1. Background
In recent decades, chronic diseases, including Parkinson's disease (PD), have increased due to improvements in health conditions, increased life expectancy, and an aging population (1). PD is a progressive neurodegenerative disease caused by the destruction of dopamine-producing neurons (2). It is the second most common disease of the central nervous system after Alzheimer's disease (3). The prevalence of this disease is rare in people under 50 years of age, with only five to 10% of diagnosed cases occurring in this age group (4). However, its prevalence increases with age, reaching 4% in individuals over 80 years old (5). In Iran, the prevalence of PD in people over 50 years is lower than in Western countries but is comparable to the prevalence reported in developing countries in Asia (6).
Currently, there is no definitive treatment for PD, and management is based on drugs and symptomatic treatments (7). It is crucial for the health system to provide services according to the community's needs (8), but there is limited information about the needs of people with PD, leading to inadequate understanding of these patients' needs (9, 10). Health care providers (HCPs) must conduct a correct and comprehensive assessment to identify and respond to patients' needs accurately. Proper assessment is necessary for allocating appropriate resources, setting goals, and formulating a care or treatment plan (11). Additionally, after evaluating the unmet needs of the patients, it is essential to prioritize the provision of services (12).
Social problems are common among PD and disrupt their lives. Physical and psychological symptoms, such as feelings of stigma, dehumanization, and loneliness, may lead patients to withdraw from social situations (13).
In a study by Rosengren et al., aimed at investigating the progression of PD and the main concerns of those affected, the data indicated that social belonging is the primary concern for PD (14). Determining what PD need is akin to assembling several puzzles simultaneously. In the study by Andrejack and Mathur, patient-centered care, support programs, access to comprehensive healthcare, and control of relevant symptoms were identified as the key components that PD in the community desire (15).
It is essential to pay attention to the social needs of PD within different cultural contexts. However, few studies have been conducted on the social needs of these patients, and most have been quantitative. Given that social needs are a complex and specific concept, quantitative studies cannot comprehensively explain these needs. A deep understanding of people's experiences with human phenomena can be obtained through qualitative research.
In this qualitative research, we seek to explore the concept of social needs or what society related to PD wants in the context of Iran, which has not been sufficiently documented, measured, or conceptualized in the literature. The research questions related to this topic remain unknown. Therefore, it is necessary to gather the opinions and experiences of patients, family caregivers, and HCPs through qualitative study to gain a deep understanding of their perspectives. Our aim is to generate insights into a complex condition like social needs, where little current evidence exists.
2. Objectives
Since no study has been conducted on the social needs of PD in Iranian society, this study aims to identify the social needs and priorities of PD from the perspectives of patients, family caregivers, and HCPs in the context of Iran.
3. Methods
3.1. Type of Research and Study Setting
This study is part of a doctoral thesis that employs a qualitative content analysis method. To identify the social needs of PD, a qualitative content analysis was conducted through semi-structured interviews between May and November 2023 in Tehran. The study setting included hospitals affiliated with Shahid Beheshti University of Medical Sciences in Tehran, which have neurology clinics. The study population consisted of: (1) all patients with PD, (2) family caregivers who live with patients, and (3) HCPs, including clinicians and nurses working in the neurology department. Based on the entry criteria, 28 participants, including 11 PD, 11 family caregivers, four nurses, and two neurologists, were selected. The inclusion criteria for the three target groups were as follows: (1) patients with PD who have been definitively diagnosed by a neurologist or movement disorder specialist, are taking anti-Parkinson drugs, have had the disease for at least six months, can communicate verbally, and live in their own homes; (2) family caregivers who have lived in the same house as the patient for at least six months continuously; and (3) HCPs with at least six months of experience caring for PD.
