1. Background
The infectious disease COVID-19, caused by SARS-CoV-2, emerged in late 2019 in China and rapidly escalated into a pandemic (1). The swift spread and high mortality rates associated with this infectious disease placed significant strain on healthcare systems (2). Consequently, healthcare systems encountered various challenges, including shortages of personal protective equipment (PPE), insufficient healthcare personnel, fear of contracting the disease and its potential consequences, concerns about transmitting the infection to family members, implementation of lockdown measures, and the loss of colleagues to the disease (3, 4). These factors contributed to diverse experiences among healthcare personnel.
The finding of a Chinese study on 10 emergency department nurses revealed a range of experiences, including fear of infection, heightened pressure during triage, feelings of gratitude, and expectations from managers. Notably, nurses expressed expectations for enhanced attention to humanistic care, increased staffing, and expanded education and training specific to emergency department protocols (5). Similarly, an Iranian study on 97 healthcare workers including nurses, doctors, emergency medical personnel, pharmacists, laboratory technicians, radiology technicians, and hospital managers, highlighted various experiences about the COVID-19 pandemic. These experiences encompassed working in a pandemic environment, adjustments to personal life with its attendant challenges, skill acquisition, adaptation to the demands of the pandemic, and considerations regarding mental health. The study underscored the importance of providing mental health support during pandemic conditions and emphasized the need for tailored care interventions across different stages of the pandemic to enhance individuals' coping and adaptation abilities (6). In another study conducted in the United States and Canada, involving 111 surgical residents, the COVID-19 pandemic was found to have three distinct effects: Educational, personal, and institutional. Adoption of telehealth and virtual training, increased empathy among residents, and program flexibility were the positive aspects reported by surgical residents. However, they also faced challenges such as lack of confidence in PPE, reduced patient caseloads leading to fewer training opportunities, and pandemic-induced burnout (7).
Mazandaran, as the third province of Iran, was significantly impacted by this infectious pandemic. Literature reviews have indicated that documenting experiences can offer valuable insights into various aspects of the COVID-19 pandemic, which can inform strategies for managing future pandemics. Considering the unique healthcare context of Mazandaran province compared to other regions, the present study aimed to explore the experiences of healthcare managers involved in patient care and treatment during the COVID-19 pandemic.
2. Methods
The present qualitative research study was conducted between April 2022 and August 2022 to gain profound insights into the experiences of healthcare providers and managers during the COVID-19 pandemic. This article adheres to the Consolidated Criteria for Reporting Qualitative Studies (COREQ) (8). The participants consisted of 15 hospital managers, including 2 clinical nurse supervisors, 3 matrons, and 10 chief executive officers. They were purposively selected from referral hospitals affiliated with Mazandaran University of Medical Sciences, Iran. Participants were chosen based on their experience in hospital management during the COVID-19 pandemic and their willingness to share their experiences.
Data were collected through semi-structured individual interviews and documents from treatment, food and drug, development, and human resources vice-chancellors. The interviews took place in quiet rooms within the hospitals at convenient dates and times. The interview questions were flexible, aiming to explore the hospital managers' experiences related to the research questions. The interviews commenced with general inquiries such as, "Please share your feelings and experiences from the onset of the COVID-19 pandemic," and progressed to more specific queries about challenges faced, strategies adopted, and trends observed during different peaks of the pandemic. Additional questions were posed to clarify responses and delve deeper into participants' experiences. On average, the interviews lasted for 60 minutes.
Data saturation was achieved after interviewing 15 hospital managers and assessing the documents from treatment, food and drug, development, and human resources vice-chancellors. Data saturation indicates that further data collection would not yield new information.
The present qualitative research employed the summative content analysis approach, conducted by a research team (9). Qualitative content analysis is a method used to gain a profound understanding of a phenomenon by structuring a large amount of textual data through a systematic process of interpretation (10).
To analyze the texts and documents, audiotaped interviews were transcribed verbatim initially. Then, the text and documents were meticulously examined by four expert researchers. They read them multiple times to grasp a comprehensive understanding of the statements. The unit of analysis was the text, which was divided into meaning units consisting of participants' experiences related to hospital management. The focus of the data analysis was to identify the challenges experienced and how the participants addressed them. To achieve this, the meaning units were condensed, abstracted, and labeled with codes. The researchers' perceptions of the statements and documents were coded, and the concepts mentioned were prioritized based on their frequency of occurrence. The codes were reviewed multiple times and categorized based on the similarity and relevance of the concepts. Subsequently, emerged codes were compared continuously, and similar codes were grouped and labeled as subcategories. Finally, the categories emerged as an interface to connect subcategories and serve as the main outcome of the data analysis (9).
