1. Background
Patients hospitalized in intensive care units are significantly susceptible to developing pressure injuries due to multiple risk factors (1, 2). Such injuries can cause numerous problems for patients, their family caregivers, and healthcare systems (3). With the global aging population continuously growing (4), there is an increase in the number of elderly individuals requiring hospitalization. This rise in hospitalizations has led to a higher demand for intensive care units for elderly patients (5). Numerous studies have identified old age as a primary risk factor for the development of pressure injuries, making elderly patients in intensive care units particularly vulnerable to such wounds (6, 7).
Approximately 57% to 60% of pressure injuries occur within the first two weeks of hospitalization, with 70% affecting individuals over 70 years old (8). Prolonged and severe pressure can lead to reduced blood supply, tissue ischemia, and ultimately cellular death (9). Risk factors include immobility, pressure on bony prominences at angles greater than 45 degrees, vascular obstruction, and systemic conditions such as malnutrition and reduced mobility due to fractures, paralysis, or surgery (10). Elderly individuals are particularly vulnerable due to age-related skin changes, decreased immunity, and thinning of the epidermal layer. Identifying high-risk groups for pressure injuries—such as the elderly and hospitalized patients, particularly in specialized care units—is crucial (11). These individuals require specialized healthcare services with a focus on pressure injury prevention (12).
In these cases, complementary medicine can be used as an approach to wellness. Complementary medicine encompasses a range of therapies and practices used alongside conventional medicine to promote health and well-being. These may include acupuncture, herbal medicine, massage therapy, and meditation, among others. One area where complementary medicine has gained increasing attention is in preventative care (13-15). The prevention of pressure injuries should be given special attention by healthcare providers, particularly in intensive care units, due to the unique conditions of patients hospitalized in these units and their increased contact with medical devices (16-18). One strategy for preventing these injuries is the use of preventive dressings (1, 2). Two studies found that silicone foam preventive dressings significantly reduced the risk of pressure injuries in high-risk and elderly patients (19, 20). However, accessing these dressings can be difficult and expensive in less developed countries like Iran (21). Researchers are now exploring cheaper alternatives such as olive oil, fish oil, and ChitoHeal gel, which have shown effectiveness in preventing pressure injuries and wounds (21, 22). Two natural products that have been the focus of complementary medicine are Aloe vera and honey. The use of these products in treating skin injuries has been studied extensively (23-27). Honey contains fats, amino acids, minerals, and vitamins, which contribute to its significant antimicrobial, immunomodulatory, antioxidant, and wound-healing properties (28). Honey is effective for various types of wounds, including abrasions, abscesses, amputations, bedsores, burns, abdominal wounds, fistulas, diabetes-related wounds, and perineum injuries. It stimulates the healing process, clears infections quickly, promotes tissue regeneration, and reduces inflammation (29-31). Aloe vera also has significant wound-healing properties, accelerating the movement of fibroblasts and keratinocytes to the injury site and protecting keratinocytes (24). The anti-inflammatory properties of honey and Aloe vera, along with their use as preventive dressings, can help prevent the development of pressure injuries. According to the studies conducted so far, the preventive effects of honey and Aloe vera dressings on healthy skin have not been investigated.
2. Objectives
The aim of this study was to investigate the effect of Aloe vera and honey preventive dressings on the prevention of pressure injuries in the sacral region among elderly patients hospitalized in an intensive care unit.
3. Methods
3.1. Study Design
The current study was a single-blind randomized clinical trial conducted over a period of 9 months in 2022.
