1. Context
Female sexual dysfunction (FSD) includes disorders such as sexual aversion, anorgasmia, and dyspareunia, which significantly impact sexual health and quality of life (1, 2). Female sexual dysfunction is highly prevalent, affecting 40 - 60% of women, with 15 - 50% experiencing sexual dissatisfaction (3, 4). In Iran, the prevalence of FSD increases with age, from 22% in women under 20 to 75.7% in those aged 40 - 50 (5). Stigma, embarrassment, and limited access to treatment often prevent women from seeking help (6).
Female sexual dysfunction affects physical health, reproductive potential, mental well-being, and couple intimacy (3, 5). Sexual pleasure plays a significant role in promoting overall health, enhancing physical and mental well-being, and increasing feelings of happiness (3, 7). Sexual satisfaction, a fundamental human right, is a key indicator of both general and sexual health and is significantly influenced by sexual function (7-9). Dysfunction leads to decreased satisfaction, adversely impacting quality of life, self-esteem, interpersonal relationships, and mental health (4, 5, 10). Optimal sexual function enhances couple satisfaction, marital interactions, and overall health (11). Sexual function impacts personal and partner well-being, with enjoyable sexual relations benefiting social and marital relations, intimacy, and commitment (12, 13). Conversely, sexual dissatisfaction can lead to family disputes, marital conflicts, spousal animosity, infidelity, and divorce, and may correlate with higher rates of crime, sexual assault, and mental illness (6, 14-22).
Telemedicine offers numerous benefits for enhancing sexual knowledge, sexual health services, and related support. It is convenient, affordable, accessible, and confidential, overcoming geographical limitations (23-26). Sexual counseling via telemedicine integrates education on sexual health and relationships, improving attitudes, self-esteem, sexual self-confidence, body image, and marital quality of life (27-32). In contrast, traditional face-to-face counseling encounters barriers such as distance, limited access to counselors, high costs, and stigma (33, 34).
Studies indicate telemedicine's effectiveness in addressing FSD (33-36). Online mindfulness programs have significantly improved sexual function and arousal disorders (34). Telemedicine-based cognitive-behavioral therapy has been shown to enhance sexual function and reduce distress (35). Additionally, telemedicine-delivered sex therapy has increased sexual satisfaction and reduced sexual problems in couples (36). However, engagement and effectiveness vary among couples, highlighting the need for further research and meta-analytic approaches to consolidate the evidence (33, 37).
Despite telemedicine's potential to enhance women's sexual health, research on its impact on sexual satisfaction shows mixed results.
2. Objectives
This systematic review and meta-analysis aim to quantitatively evaluate the effectiveness of telemedicine interventions in improving women's sexual pleasure and fulfillment. The focus is on specific intervention components and desired outcomes, offering a clearer understanding of how telemedicine can support women's sexual well-being.
3. Evidence Acquisition
3.1. Materials and Methods
This review adheres to the PRISMA statement (38) for reporting systematic reviews, and its protocol was prospectively registered in PROSPERO under the unique identifier CRD42024538601.
3.2. Data Sources and Search Strategy
SCOPUS, Web of Science, and PubMed were comprehensively searched to identify relevant studies published in English up to January 2024 that investigated the impact of telemedicine interventions on women's sexual performance. The initial search terms included variations related to the concept of sexual health (e.g., sexual difficulty, sexual disorder, sexual problem, sexual dysfunction, sexual complaint), mobile technology (e.g., mobile apps, mobile health, smartphone, mHealth, cell phone, personal digital assistant (PDA), tablet, iPad, mobile applications, telemedicine), and outcomes (e.g., empowerment, management, satisfaction, training, education, enhancement, consultation, promotion, care, change). The terms were combined using the conjunction "AND" and the disjunction "OR," along with Medical Subject Headings (MeSH) terms. The search strategy was applied to the titles and abstracts of the retrieved studies. To ensure comprehensiveness, a manual search of reference lists from relevant articles was also conducted. Studies were included regardless of design, outcome measures, or publication type. Detailed database search strategies are provided in Appendix 1.