3.2. Sampling and Data Collection
Participants in the study were selected using a purposive sampling strategy with maximum diversity. To ensure maximum diversity, participants were chosen based on demographic characteristics such as age, sex, disease duration, disease stage according to the Hohn and Yahr criteria, education level, and different social classes. The time and place of the interviews were determined by the preferences of the participants, resulting in six interviews in the patients' homes, one interview at the university, three interviews in hospital rest rooms, two interviews in doctors' offices, one interview in a park, and 15 interviews in clinic consultation rooms.
Semi-structured, in-depth, face-to-face interviews were used to collect data. All interviews were conducted by the first author.
No one else was present except the participants and researchers, ensuring the participants' privacy during the interview. After explaining the study, its objectives, the privacy and confidentiality of personal information, the reason and method for using audio recording, and informing participants that they could stop the interview whenever they felt tired, the interviews began with general and open-ended questions such as, "Please talk about the needs and problems in society despite PD?" and "What solutions do you consider effective in dealing with these problems?" followed by, "What are your expectations from others in connection with PD?"
Questions for family caregivers, nurses, and clinicians were similarly structured but used third-person verbs, such as, "Please talk about the needs and problems that your patient/patients in the community have with PD?" If necessary, follow-up and probing questions for clarification, such as, "Could you explain more?" or "What do you mean?" were used. In addition to audio recording, the researcher also took field notes to record additional information. At the end of the interview, to ensure that the participant had expressed all their experiences, the question "Is there anything else you would like to talk about?" was asked. The interview duration ranged from 35 to 90 minutes. All patients were interviewed only once. No one refused to continue the interview, and the interviews proceeded to completion.
Next, the prioritization of identified social needs was conducted using two Delphi steps to determine priorities. Sixteen PD, fourteen family caregivers, and twenty-three HCPs from eight different disciplines (neurology, nursing, nutrition, occupational therapy, speech therapy, physical therapy, occupational therapy, and psychology) participated in this part.
In the first stage of the Delphi process, the list of patients' social needs was provided to the Delphi group members via email, social media, or a paper survey according to their preference. They were asked to evaluate the needs based on two criteria: Importance (using a five-point Likert scale) and rank (prioritizing in order). Participants were also requested to mention the reason for their preference in a sentence or paragraph and to call the contact number provided in the letter if there was any ambiguity. In the second stage, participants were allowed to compare their opinions with those of other group members. In this round, the needs were prioritized, and feedback from the first stage was provided to the participants. Again, the rating was given using a five-point Likert scale. Finally, the consensus percentage of the participants was calculated.
3.3. Data Analysis Method
Data analysis was conducted simultaneously with data collection and continued until data saturation was reached. No new data were obtained after the 25th interview, indicating data saturation. However, three additional interviews were conducted to ensure saturation. Data analysis was performed using the conventional content analysis approach based on Granheim and Lundman's five-stage model (16). Immediately after each interview, the recordings were listened to several times and transcribed verbatim using Word software. The text of each interview was read at least three times. Meaningful units were then extracted, and a code was assigned to each one. Initial coding was done by the interviewer and the main researcher (first author). Classification and checking of codes were conducted by two members of the research team. The codes were grouped into subcategories based on similarities and differences, and then main categories were extracted. A consensus on the final classification was reached by the research team. MAXQDA2020 software was used to manage the qualitative data, and a final list of social needs for PD was obtained.
3.4. Research Rigor
To ensure trustworthiness, this study was based on four criteria: Credibility, dependability, transferability, and confirmability, as presented by Guba and Lincoln in 1985 (17).
3.4.1. Credibility
A maximum variety sampling technique was used, along with several data collection methods such as field notes and review by three participants to confirm the accuracy of the extracted codes. The corresponding author examined the data to ensure the concordance of the codes with the participants' statements. Bracketing was also employed to prevent its effect on data analysis.
3.4.2. Dependability
The researchers fully documented their activities related to data collection and analysis. Codes were derived from the interpretation of the participants' experiences, with examples of how subcategories and categories were extracted, including excerpts from the interviews (by the first author). The re-coding method (by the corresponding author and fourth author) was used, and the results of the two codings were compared. Long-term engagement with the data and maintaining friendly relations with the participants were ensured throughout all stages of the research.