3.2. Study Setting and Participants
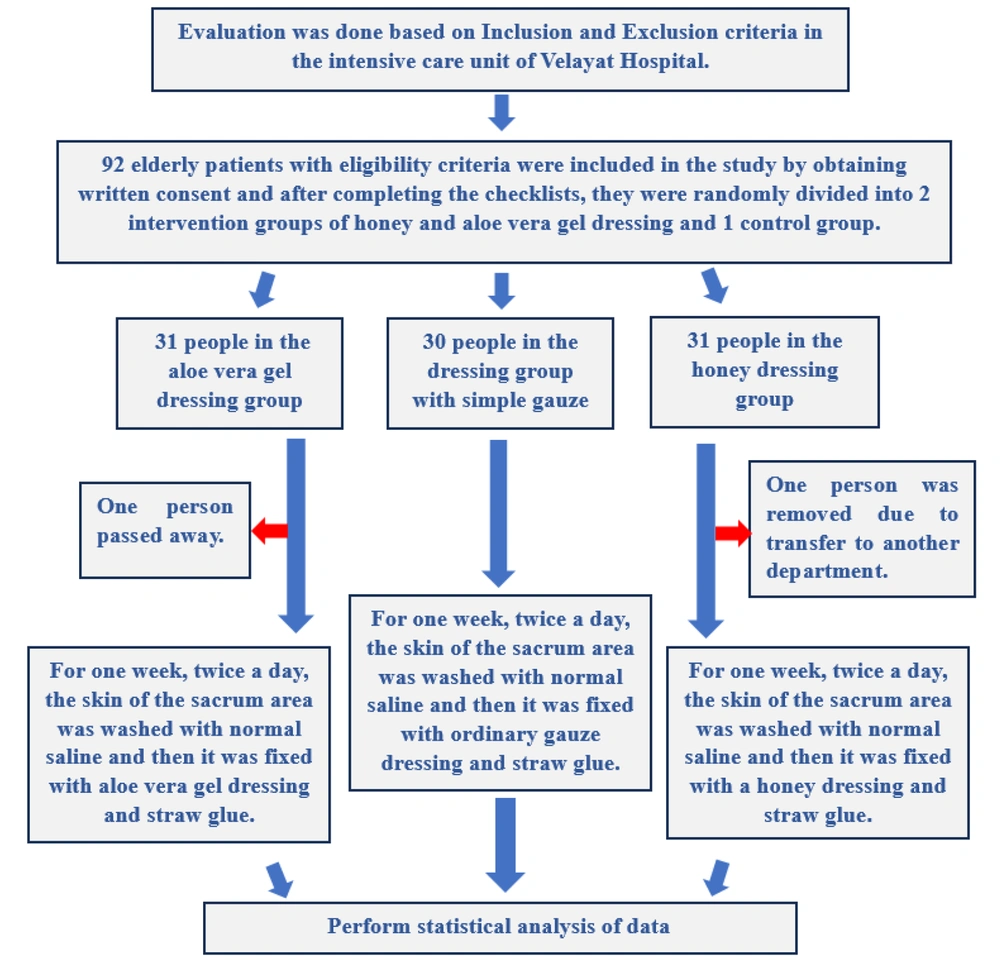
The study was conducted at Velayat Hospital, affiliated with Qazvin University of Medical Sciences. This hospital has one ICU with 14 active beds. The study population consisted of elderly patients at high risk of developing pressure injuries. Based on the results of previous studies and using the following sample size formula, 28 patients were required for each group. Accounting for a 10% attrition rate, the estimated total sample size for all three groups was 92 patients (Figure 1).
3.3. Inclusion and Exclusion Criteria
Patients included in the study were those who did not have any pressure injuries at the time of ICU admission, had a Braden scale score of 14 or below, and were aged 60 or older. Patients with absolute movement restrictions, such as those with spinal cord injuries, were excluded from the study, as were those who developed a pressure injury within the first 12 hours after ICU admission.
3.4. Data Collection and Measurement
3.4.1. Tools Used in the Study
3.4.1.1. Demographic Information
This demographic information included items related to the patient’s age, sex, weight, cause of hospitalization, smoking status, drug addiction, underlying diseases, type of nutrition in the ward (enteral or parenteral), and type of oxygenation in the ward (endotracheal tube, tracheostomy, or spontaneous breathing).