This study received approval from the ethical committee of Mazandaran University of Medical Sciences (IR.MAZUMS.REC.1402.643). Participants were informed that they could withdraw from the study at any time. Their voices were recorded for data analysis and were deleted upon completion of the analysis. Additionally, honesty in reporting results and data confidentiality were ensured.
The four criteria of credibility, confirmability, dependability, and transferability were employed to ensure the accuracy of the qualitative study (11). Credibility was established through long-term involvement and sufficient interaction with the participants, collecting valid information, and member checking. For dependability, peer checking by two qualitative research experts was conducted to confirm the accuracy of the data analysis process. Furthermore, confirmability was established by the perspectives of the research team collaborators. The entire research process was documented and reported in detail to ensure the transferability of the results. Maximum variation was ensured in selecting participants in terms of hospital management levels and COVID-19 management experiences.
3. Results
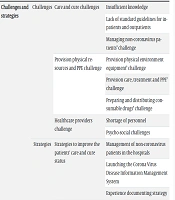
The mean ± SD of the age of participants was 48.12 ± 12.00 years. 66.6% and 33.4% of the participants were male and female, respectively. Based on the purpose of the study, exploring the experiences of healthcare providers and managers in the COVID-19 pandemic, 890 codes were extracted. The themes of “challenges and strategies” emerged in the process of reducing and abstracting the codes. It included two categories: Challenges and strategies (Table 1). The subcategories have been described as follows using direct quotations.
| Theme | Category | Subcategory | Code |
|---|---|---|---|
| Challenges and strategies | Challenges | Care and cure challenges | Insufficient knowledge |
| Lack of standard guidelines for inpatients and outpatients | |||
| Managing non-coronavirus patients’ challenge | |||
| Provision physical resources and PPE challenge | Provision physical environment equipment’ challenge | ||
| Provision care, treatment and PPE’ challenge | |||
| Preparing and distributing consumable drugs’ challenge | |||
| Healthcare providers challenge | Shortage of personnel | ||
| Psycho-social challenges | |||
| Strategies | Strategies to improve the patients' care and cure status | Management of non-coronavirus patients in the hospitals | |
| Launching the Corona Virus Disease Information Management System | |||
| Experience documenting strategy | |||
| Strategies for PPE and physical resources | Rationing of PPE and drugs | ||
| Establishment of equipment supply committees | |||
| Creativity in management of the correct use of equipment | |||
| Using the help of philanthropists | |||
| Human resource management strategies | Provision health care workers | ||
| Increasing the knowledge and ability of caring and curing the patients | |||
| Establishing mental health committee |
3.1. Challenges
The challenges category has evolved from three subcategories: "Care and Cure Challenges," "Provision of Physical Resources and PPE Challenges," and "Healthcare Providers' Challenges."
3.1.1. Care and Cure Challenges
The "Care and Cure Challenges" subcategory emerged from three codes: Insufficient knowledge, lack of standard guidelines for inpatients and outpatients, and managing non-coronavirus patients' challenges.
3.1.1.1. Insufficient Knowledge
Due to the emerging nature of the disease, there was no prior knowledge or scientific textbooks available for treating patients, which made the first peak one of the most challenging due to a lack of knowledge. A pediatrician stated, "Our hospital served as the center for children in Mazandaran province, and there was scant knowledge about the coronavirus disease, especially concerning pediatric COVID-19. On one hand, the Chinese claimed that children do not contract the coronavirus disease at all and that the risks of hospitalization and mortality are very low. Although this was somewhat true, in the early stages, we knew nothing about MIS-C (Multisystem inflammatory syndrome in children) or COVID-induced Kawasaki disease."
3.1.1.2. Lack of Standard Guidelines for Inpatients and Outpatients
At the beginning of the COVID-19 pandemic, hospital managers faced challenges such as the lack of guidelines for treating outpatients and inpatients. An infectious disease specialist said, "In the early days of the pandemic, we had no clear treatment protocols. Many instructions were implemented through trial and error. For instance, I prescribed corticosteroids while my colleague did not. It was crucial to determine when we should administer corticosteroids. In some cases, prescriptions were simply copied from one another."