3.4.3. Transferability
The researchers provided a clear and purposeful description of the research process, allowing others to follow the research path and evaluate the applicability of the study data. The maximum diversity technique was used in sampling. Bracketing was also employed to prevent its effect on data analysis.
3.4.4. Confirmability
All research stages, methodologies, and decisions made during the research were clearly explained so that other researchers could follow them if necessary. All raw data, notes, documents, and recorded interviews have been preserved for future reviews.
3.5. Ethical Considerations
This study was approved by the ethical committee of Shahid Beheshti University of Medical Sciences. Ethical considerations related to the research, such as explaining the aim of the research, maintaining privacy and confidentiality of personal information, and the reason and method for using audio recording, were fully observed. Written informed consent was obtained from all participants before any data collection.
4. Results
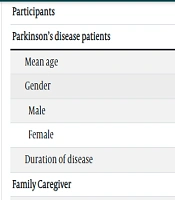
Twenty-eight participants, including 11 PD, 11 family caregivers, four nurses, and two neurologists, were included in this study (Table 1). It should be noted that patients and family caregivers were not related to each other. Primary coding of the qualitative interviews yielded 697 primary codes. From these primary codes, 12 subcategories and three main categories were extracted. Examples of codes, subcategories, and categories are provided in Table 2. The demographic characteristics of the participants in the two Delphi stages are given in Table 3. Descriptive statistical tests (mean, frequency, percentage, and weighted mean) were used to analyze the data in the first stage of the Delphi. The requirements with the highest score in each category were selected, resulting in a list of prioritized needs (Table 4). After the second stage of the Delphi, a list of patient preferences was obtained by the consensus of the participants. The social needs of PD were confirmed by 86.90% (Table 5).
| Variables and Code | Gender | Age, (y) | Marital Status | Job | Education/Relationship/Work Experience Related to PD | Duration of the Disease (y) | Stage of Disease (Hohn and Yahr) |
|---|---|---|---|---|---|---|---|
| Patients | |||||||
| 1 | Female | 60 | Divorced | Retired | Bachelor | 2 | 2 |
| 2 | Male | 64 | Married | Retired | Diploma | 4 | 1 |
| 3 | Female | 77 | Widow | Retired | High School | 14 | 5 |
| 4 | Male | 63 | Married | Retired | Bachelor | 4 | 2 |
| 5 | Male | 64 | Married | Retired | Diploma | 8 | 1 |
| 6 | Male | 70 | Widower | Jobless | Illiterate | 17 | 4 |
| 7 | Female | 62 | Divorced | Housewife | Diploma | 12 | 3 |
| 8 | Female | 75 | Married | Retired | Bachelor | 10 | 2 |
| 9 | Male | 60 | Married | Retired | Diploma | 10 | 2 |
| 10 | Male | 66 | Married | Seller | Associate degree | 17 | 2 |
| 11 | Male | 68 | Married | Armed Forces | Master | 4 | 1 |
| Family caregivers | |||||||
| 1 | Female | 38 | Married | Bachelor | Daughter | ||
| 2 | Female | 36 | Single | Diploma | Daughter | ||
| 3 | Female | 45 | Married | Master | Daughter | ||
| 4 | Female | 24 | Married | Bachelor | Daughter | ||
| 5 | Female | 75 | Married | Diploma | Spouse | ||
| 6 | Female | 45 | Single | PhD | Daughter | ||
| 7 | Female | 38 | Single | Bachelor | Daughter | ||
| 8 | Male | 42 | Married | Bachelor | Son | ||
| 9 | Female | 49 | Married | High School | Spouse | ||
| 10 | Female | 32 | Single | Bachelor | Daughter | ||