3.4.1.2. Braden Scale
The Braden Scale was used to predict the risk of developing pressure injuries. It was first introduced by Braden and Bergstrom in 1987, and its validity and reliability have been evaluated in Iran (32, 33). The scale consists of 6 risk factors: sensory perception, moisture, activity, mobility, nutrition, and friction and shear. Each of these parameters, except for abrasion force, is graded from 1 to 4, with abrasion force graded from 1 to 3. A score of 1 indicates a worse situation, while a score of 4 indicates a better situation. The final score is obtained by summing the individual scores. A lower score on this scale indicates a higher risk of developing pressure injuries.
3.4.1.3. Pressure Injury Staging System
The tool, designed in 2016 by the American Pressure Injury Association and the European Pressure Ulcer Advisory Panel, categorizes pressure injuries into six stages. These range from stage one (erythema and redness without skin paleness) to stage six (extensive tissue damage) (34).
3.5. How to Prepare Aloe Vera and Honey
The Aloe Vera gel used for patients in the Aloe Vera gel group was 100% pure and produced by Seagull Company, located in Karaj, Iran (35). Dressing application for this group was performed by one of the researchers (AF). The thyme honey was prepared by Shahbaloothoney Company (36), located in Qazvin, Iran. This honey meets the standards set by the Ministry of Health and has been verified through relevant laboratory reports. Shahbaloothoney is a reputable brand in the production of bee products, including honey, royal jelly, and pollen, as well as in the breeding of queens and bees. The company holds brand registration number 255059, an exploitation license from the Jihad Agriculture Organization under number 117762, and a health and operation permit for the workshop numbered 28/53/209747-2038-1078. Dressing for this group was also performed by one of the researchers (AF).
3.6. Study Interventions
All patients at moderate and high risk of pressure injuries were included in the study. Patients were initially evaluated at the time of admission by the research team and were included in the study if they met the inclusion criteria. Participants were selected and included in the study through random sampling using a ball and bag method, performed by a nurse who was unaware of the study groups. They were then divided into three groups using a computer randomization method (Figure 1). Before applying the preventive dressings, a sensitivity test was conducted by a nurse on the patients' forearms. After 24 hours without any complications, the dressings were applied to the sacral area. None of the patients tested positive for allergies, as the dressings were applied to healthy skin, and no complications were observed during the study. The location of the dressings is shown in Figure 2. Schematic photos were used to comply with ethical rules and due to the lack of permission to publish patient photos.
3.7. Aloe Vera Preventive Dressing Group
In this group, the skin of the sacral region was first examined by the patient's nurse and one of the researchers (AF). The skin was then cleansed with gauze impregnated with normal saline solution. After cleansing, 5 cc of aloe vera gel was applied to a simple gauze and placed on the patient's sacral region, then covered with adhesive tape. This procedure was performed twice a day (once in the morning and once in the evening). The dressing remained in place for up to 7 consecutive days.
3.8. Honey Preventive Dressing Group
In this group, the skin of the sacral region was first examined by the patient’s nurse and one of the researchers (AF). The skin was then cleansed with gauze impregnated with a normal saline solution. After cleansing, 5 cc of honey was poured onto a simple gauze and placed on the patient’s sacral region, then covered with adhesive tape. This procedure was performed twice a day (once in the morning and once in the evening). The dressing remained in place for up to 7 consecutive days.
3.9. Simple Gauze Preventive Dressing Group
In this group, the skin of the sacral region was first examined by the patient’s nurse and one of the researchers (AF). The skin was then cleansed with gauze impregnated with a normal saline solution. After cleansing, a simple gauze was placed on the patient’s sacral region and covered with adhesive tape. This procedure was performed twice a day (once in the morning and once in the evening). The dressing remained in place for up to 7 consecutive days.