3.3. Inclusion Criteria
Studies were included if they met the following criteria:
1. Investigated the efficacy of telemedicine interventions for improving sexual function in women.
2. Utilized the Female Sexual Function Index (FSFI) as the primary measure of sexual function.
3. Were published in peer-reviewed scientific journals.
4. Enrolled participants who identified as cisgender women and engaged in regular sexual activity.
3.4. Exclusion Criteria
Studies were excluded based on the following criteria:
1. Were non-original research, such as books, review articles, conference papers, theoretical articles, letters to the editor, commentaries, or opinions.
2. Focused on telehealth interventions for men, gay men, or bisexual women.
3. Investigated telehealth applications unrelated to sexual dysfunction.
4. Employed non-experimental research designs.
3.5. Literature Management
Following the formulation of the search strategy and the acquisition of pertinent articles, the reference management software EndNote X5 (Thomson Reuters, New York, NY, USA) was used to consolidate all retrieved records.
3.6. Data Extraction
Two independent reviewers (S.A. and E.J.) conducted the initial screening of the retrieved articles and extracted relevant data using a standardized data extraction form developed by the researchers. Any discrepancies between the reviewers were resolved through consultation with a third reviewer (Kh. M.). The data extraction form included the following elements:
- General information: Author, study country, publication year, study design, disease type, target population, method details, and main findings.
- Sexual function assessment: Information on the instrument used to measure sexual function (e.g., FSFI version, number of items, and outcome scores).
- Telehealth intervention details: Details about the specific telemedicine intervention, including the mode of delivery (e.g., video conferencing, telephone, etc.), intervention duration, and format.
After data extraction, the information was organized into a form to facilitate data analysis and synthesis.
3.7. Primary Outcome Measures
Sexual desire, arousal, lubrication, orgasm, pain, satisfaction, and overall FSFI scores.
3.8. Article Selection Process
A comprehensive search strategy initially identified 4,174 articles from database searches. An additional 14 articles were identified by manually reviewing the reference lists of the retrieved studies. Using automated duplicate detection software (EndNote), 2,812 duplicates were removed, resulting in 1,376 unique articles for title and abstract screening. Two independent reviewers (S.A. and E.J.) screened these articles, excluding 57 that did not meet the format criteria for journal article inclusion (e.g., book chapters, conference proceedings). After applying predefined eligibility criteria, an additional 740 articles were excluded. The remaining 106 articles underwent full-text review by the same two reviewers (S.A. and E.J.). Following a thorough evaluation against the eligibility criteria and for topic relevance, 100 articles were excluded. This rigorous selection process led to the final inclusion of 6 eligible studies in this review. A detailed flowchart illustrating the article selection process is provided in Appendix 2.
3.9. Quality Assessment
Two independent reviewers (S.A. and E.J.) evaluated the methodological quality of the included studies using the Modified Jadad Scale (39). This eight-item instrument (Appendix 3) assesses key methodological components of randomized controlled trials (RCTs) that are relevant to minimizing bias and enhancing internal validity (39). Each item has a binary response (yes/no), with a score of 1 awarded for a positive response and 0 for a negative response. As a result, studies can achieve a maximum total score of 8.
We recognize the difficulty in achieving perfect scores on the Modified Jadad Scale, especially regarding blinding in non-attendance interventions for sexual health issues. Therefore, all retrieved studies were included in the analysis regardless of their total score. However, we acknowledge limitations in certain studies, such as small sample sizes and the impracticality of randomization due to specific patient characteristics (further details are provided in Appendix 3).
3.10. Meta-Analysis
To evaluate the effectiveness of telemedicine interventions for improving women's sexual performance, we employed a meta-analysis approach. Standardized mean differences (SMDs) were calculated to assess the strength of the relationships between interventions and outcomes. Standardized mean differences close to 0 indicate weak relationships, while values of 1 or greater suggest strong associations. We calculated 95% confidence intervals (CIs) to determine the precision of the effect size estimates. Overlapping CIs between studies typically indicate non-significant differences in SMDs (40).