| 11 | Female | 58 | Married | Diploma | Spouse | ||
| Health care providers | |||||||
| 1 | Male | 33 | Nursing | Master | 5 | ||
| 2 | Male | 30 | Nursing | Bachelor | 4 | ||
| 3 | Male | 25 | Nursing | Bachelor | 3 | ||
| 4 | Male | 33 | Nursing | Master | 4 | ||
| 1 | Female | 36 | Physician | Neurologist | 3 | ||
| 2 | Female | 40 | Physician | Movement disorder specialist | 8 |
| Category | Interactionism by Leaving Unwanted Isolation | |||
|---|---|---|---|---|
| Subcategory | Maintaining and promoting social interactions | Maintaining aspects of the job and continuing some professional skills | Voluntary membership in groups and institutional participation | Participation in social activities |
| Code | Escape from isolation by not staying at home | |||
| Interactions with relatives | ||||
| Interactions with friends, peers, and other patients | ||||
| Reduced social bonding with forced isolation | ||||
| Participants | Values |
|---|---|
| Parkinson’s disease patients | |
| Mean age | 53.75 |
| Gender | |
| Male | 8 |
| Female | 8 |
| Duration of disease | 6.62 |
| Family caregiver | |
| Mean age | 38.07 |
| Gender | |
| Male | 8 |
| Female | 6 |
| Relative to the patient | |
| Daughter | 5 |
| Spouse | 2 |
| Son | 7 |
| HCPs | |
| Mean age | 38.47 |
| Gender | |
| Male | 10 |
| Female | 13 |
| Discipline | |
| Nurse | 8 |
| Neurologist | 4 |
| Movement disorders fellowship | 1 |
| Physiotherapist | 2 |
| Occupational therapist | 2 |
| Nutritionist | 2 |
| Social worker | 2 |
| Speech therapist | 1 |
| Psychologist | 1 |
| Variables | Parkinson’s Disease Patients and Family Caregivers | HCPs | ||||
|---|---|---|---|---|---|---|
| Needs | Priority Score | Mean | Rating Score | Priority Score | Mean | Rating Score |
| Maintaining and promoting social interactions | 157.20 | 3.93 | 40 | 35.12 | 4.39 | 8 |
| Maintaining aspects of the job and continuing some professional skills | 22.77 | 2.53 | 9 | 0 | 3.43 | 0 |
| Voluntary membership in groups and institutional participation | 3.33 | 3.33 | 1 | 0 | 3.69 | 0 |
| Participation in social activities | 25.28 | 3.16 | 8 | 99.32 | 3.82 | 26 |
| Financial support | 138.01 | 3.73 | 37 | 60.76 | 4.34 | 14 |
| Social belonging, and effective communication | 148.05 | 4.23 | 35 | 68.04 | 4.56 | 15 |
| Self-care and play efficient role | 11.04 | 2.76 | 4 | 56.96 | 3.56 | 16 |
| Comprehensive education programs for multiple target groups | 47.19 | 3.63 | 13 | 132.12 | 4.56 | 27 |
| Continued access to movement disorders specialist | 92 | 4 | 23 | 35.12 | 4.39 | 8 |
| Access to coordinated multidisciplinary services | 2.40 | 2.40 | 1 | 0 | 3.43 | 0 |
| Supporting organizations and associations | 7.06 | 3.53 | 2 | 0 | 3.69 | 0 |
| Appropriate insurance coverage | 19.80 | 3.30 | 6 | 99.32 | 3.82 | 26 |
| Variables | Social Needs | Ranking by Group | Frequency and Percentage of Agreement |
|---|---|---|---|
| PwPD and family caregivers | Maintaining and promoting social interactions | First | 28 (93.3) |
| Social belonging and effective communication | Second | 30 (100) | |
| Financial support | Third | 27 (90) | |
| HCPs | Comprehensive education programs for multiple target groups | First | 23 (100) |
| Participate in social activities | Second | 20 (86.90) | |
| Social belonging and effective communication | Third | 22 (95.65) |
Three main categories were extracted: "Interactionism by leaving unwanted isolation," "Continuity of healthcare services delivery," and "Individual-oriented and community-oriented advocacy programs," with 12 subcategories explained below.