3.10. Data Analysis
Mean and standard deviation, one-way ANOVA, and chi-square tests were used for data analysis. Data were analyzed using SPSS v23, and the significance level was set at less than 0.05.
3.11. Ethical Considerations
The current study was approved by the Ethics Committee of Qazvin University of Medical Sciences (IR.QUMS.REC.1397.403). The study proposal was also registered in the Iranian Clinical Trial System under the number IRCT20190326043114N1. Due to the low level of consciousness of the patients, informed consent forms were completed by the patients' family members. Participants' autonomy and confidentiality were maintained throughout the study by the researchers.
4. Results
The mean scores on the Braden Scale for patients in the aloe vera, honey, and simple dressing groups were 10.83, 10.40, and 10.30, respectively (P = 0.40). No significant differences were found in other demographic variables among the three groups (P > 0.05). Table 1 provides detailed information on the demographic variables for all three groups.
| Items | Aleo Vera Group | Honey Group | Simple Dressing Group | P-Value |
|---|---|---|---|---|
| Total Braden Score | 10.8 | 10.40 | 10.30 | 0.40 |
| Gender | 0.88 | |||
| Male | 20 | 20 | 22 | |
| Female | 10 | 10 | 8 | |
| Age | 74.7 ± 5.05 | 72.7 ± 6.8 | 73.6 ± 7.4 | 0.51 |
| Body Mass Index | 20.9 ± 1.6 | 20.9 ± 1.7 | 21.5 ± 2.3 | 0.67 |
| GCS | 10.5 ± 3.2 | 9.8 ± 3.5 | 10.1 ± 2.7 | 0.33 |
| Albumin level | 3.1 ± 0.6 | 3.2 ± 0.8 | 3.5 ± 0.8 | 0.62 |
| Hemoglobin level | 13.7 ± 2.1 | 15.2 ± 5.2 | 14.6 ± 1.4 | 0.8 |
| Respiration type | 0.09 | |||
| Spontaneous | 18 | 18 | 17 | |
| Mechanical ventilation | 12 | 12 | 13 |
a Values are expressed as mean ± SD.
Regarding the development of pressure injuries, 10 patients developed such injuries: 7 in the simple dressing group and 3 in the honey dressing group. None of the patients in the aloe vera dressing group developed pressure injuries. The Fisher exact test results indicated a statistically significant difference in the development of pressure injuries among the different groups (P < 0.05). The chi-square test results showed that the frequency distribution of pressure injuries was similar between the honey and simple gauze groups, with no statistically significant difference between them (P > 0.05) (Table 2).
| Pressure Injury Group | Yes | No | Total | Chi-square Test Result |
|---|---|---|---|---|
| Aloe vera | 0 | 30 | 30 | F Exact= 7.92; P-value = 0.01 |
| Simple dressing | 7 | 23 | 30 | |
| Total | 7 | 53 | 60 |
Additionally, the chi-square test results indicate that the frequency distribution of pressure injuries between the aloe vera and honey groups is nearly identical, with no statistically significant difference observed (P > 0.05). Clinically, it is noteworthy that no pressure injuries occurred in the aloe vera group, while there were 3 cases in the honey group and 7 in the simple gauze group.
5. Discussion
The results of this study demonstrated that the use of aloe vera preventive dressing on the sacral region significantly reduced the risk of developing pressure injuries. Honey dressing also showed some effectiveness in this study.
The literature review revealed no similar studies on the combined use of aloe vera and honey dressings for preventing pressure injuries. However, several studies have examined the effects of topical aloe vera gel for preventing pressure injuries. In the study by Hekmatpou et al., 80 patients hospitalized in the orthopedic department were divided into control and intervention groups. The intervention group used aloe vera gel twice daily for ten days. The study reported that the topical application of aloe vera gel significantly reduced the risk of pressure injuries in high-risk patients (37). Similarly, study by Falahi et al. found that topical application of aloe vera gel reduced the occurrence of pressure injuries and prevented redness at pressure points (38). Although these studies found that patients using topical aloe vera experienced fewer pressure injuries, the incidence was not zero, as observed in this study. In one study, the incidence was 5.1% (37), and in another, it was 33.3% (38). This suggests that using gauze impregnated with aloe vera gel has a more significant preventive effect compared to topical application alone.
