories, and themes were abstracted. All coding and classification steps were performed using MAX Qdata software version 2007.
3.4. Data Rigor
Trustworthiness was established using the criteria proposed by Guba and Lincoln, namely credibility, dependability, confirmability, and transferability (22). In this context, the text of the interviews with some participants was reviewed, and their additional comments were incorporated. Additionally, the research team had long-term involvement with the data, and the data analysis process was conducted continuously and comparatively. If any conflicts arose during the analysis process, they were resolved through discussion and by allocating sufficient time.
3.5. Ethical Considerations
Furthermore, all ethical considerations in this research, including obtaining permission from the faculty ethics committee (IR.KHOY.REC.1400.002), securing informed consent from the participants to participate in the study, and ensuring the anonymity of the participants in the research, were addressed. The participants completed an informed consent form, granting permission to record the conversation and use the information anonymously. The right to withdraw from participation was respected throughout the study.
4. Results
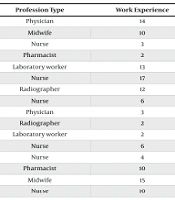
Participants were 16 female and male medical workers. Their age and work experience ranged from 24 to 52 years and from 2 to 17 years, respectively (Table 1).
| Participant Number | Sex | Age | Profession Type | Work Experience |
|---|---|---|---|---|
| 1 | Male | 44 | Physician | 14 |
| 2 | Female | 35 | Midwife | 10 |
| 3 | Female | 25 | Nurse | 3 |
| 4 | Female | 30 | Pharmacist | 2 |
| 5 | Female | 48 | Laboratory worker | 13 |
| 6 | Male | 52 | Nurse | 17 |
| 7 | Male | 45 | Radiographer | 12 |
| 8 | Female | 28 | Nurse | 6 |
| 9 | Female | 29 | Physician | 3 |
| 10 | Female | 24 | Radiographer | 2 |
| 11 | Male | 25 | Laboratory worker | 2 |
| 12 | Female | 28 | Nurse | 6 |
| 13 | Female | 26 | Nurse | 4 |
| 14 | Female | 48 | Pharmacist | 10 |
| 15 | Female | 52 | Midwife | 15 |
| 16 | Male | 32 | Nurse | 10 |
After analyzing the transcribed interview texts, we identified seven subcategories and three main categories. The main categories were “conflicting feelings,” “continuation of the fight against COVID-19,” and “getting rid of COVID-19” (Table 2).
| Themes | Sub-themes |
|---|---|
| 1. Conflicting feelings | 1.1. Confidence or doubt |
| 1.2. Hope or worry | |
| 1.3. Complications and benefits | |
| 2. Continuing of the fight against COVID-19 | 2.1. Responding to social/professional responsibility |
| 2.2. Encouraging people to accept the vaccine | |
| 3. Getting rid of COVID-19 | 3.1. Return to normal life |
| 3.2. Reduction of mortality |
4.1. Conflicting Feelings
In all the interviews, the healthcare workers tried to express the concept that the COVID-19 pandemic and the urgency to vaccinate the medical staff as the first people in the country caused them to have conflicting feelings about the effectiveness of the vaccine. The subcategories of this category included “confidence or doubt”, “hope or worry”, and “complications and benefits”.
4.1.1. Confidence or Doubt
The participants stated that they had conflicting feelings about vaccination and were hesitant to make a decision. On the one hand, they were confident about the importance of vaccines from a scientific point of view, and on the other hand, they doubted it due to the rapid preparation of the COVID-19 vaccine. A participant describes his feelings like this:
“I know the vaccine is good. We have gone through so much about the vaccine in the university courses. But can you really trust the vaccine that was made so quickly!!!” (Participant 4).
4.1.2. Hope or Worry
Most participants expressed dual feelings. Although they were worried about new vaccines, the hope of improving the current situation made them accept vaccination.
“We were the first group to get vaccinated, so I thought we were being tested. I was afraid and worried, but I researched on the internet and saw that those who were vaccinated did not have much problem. I overcame my feelings and injected them” (Participant 15).
“I was afraid of the vaccine, but because of my job in the hospital, I took it, hoping not to transmit the disease to my family” (Participant 11).
4.1.3. Complications and Benefits
Another factor that caused the participants to have conflicting feelings about the vaccine was that there was a lot of true and false information about the vaccine.
“Some say that vaccination has many side effects. Those who take the vaccine get a gene mutation, but some say no. In any case, we as the first group should be vaccinated” (Participant 10).