4.1. Individual-Centered and Community-Centered Advocacy Programs
Individual-centered advocacy programs aim to respond to the health needs of PD by supporting them through empowerment, while community-centered advocacy programs address their needs by seeking to change existing care systems. This category includes the subcategories of financial support, social belonging and effective communication, promoting self-care and playing an efficient role, and comprehensive education programs targeting multiple groups.
4.1.1. Financial Support
The need for financial support to cover treatment and living expenses is one of the most important needs for patients. On one hand, patients face limited and insufficient sources of income, as it becomes difficult for them to continue their professional activities. On the other hand, the heavy costs of their treatment make them require material support. One of the nurses stated, "Most of the patients have financial problems, and as they get older, their income decreases, which exacerbates their financial issues. They have a lot of financial problems" (Nurse, Code 4).
4.1.2. Social Belonging and Effective Communication
This need is strongly felt by participants, especially patients and caregivers, who believe it is sometimes unmet. One of the caregivers remarked, "Sometimes they treat us as if we came from Mars. We are the same people. We belong to this community" (Patient, Code 7). Additionally, effective communication with others, particularly HCPs, is a significant need for patients. A family caregiver shared, "Several occupational therapists came. Physiotherapists came. Exercised him. Walked him. He didn't cooperate. He was yelling. They also said that we can't work with him. He has to ask for it himself. Then we found an occupational therapist. He came and connected with her through friendship" (Family caregiver, Code 5).
However, it is crucial to distinguish between genuine support and pity. One of the participating nurses stated, "People who have PD struggle with their bodies, but their souls remain the same. They expect to be treated like strong individuals, but people around them often pity them and look at them like children" (Nurse, Code 1).
4.1.3. Self-care and Playing an Efficient Role
In the early stages of the disease, patients' ability to self-care underwent fewer changes. However, as the disease progressed, patients expressed their inability to self-care in various ways due to the severity of their condition and the type of disabilities they experienced. Conflicts in responsibilities, inefficiency in fulfilling roles, and the loss of main roles were significant challenges for the participants. This was especially prominent in patients with motherly roles, given the cultural expectations and the importance of this role in Iranian society, which caused them considerable distress. One patient remarked, "Sometimes I feel sorry for my children. I want to do what a mother does for her children, but I can't" (Patient, Code 7). In advocacy programs aimed at promoting self-care and playing an efficient role, emphasizing abilities is crucial. A nurse noted, "Instead of focusing on the disabilities of PD, let's focus on the abilities" (Nurse, Code 4).
4.1.4. Comprehensive Education Programs for Multiple Target Groups
Comprehensive education programs are not only aimed at increasing patients' awareness but also at educating families, increasing the number and level of awareness among HCPs, raising awareness about PD at the community level, and providing a reliable and accessible source of information. HCPs consider such educational programs a priority for the social support of patients. However, patients and their family caregivers had differing opinions. Some were eager to learn and seek knowledge, while others did not feel the need for information. Most patients expressed a desire for filtered information to avoid causing them stress and anxiety. One patient mentioned, "I try to study on the internet. Sometimes my wife tells me not to study so much. I have the right to know. She says don't read so much. Sometimes you shouldn't know everything. I try to read less" (Patient, Code 11).
Due to the shortage of movement disorders specialists, it is essential for neurologists in the country to periodically participate in specialized Parkinson's training courses. One participating physician stated, "The ability of PD fellowships in patient management is naturally greater, and there are no PD specialist nurses in the country. In the current situation, it is better to have more specialized PD courses for the treatment staff" (Physician, Code 2).
Patients expressed their sadness about the limited knowledge of PD in society. The general public's understanding of PD is often limited to just one symptom: Hand tremors. They have even experienced stigma and disbelief due to the lack of awareness about PD. One patient said, "People think we are lying because we appear to be fine sometimes" (Patient, Code 7).