In a study by Zanaty et al., the therapeutic effect of aloe vera gel on second-stage pressure injuries was evaluated in 60 patients admitted to intensive care units. The results showed that aloe vera gel dressing was highly effective in healing second-stage pressure injuries (39). Additionally, a study on the effects of 1% aloe vera cream on the healing of second-degree pressure injuries reported significantly positive results (39). Baghdadi et al. also found that aloe vera ointment was more effective than calendula ointment in preventing pressure injuries, with none of the patients using aloe vera dressings developing pressure injuries (27).
Although no specific studies have directly examined the preventive effect of honey on pressure injuries, existing research has explored honey’s impact on skin problems. Güneş and Eser investigated the effect of honey dressing on the treatment of pressure ulcers and found that wound healing in the intervention group was four times better than in the control group (26). Lavaf et al. found no significant difference in healing scores between honey cream and phenytoin treatments for episiotomy wounds (40). Mehrabani et al. compared honey dressing with hydrocolloid dressing for pressure ulcers and revealed similar effectiveness (41). Due to its ease of preparation, cost-effectiveness, and natural properties, honey dressing is recommended as a favorable option for pressure ulcer healing. Additionally, Zaleh Nikova and Vyhlidalova demonstrated that honey dressings promote faster wound healing, reduced wound size, and less pain intensity in non-healing wounds among elderly patients receiving home care (42). Honey’s characteristics, such as its low pH and water activity, along with its microbiological, enzymatic, and chemical stability, help prevent damage to the skin, which aligns with the results of the present study (43). Given the variations in study area, skin examined, and study duration between our research and other studies, further investigations are necessary to obtain more precise results on the effectiveness of honey in preventing pressure injuries. These studies should involve diverse populations and larger sample sizes.
Increased pressure and shear on the cell surface can damage cells and subsequently lead to pressure ulcers. Synthetic preventive dressings reduce pressure on the skin, prevent cell damage, and ultimately decrease the development of pressure injuries (44). In the current study, the use of aloe vera gel as a preventive dressing had a significant effect on preventing pressure injuries. This effectiveness can be attributed to two reasons. First, aloe vera gel possesses remarkable properties and constituents that positively affect the skin. Aloe vera is rich in vitamins, zinc, amino acids, mucopolysaccharides, and water, all of which are beneficial for maintaining the moisture and integrity of skin cells (45). Second, the application of aloe vera gel with a dressing contributed to the decreased development of pressure injuries in this study. The gauze used, in combination with aloe vera gel, like industrial dressings, helps prevent excessive pressure on the skin of the sacral region, resulting in a reduction in pressure injuries.
5.1. Study Limitations
In this study, one of the limitations was the nurses' lack of familiarity with preventive dressings. To address this, we provided necessary training to all nurses in this area. Additionally, due to time constraints imposed by the study being part of a thesis, a longer study was not feasible.
5.2. Conclusions
Preventing pressure injuries among elderly patients hospitalized in intensive care units is highly important. One of the main strategies to reduce the development of pressure injuries is the use of preventive dressings. The results of this study revealed that aloe vera preventive dressing was effective in preventing pressure injuries among elderly patients in the intensive care unit. This type of dressing is low-cost and affordable, making it more feasible for use in countries with limited financial resources. It is anticipated that the findings from this study will contribute to improved preventive care, enhance education for families of bedridden patients transitioning back home with similar conditions, and inspire innovative ideas in preventive care, ultimately leading to cost reduction. Due to the lack of similar studies, further research is highly recommended. It is also suggested to compare aloe vera dressing with industrial dressings.