4.2. Continuation of the Fight against COVID-19
The continuation of the fight against COVID-19 was another significant aspect derived from the interviews with the medical staff. They endeavored to convey the notion that vaccination equates to persisting in the battle against the COVID-19 virus. In essence, they viewed accepting vaccination as the first individuals in society, despite doubts, worries, and fears of complications, as part of their professional responsibility. They expressed that by doing so, they aimed to alleviate people's fear of vaccination and encourage its acceptance. This category included two additional subcategories named “response to social and professional responsibility” and “encouraging people to accept the vaccine”.
4.2.1. Responding to Social/Professional Responsibility
All participants in the research emphasized that one of their professional and social responsibilities is vaccination to continue the fight against COVID-19.
A nurse with over 20 years of experience stated, “I consider vaccination as the primary line of treatment in my professional responsibility. When I witness patients succumbing every day despite all the care, I am compelled to advocate for vaccination” (Participant 8).
Another participant remarked, “as a lung specialist, it is my duty to diagnose and treat COVID-19 patients. Firstly, I volunteer and request to receive the vaccine because I believe it is a professional obligation. People will not embrace vaccination until we set an example” (Participant 9).
4.2.2. Encouraging People to Accept the Vaccine
Healthcare workers felt that by accepting vaccination as the first group in the country, they have taken a stride toward the general public's acceptance of vaccination. An example of participants' quotes is provided below:
“I strongly advise all those who inquire to get vaccinated; it is not really dangerous” (Participant 2).
“My friends and family all inquire what to do when it's our turn to receive the vaccine. I know they heed my words. I tell them to go for it” (Participant 1).
“People trust us as a scientific reference. I received the vaccine so that others would follow suit. I want the general public to get vaccinated because the virus is truly lethal. Do not hesitate; head to the nearest health center and get vaccinated” (Participant 9).
4.3. Getting Rid of COVID-19
Getting rid of COVID-19 was another category obtained from this qualitative study. All medical staff believed that despite their conflicting feelings, they had to overcome these conflicts to return to normal life and eliminate COVID-19.
4.3.1. Return to Normal Life
The medical staff stated that returning to life before the coronavirus disease was one of the factors that facilitated the acceptance of the COVID-19 vaccine. They felt tired of the restrictions experienced in their work and personal lives and desired to eliminate COVID-19.
“I also administer the vaccine myself and recommend that everyone do it. We are truly exhausted; we want to return to our normal daily routine, to be able to go home, confidently hug our children, go to restaurants, use the elevator, and...” (Participant 5).
“We want the COVID-19 restrictions to be lifted and for sports activities and lifestyle to return to normal. I am very happy to play a role in restoring life to its usual routine” (Participant 10).
4.3.2. Reduction of Mortality
Most participants expressed that by accepting vaccination as the first target group, they aimed to help reduce mortality and eliminate COVID-19.
“I want to contribute to decreasing the death rate. We are weary of witnessing and hearing news of death” (Participant 16).
5. Discussion
The findings of this qualitative study provided us with important information about the perception of the medical staff towards COVID-19 vaccination. The results of this study can provide valuable insights for developing appropriate strategies to control emerging and infectious diseases in the future.
Data analysis revealed 3 main categories and 7 subcategories. The main categories extracted included “conflicting feelings,” “continuing the fight against COVID-19, and getting rid of COVID-19.”
The first category that emerged in this study was conflicting feelings. Confidence or doubt, hope and worry, side effects, and benefits of vaccination were among the dimensions of this inconsistency in emotions.
A multinational and multicenter study states that complex psychosocial factors influence the willingness of frontline healthcare workers to receive the COVID-19 vaccine (23). In fact, despite having sufficient knowledge and information about vaccines, medical workers were doubtful and had mixed feelings about accepting or not accepting the vaccine. Previous studies also showed that there is no correlation between the level of knowledge about the COVID-19 vaccine and acceptance of the vaccine (24-26). In the present study, medical staff were not fully confident about the vaccine, and this factor produced uncertainty in decision-making.
Of course, throughout history, there has been a lack of trust in health authorities regarding vaccines such as AIDS, polio, and influenza (23, 26). Other studies have mentioned concerns about safety and efficacy, side effects, mistrust of government and institutions, waiting for more information to be released, and feelings of violation of personal rights as reasons for vaccine hesitancy (27-29).
The most important point in accepting the vaccine is its approval. A study conducted in Iran also indicated that 60 percent of healthcare workers were willing to get a vaccine (30). The results of a study conducted in Saudi Arabia reported that about half of the participants wanted to receive the vaccine immediately, and the rest wanted to delay vaccination until the final approval of the vaccine. This study calls for more vaccine-related education among healthcare workers to reduce any fear that may be associated with the COVID-19 vaccine (17).