3.1.1.3. Managing Non-coronavirus Patients’ Challenge
Some vulnerable groups, such as pregnant women, were affected by the increasing patient load at certain times. One of the head nurses said, "We received too many referrals of pregnant women, which posed a problem for us. Our center was not a tertiary hospital, so we transferred them to the mentioned hospitals because they were high-risk. However, the tertiary hospitals did not have empty beds to admit these patients."
The COVID-19 pandemic caused some routine care and treatment aspects of hospitals to face challenges such as the lack or delay of medical services for non-coronavirus patients, for various reasons. One of the hospital managers stated, "We did not admit vulnerable groups such as cancer patients for only a short period because we could not accept the risk of them getting infected with COVID-19 following admission to receive chemotherapy drugs." Moreover, the pandemic conditions led to a decrease in the admission of some patients. One university vice-chancellor of treatment shared his experience: "The referral rate of patients decreased significantly for two reasons: The closure of specialized clinics which were turned into respiratory clinics, and also the fear of patients going to the hospital. For example, one patient believed that because of his immune deficiency, if he went to the hospital, he would contract an infectious disease there."
3.1.2. Provision Physical Resources and PPE’ Challenge
The "Provision of Physical Resources and PPE" challenge emerged from three codes: "Provision of Physical Environment Equipment" challenge, "Providing Care, Treatment, and PPE" challenge, and "Preparing and Distributing Consumable Drugs" challenge.
3.1.2.1. Provision Physical Environment Equipment’ Challenge
Providing physical environment equipment, including physical space, ventilation systems, and hospital beds, was one of the acute challenges at that time. An executive hospital director stated, "The biggest challenge was the old structures of our hospital. For example, most of our hospitals have normal ventilation and are not equipped with negative or positive pressure isolation rooms." He further stated, "The guidelines instructed us to perform a two-layer triage, but the entrance of many hospitals is the same, requiring both respiratory and non-respiratory patients to enter through the same door. On one hand, it was not possible to perform two-layer triage effectively."
In the early days of the COVID-19 pandemic, as the number of inpatients increased, the lack of hospital beds became a major challenge for hospital managers. In this context, one of the matrons said, "We could not separate infectious from non-infectious patients. The physical space of the hospital did not allow it." Furthermore, the challenge of providing inpatient beds for both COVID and non-COVID patients arose. A surgeon explained, "The university had mandated that elective operations be canceled. Although cataract surgery is not an emergency procedure, the patient could become blind if this surgery is delayed."
3.1.2.2. Providing Care, Treatment and PPE’ Challenge
One of the challenges was providing PPE for employees, including masks, oxygen generators, ventilators, disinfectant solutions, and gowns. Due to the ambiguous nature of the pandemic, the need for PPE was also uncertain. One of the support staff said, "N95 masks were completely unavailable. Alcohol was either not available or only counterfeit versions were found in the market."
3.1.2.3. Preparing and Distributing Consumable Drugs’ Challenge
One of the food and drug vice-chancellors said, "At times, we faced severe drug shortages. For example, we had only 10 vials of Actemra! In this regard, the medicines were rare and expensive. Sometimes, even the normal saline serums were in short supply."
3.1.3. Healthcare Providers Challenge
The "Healthcare Providers' Challenges" subcategory emerged from two codes: shortage of personnel and psycho-social challenges.
3.1.3.1. Shortage of Personnel
One of the challenges that developed during the COVID-19 pandemic was the need for trained and standard personnel. One of the matrons stated, "We had to convert a 12-bed ICU into a 24-bed ICU in a short time. The increase in hospital beds required specialist nurses, and this change led to a shortage of standard staff." One of the head nurses said, "Unfortunately, during the peak of the pandemic, many key personnel such as nurses and doctors got infected, and in some cases, they died."
3.1.3.2. Psycho-social Challenges
The COVID-19 pandemic led healthcare providers to face many psycho-social challenges, including fear, anxiety, stress, feelings of crisis and war, and worry due to the lack of knowledge about the disease and its treatment, as well as fatigue, burnout, and job dissatisfaction in the first phase of the pandemic. Initially, both the community and healthcare providers experienced shock due to the rapid spread of the disease. One of the hospital managers said, "The spread of this disease both globally and nationally, coupled with insufficient awareness of its characteristics, was considered shocking." A frontline nurse expressed her anxiety, stating, "I worked in a fever clinic. My husband had diabetes, and my parents were elderly. While taking care of them, I was anxious that I might transmit the disease to them."