Additionally, having a reliable and accessible source of information is a significant demand of patients and their families. Considering the vast reach of internet networks, this source is seen as the primary resource for patients and their families. However, the unreliability of some internet pages is a concern for PD. One patient mentioned, "I read a lot on the internet. The internet is good; it has all the information available, but I don't think it is very reliable. Some sites are not clear about where they get their content" (Patient, Code 9).
4.2. Continuity of Healthcare Services Delivery
Participants reported the need to access various healthcare services, which was associated with numerous challenges. The problems of accessing services and ensuring their continuity were identified as a critical care need for PD in the community. This category includes subcategories such as continuous communication with movement disorder specialists, access to coordinated multidisciplinary services, access to supporting organizations and associations, and appropriate insurance coverage.
4.2.1. Continued Access to Movement Disorders Specialists
Some patients expressed the need for access to a movement disorders specialist. One patient noted, "My doctor is a neurologist, and Parkinson's is just one of his branches. It would be better if it was a specialist" (Patient, Code 4). This need arises because there are few movement disorder specialists in Iran, making it difficult for patients to access them. More importantly, continuous communication with a specific neurologist is crucial, as the physician needs to monitor the patient over several months to determine the appropriate medication regimen.
4.2.2. Access to Coordinated Multidisciplinary Services
Access to rehabilitation services such as occupational therapy, physiotherapy, speech therapy, psychology, and nutritional counseling is another essential need for these patients. Coordination between multidisciplinary services is vital, and the role of a PD specialist nurse in this field is undeniable, though such a role does not exist in Iran. One participating physician stated, "PD nurses must be in the center for various reasons. One person cannot meet all the patient's needs. I can't teach exercise or medicine; a movement disorders nurse plays a very important role in clinics" (Physician, Code 2).
4.2.3. Supporting Organizations and Associations
Patients expect access to supporting organizations and associations, but they often do not receive proper support or are unaware of such organizations' existence. One family caregiver said, "There should be a place specifically for Parkinson's that has everything, for example, a physiotherapist, even a pharmacy with medicines. You can go and get everything you need and come out" (Patient, Code 8). Another patient pointed out economic problems as the cause of insufficient support: "I am also a member of the association. The association is nice, but what can they do? They don't have many facilities either. They have financial problems. No one is helping them" (Patient, Code 7). It is worth noting that the PD Association in Iran is a new non-governmental organization managed through donor support.
4.2.4. Appropriate Insurance Coverage
Adequate support from insurance companies is another critical need for these patients. Parkinson's medications are expensive, and given the economic conditions of many individuals, these drugs need to be covered by insurance. One patient said, "If there is insurance and a place where I can get my medicine, it will be very good" (Patient, Code 6). One of the participating doctors suggested, "If PD becomes one of the special diseases, the initial cost will be high, but currently, more costs are being imposed indirectly. Many patients have modest expectations. They just want their medicines to be available and their costs to be lower. That's all they want. They are not demanding patients" (Physician, Code 2).
4.3. Interactionism by Leaving Unwanted Isolation
The nature of PD affects the social interactions of PD. According to patients and their caregivers, social interaction is one of their most important social needs and a serious concern. Isolation has led to worsening physical and psychological symptoms. This category includes maintaining and promoting social interactions, maintaining aspects of their job and continuing professional skills, voluntary membership in groups and institutional participation, and participation in social activities.
4.3.1. Maintaining and Promoting Social Interactions
Social interactions through communication with friends, peers, and relatives are a major concern and need for the majority of participants, frequently mentioned in their statements. This desire for interaction arises even contrary to the patients' past personality traits. The wife of one patient noted, "Before his disease, he didn't go everywhere he was invited, but now that he's sick, he wants to go. They used to invite him, but he didn't go" (Family caregiver, Code 5). Communication with friends is so important to patients that they are satisfied despite physical discomfort. One patient said, "I was happy. I want to go out with my friend. I'm having fun. I was in pain there, but overall it was very good for me" (Patient, Code 7). The beneficial effects of socializing with relatives even made one patient forget about the disease, "If I was with my sister or the rest of our family, I can't even remember the illness" (Patient, Code 7).