In the current study, medical staff were also skeptical about the side effects and benefits of the vaccine. A study conducted in Egypt showed that 60% of health workers did not want to receive the vaccine. Lack of immunity, fear of genetic mutation and new technology, as well as belief in the ineffectiveness of vaccines, were the main reasons for reluctance (31). On the contrary, in a study in India, health workers felt they needed vaccination to reduce the risk of transmission to their families (32). Considering that health workers were the first people to decide on vaccination, it was necessary to increase the acceptability of the vaccine by highlighting various issues about the safety and efficacy of the vaccine, preferably by a reliable source of information (33).
The next category extracted from this study was the “continuation of the fight against COVID-19” disease. The medical staff stated that they voluntarily accepted the COVID-19 vaccine due to their “response to social and professional responsibility” and “encouraging people to receive the vaccine”. A qualitative study in Iran related to the social responsibility of nurses revealed that social and professional responsibility makes people do voluntary and charitable work and do not expect rewards (34). Health care professionals must fulfill their professional, social, and personal responsibilities towards vaccination. They are responsible for maintaining the safety of patients, colleagues, and the entire legal system community. They have a moral responsibility to society to prevent the spread of the virus and to support good hygiene practices. This responsibility means a commitment to understanding, supporting, and adhering to current evidence-based standards and guidelines. If health care professionals do not have sufficient knowledge, they should seek reliable information (35).
Medical workers involved in this research strongly believe that administering the vaccine through them can facilitate public acceptance and effectively curb the spread of the coronavirus. It is widely recognized that healthcare professionals hold great influence and credibility in the domain of health. Consequently, their expertise and guidance in addressing various concerns regarding COVID-19 vaccination are highly cherished and trusted by the population.
The last category extracted was based on the experiences of health workers from the study “Getting rid of COVID-19”. They expressed one of their reasons for getting the vaccine to get rid of the coronavirus disease. They stated that by receiving the vaccine, they would like the pandemic to subside and, in addition to “returning to normal life,” it would also lead to a decrease in the death rate. Therefore, by accepting the COVID-19 vaccine, they wanted to get rid of the disease as soon as possible. Studies show that nurses and other healthcare workers were under excessive mental pressure during the COVID-19 period. They experienced anxiety, fear, insomnia, and conflict with the family, especially with concerns about contaminating family members, inability to socialize, and disease transmission (36, 37). The findings of the current study showed that healthcare workers had an appreciable interest in receiving the COVID-19 vaccine. They were trying to fulfill their personal and social responsibility by leaving aside doubts about the vaccine and playing an active role in sensitizing and encouraging society to vaccination so that life can return to normal after getting rid of the COVID-19 epidemic.
5.1. Study Limitations
Caution in generalizability is one of the limitations of the results of all qualitative studies. The findings of the present study may be applicable in a setting similar to our context.
5.2. Conclusions
The medical staff believed that they would like to receive the COVID-19 vaccine in order to continue fighting the disease and get rid of it, but they had conflicting feelings about receiving it. The perceptions of healthcare workers regarding healthcare issues hold significant value in informing the general public's understanding and acceptance of critical health matters. Their role in shaping public opinion should not be underestimated. Therefore, it is crucial for health policymakers, particularly in the context of epidemics and infectious diseases, to prioritize creating both scientific and psychological environments that foster acceptance among healthcare workers. By doing so, these workers can serve as reliable references for the population, influencing their decision to embrace or reject important health measures.
The findings of this study hold immense potential in guiding the formulation of appropriate strategies to effectively control and mitigate infectious diseases in the future. Insights gained from understanding healthcare workers' perspectives can pave the way for targeted interventions and informed decision-making, thereby enhancing public health outcomes. By harnessing the knowledge and experiences of healthcare professionals, policymakers can identify and address the gaps in knowledge, attitudes, and behaviors that may hinder the control of infectious diseases.
Furthermore, incorporating the perspectives of healthcare workers in policy design and implementation can foster a sense of ownership and commitment among these individuals, subsequently increasing their engagement and adherence to preventive measures. This, in turn, can have a cascading effect on the general public, boosting overall compliance and reducing the spread of infectious diseases.
To truly harness the potential of healthcare workers as sources of knowledge and drivers of acceptance, it is critical to invest in their professional development, provide them with the necessary resources and support, and ensure their voices are heard in the policymaking process. By actively involving healthcare workers in decision-making, the health system can create a collaborative environment that promotes open dialogue and embraces the wealth of expertise and insights they bring.