3.2. Strategies
The strategies category evolved from three subcategories: Strategies to Improve Patients' Care and Cure Status, Strategies for PPE and Physical Resources, and Human Resource Management Strategies.
3.2.1. Strategies to Improve the Patients' Care and Cure Status
The "Strategies to Improve Patients' Care and Cure Status" subcategory emerged from three codes: Management of non-coronavirus patients in hospitals, launching the Coronavirus Disease Information Management System, and experience documenting strategy.
3.2.1.1. Management of Non-coronavirus Patients in the Hospitals
One of the executive hospital managers said, "We designated certain departments as separate wards for admitting non-coronavirus patients, depending on their number in our hospital." He further stated, "We had a clean ward. For example, out of nine CCUs, only heart patients were admitted to four of them, while the other CCUs admitted Covid patients."
3.2.1.2. Launching the Corona Virus Disease Information Management System
According to documents from the supporting vice-chancellor, the Emergency Operations Center (EOC) began operating 24 hours a day with the telephone number 34407. Additionally, several interventions were implemented, such as setting up a response site in the pre-hospital emergency center, disseminating information to the public, training experts and students to handle calls, registering suspicious cases in the tracing system, and ensuring the presence of general practitioners and faculty members to enhance the specialized level of response.
3.2.1.3. Experience Documenting Strategy
According to documents from the treatment vice-chancellor, one of the decisions made by the managers to increase personnel awareness involved the recording and exchange of experiences through the Ministry of Health's experience registration system. This system included various details such as the names of the experience team members, the title of the experience, a summary, the knowledge area, keywords, the event or problem that led to the acquisition of the experience, a description of the experience, results of the implementation, the intended audience and users, and the applications of the experience. It also included suggestions resulting from the experience, the timeframe of the experience, and its documentation.
3.2.2. Strategies for PPE and Physical Resources
The "Strategies for PPE and Physical Resources" subcategory evolved from four codes: Rationing of PPE, establishment of equipment supply committees, creativity in managing the correct use of equipment, and utilizing the help of philanthropists.
3.2.2.1. Rationing of PPE and Drugs
Another strategy adopted by hospital managers for better equipment management was the rationing of equipment. Regarding this, one of the food and drug vice-chancellor managers said, "The personnel at the food and drug depot rationed the drugs and PPE based on the number of patients and nurses in each hospital. A representative from each hospital came daily at 18:00 to collect equipment and drugs."
3.2.2.2. Establishment of Equipment Supply Committees
The establishment of equipment supply committees also played a crucial role in managing the equipment supply challenge. One of the hospital managers said, "For the first time in Mazandaran province, we formed a ventilation committee. Initially, we had the highest number of deaths among our personnel, but such incidents almost never occurred again. One of the reasons was that we improved the ventilation status of the ICUs."
3.2.2.3. Creativity in Management of the Correct Use of Equipment
The managers also employed innovative approaches to manage oxygen consumption. In this context, one of the nursing supervisors said, "All of the patients required a high FIO2. Managing this challenge was not an easy task. Patients themselves would adjust the oxygen screw to increase the flow, believing that the louder noise from the flowmeter meant they were getting more oxygen, which gave them peace of mind. We assessed the patients carefully. If a patient did not need a reservoir bag, we switched them to a nasal cannula."
3.2.2.4. Using the Help of Philanthropists
Leveraging public participation through charities contributed to equipping hospitals. One hospital manager said, "During the first peak, we really faced an equipment shortage; our center did not have an oxygen generator, which we managed to acquire with the help and support of philanthropists." Another hospital manager added, "Charity organizations stepped in and purchased respiratory aid equipment such as ventilators and CPAP machines."
3.2.3. Human Resource Management Strategies
The "Human Resource Management Strategies" subcategory emerged from three codes: Provision of healthcare workers, increasing the knowledge and ability to care for and treat patients, and establishing a mental health committee.
3.2.3.1. Provision Health Care Workers
To manage the shortage of healthcare providers, one of the matrons said, "We utilized the operating room personnel and technicians to assist other wards because our elective operations were actually canceled. In this way, we ensured there were enough healthcare providers available." The supporting vice-chancellor manager added, "We hired workers on 89-day contracts to compensate for the shortage of healthcare providers."