Movement problems, lack of time for children, economic difficulties, the presence of stairs and physical barriers to leaving the house, the restrictions of the COVID-19 pandemic, feelings of shame and perceived shame, and being a burden on caregivers all lead patients to unwanted isolation, causing significant distress. "He hasn't left the house for six months. He says that no one has the right to come to our house. He doesn't want anyone to see him. He doesn't like to be seen by anyone. He runs away from people" (Family caregiver, Code 11).
4.3.2. Maintaining Aspects of the Job and Continuing Professional Skills
Maintaining aspects of the job and professional skills serves not only to maintain income for patients but also as a means to better control the symptoms of PD. One patient said, "For example, when you are at work, you don't think extra. You feel better. But unemployment makes you stressed" (Patient, Code 2). The wife of another patient spoke about his strong insistence on going to work: "He was in a good mood to keep going. He could hardly go to the bazaar where he works with a cane" (Family caregiver, Code 5).
4.3.3. Voluntary Membership in Groups and Institutional Participation
Participating in various groups and institutions is another activity that participants acknowledged. One caregiver mentioned, "He likes to go out. My dad is a member of the NA association. He has quit drugs for 18 - 19 years. Then I take him to the meeting. His mood improves. He says that only NA gives him hope. It gives him very good energy" (Family caregiver, Code 10).
4.3.4. Participation in Social Activities
One physician stated: "Another important point is why are they so isolated? Because their mobility is impaired, they cannot go out of the house; they are isolated in homes or care centers for the elderly. Isolating them can be very difficult. It can make their illness worse. They should be involved in the activities of society and be present as much as possible" (Physician, Code 1).
5. Discussion
This study identifies the social needs of PD from the perspective of patients, family caregivers, and HCPs, and the priority needs will be discussed in this section.
Getting out of unwanted isolation by maintaining and promoting social interactions with others is seen as a serious concern and priority for these patients. According to the present research, in the qualitative study by Sjodahl Hammarlund et al., compromised social participation is considered a key need for PD, with subclasses of limited ability to meet others, feelings of social isolation, social embarrassment, and speech problems (18). This could be due in part to conducting part of this study during the COVID-19 pandemic restrictions. Interaction in any form is the missing link for PD. The results of the study by Subramanian et al. also emphasize the need to maintain the social connection of PD and prevent loneliness during the COVID-19 pandemic despite social distancing (19). They believe that the limitations of the COVID-19 pandemic and their isolation worsened their physical and psychological symptoms, which is consistent with other studies.
In the study by Luis-Martinez et al., 12 patients with mild to moderate PD were evaluated in March 2020 before and after two months of isolation as part of a clinical study due to the pandemic. After two months of isolation, a moderate deterioration in the balance system test, an increase in the risk of falling, and an increase in body weight as a result of long-term immobility were among the findings of this study (20). PD impairs social functioning, and since satisfaction with social role functioning is related to overall happiness and quality of life, reduced social participation is a risk factor for depression, cognitive decline, increased healthcare costs, and patient mortality (21). Therefore, it is necessary to pay special attention to the symptoms related to the reduction of social interactions.
In this study, social belonging and effective communication from family and healthcare providers (HCPs) are among the priorities of patients' social needs. Consistent with the present study, Sjodahl Hammarlund et al. found that patients desire to increase social belonging (18). Additionally, Rosengren et al. identified social belonging as the main concern for achieving life satisfaction when adapting to PD (14). Previous studies show the significant impact of social support on the physical, mental, and social health of patients with PD, reducing levels of depression, anxiety, and stress (22-24). Social support not only increases participation in physical activities (25) but also improves the psychological quality of life for patients (26).