3.2.3.2. Increasing the Knowledge and Ability of Caring and Curing the Patients
To enhance the knowledge and skills of healthcare providers, nursing supervisors and head nurses organized educational workshops. One of the nursing supervisors said, "I planned workshops to educate the staff about this infectious disease, its treatment, and how it is transmitted." Another nursing supervisor added, "To train the staff, we looked up instructions provided by the university and national resources. We enlisted the help of our infectious disease experts to prepare pamphlets and posters."
3.2.3.3. Establishing Mental Health Committee
Due to the high mental pressure nature of the pandemic and to address occupational burnout, a mental health committee was formed. One health manager stated, "The committee was established to rehabilitate the mental health status of healthcare providers, including those in nursing and medicine."
4. Discussion
The present study aimed to explore the experiences of healthcare providers and managers in the COVID-19 pandemic. Two main themes, "challenges" and "strategies," emerged from the interviews and documents. Healthcare providers and managers experienced unpreparedness in the first days of the pandemic. Similar to this, the results of a qualitative study in Mashad, Iran, showed the biggest problems were infrastructural challenges, including the absence of negative pressure isolation rooms and a lack of ventilation for each room (12).
The COVID-19 pandemic led to nonurgent services for non-COVID-19 patients being postponed in some countries (13). The results of a Spanish study showed the average weekly admission rate decreased by 20.8% during the COVID-19 pandemic (14). In the present study, some vulnerable groups such as pregnant women were affected following the increasing load of COVID-19 patients, and in some cases, the lack or delay of medical services for non-coronavirus patients was reported.
Shortage of physical resources including physical space, ventilation systems, and hospital beds was experienced by health managers. A similar situation was explained by other Iranian health managers. In the recent study, the lack of equipment, shortage of oxygen supply, ventilators, PPE, and delayed delivery of PPE before each shift were reported as challenges related to the shortage of physical resources at the beginning of the pandemic (12).
In the present qualitative study, the health managers said it was not possible to perform a two-layer triage in emergency rooms secondary to the old structure of hospitals. However, an Italian study reported that they followed a two-layer triage in emergency rooms. They had an isolation triage room with a nurse and admitted the identified COVID-19 patients (15). Iranian healthcare policymakers should notice this point in restructuring and designing the emergency rooms.
One of the challenges that developed during the COVID-19 pandemic was the need for trained and standard personnel that emerged following the extension of the physical environment of ICUs. The results of Ebrahimi et al.'s study in the southeast of Iran showed a deficiency of skilled healthcare providers during the COVID-19 crisis. They believed that due to the fatal nature of the pandemic, a severe shortage of hospital staff emerged (16). This challenge was also experienced in a qualitative study in the USA as redeployment. In the recent study, redeployment was experienced by nurses when they were assigned to work on another ward that had higher acuity patients or even different settings such as a pediatric ward vs. an adult ward (17).
The COVID-19 pandemic induced many psychosocial challenges. The health managers believed most healthcare providers felt fear. Fear was also experienced by healthcare providers in the study by Tabatabaee et al. (12). The results of a qualitative descriptive study in the USA revealed that healthcare providers experienced three types of stressors: Work stressors, personal life stressors, and stressors that intersect work and personal life, respectively (18).
To manage the shortage of healthcare providers, the managers at Mazandaran University hired 89-day contract workers to compensate for the shortage. Similar to this strategy, the results of a qualitative study in Alborz, Iran, revealed that they also hired 89-day contract workers to manage the shortage of human resources (19). Although, in the present study, the health managers utilized the potential capacity of some wards such as the operating room, where healthcare staff had been released due to the cancellation of elective surgeries.
Based on the Italian qualitative study, education emerged as the most prominent theme. The health managers believed they had an internal-facing obligation to train their staff (20). The results of a Chinese qualitative study showed that educational videos were a source of support in the COVID-19 pandemic because they had worked in non-infectious departments previously (21). Similarly, in the present study, clinical nursing supervisors planned some educational workshops to develop the knowledge and abilities of healthcare providers. An observational study conducted in the Netherlands on healthcare providers showed that they were satisfied with using COVID-19 app education (22).
The results of the present study revealed some challenges and strategies experienced by healthcare providers and managers at Mazandaran University of Medical Sciences. These experiences can be used to revise health-related policies. Documenting these experiences can help us manage future infectious pandemics.