Financial issues, as one of the biggest problems for patients, can create substantial challenges for them and their families. For example, financial problems are the main cause of patients' medication non-adherence, and the negative effects are well documented (27). Poor medication adherence exacerbates symptoms, accelerates disease progression, decreases quality of life, increases hospitalization duration, leads to more hospitalizations, and raises healthcare costs (28, 29). Additionally, financial obstacles are the primary barrier to accessing healthcare services and limit the use of rehabilitation services for patients with PD (30).
In this study, the priority identified by HCPs is the need for comprehensive education programs targeting multiple groups with reliable and accessible information sources. Comprehensive education programs should address the needs of patients, caregivers, HCPs, and the general public. For instance, there is a need for movement disorder specialist nurses in Iran who can play a critical role, particularly in providing coordinated services.
Due to the shortage of nurses and the challenge of training specialist nurses in the country, it is possible to address this issue by offering specialized Parkinson's courses. Moreover, public awareness of PD should not be limited to recognizing hand tremors as a normal sign of aging. Necessary measures should be taken, especially in public and virtual media, to raise awareness. The importance of this issue is highlighted in the study by Khalil et al., which, with the consensus of the International Parkinson Group and the Middle East Association of Movement Disorders, reached eight principles, including the need for educational programs and increasing awareness among the general population and HCPs (31).
Studies from other countries have shown an increase in the annual access rate of people with Parkinson's disease (PD) to health systems (32). However, the results of the present study indicate that accessing various health services remains difficult for PD in Iran, even in Tehran, where patients receive the most services, particularly from movement disorder specialists. Patients in smaller cities face even more significant challenges. In line with the present study, Singh et al. identified access issues to healthcare in rural PD communities (33). Those dissatisfied with their access to services often face worse health conditions (34). For instance, living in rural areas is linked to poorer access to essential health services, worse health outcomes, higher emergency department visit rates, longer-term care admissions, and lower life expectancy (35).
This study identified obstacles to communication that caused ambivalence in the behavior of patients and caregivers. Some patients stopped communicating with their physicians and continued taking prescribed drugs as per their routine, while others frequently visited their physicians and changed their drug doses regularly. In Zaman et al.'s study, barriers to accessing healthcare services at both the individual and system levels were investigated. Individual-level barriers included the skills needed to search for services, the ability to participate in healthcare, transportation, and service costs. System-level barriers included inadequate distribution and non-availability of healthcare services (36).
With the implementation of the electronic prescription plan in Iran, physicians can enter only a limited number of drugs into the system each month, leading to patients not receiving enough medication. Inadequate insurance support has been mentioned as a barrier to care in PD. Various articles have stated that the lack of health insurance coverage can prevent PD from accessing essential healthcare services (37, 38). Identifying these obstacles and providing solutions to overcome them can lead to better access to healthcare services for PD.
5.1. Strengths and Limitations
Our study population was diverse in demographic characteristics, including two patients with H&Y stages 4 and 5, which is unique given the level of disability at these stages. This diversity allows us to make a valid contribution to understanding the social needs of patients with PD. Additionally, participants came from various regions of Tehran and other cities, including a participant from Minab, Bandar Abbas, far from the capital. However, one limitation was the post-COVID-19 period and quarantine restrictions, which might have influenced participants' perceptions of their social needs. Furthermore, the sampling focused on patients living in private homes. Future studies should include patients living in care centers or hospitals.
5.2. Conclusions
The results of the study indicate that people with PD experience various social needs. Neglecting any dimension of health needs can impact other areas; therefore, HCPs must adopt a holistic and interdisciplinary approach, addressing not only physical needs but also social needs based on their priorities. It is essential to consider social needs when formulating care plans. Since PD affects social interactions, both patients and their caregivers view social interactions as a crucial unmet need. Meanwhile, HCPs prioritize educating patients and families and offering specialized PD courses. Policymakers should consider implementing social support programs and provide specialized training for HCPs in the field of PD.