To quantify the variability in effect sizes across studies (heterogeneity), we used Cochran's Q test and the I² statistic. According to established thresholds (41), an I² value below 25% suggests minimal heterogeneity, values between 25% and 75% indicate moderate heterogeneity, and values exceeding 75% reflect substantial heterogeneity. Given the potential for heterogeneity due to variations in sample size and outcome scores (Appendix 4 and 5), a random-effects model was employed for the meta-analysis. To assess potential publication bias, we planned to use funnel plots and Egger's test if a sufficient number of studies (typically 10 or more) were included for each outcome. Data analysis was conducted at a significance level of alpha < 0.05 using STATA software (version 14.0).
4. Results
From a total of 4,174 articles obtained from the database search, 6 articles with a combined sample size of 229 were included in the meta-analysis (33-37, 42). These studies examined the effect of telemedicine approaches on women's sexual performance using the FSFI questionnaire, which measures sexual performance in five areas and provides an overall satisfaction score. The homogeneity results for each area and the total score of the scale are detailed in Appendix 2.
The meta-analysis results indicate that telemedicine is generally effective in improving sexual desire, arousal, lubrication, orgasm, pain, satisfaction, and overall FSFI scores.
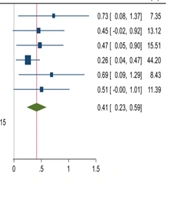
4.1. The Effects of Interventions on Sexual Desire in the Posttest
A meta-analysis of six studies involving 228 participants revealed that telemedicine interventions had a significantly stronger positive effect on sexual desire in the post-intervention period compared to the pre-intervention period (SMD = 0.92, 95% CI = 0.51, 1.32) (33-37, 42). The highest weighted effect size was from the study by Lori A. Brotto in 2021 (SMD = 1.58), and the lowest was from the study by Hummel et al. in 2017 (35) (SMD = 0.36). Based on the value of the test statistic, the difference in the results of the studies was not random and was statistically significant. The Higgins heterogeneity value was 80.5%, indicating high heterogeneity between studies in the meta-analysis (Figure 1).
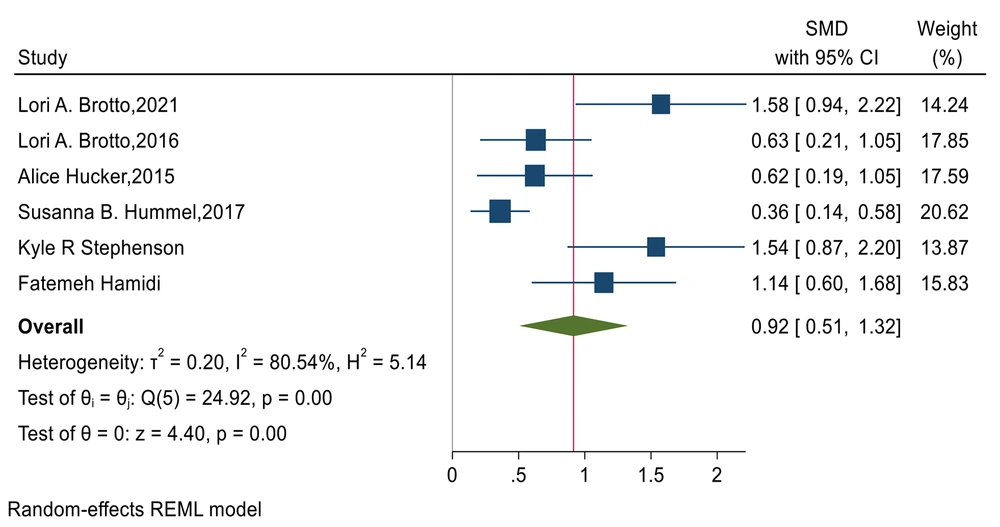
4.2. Effects of Interventions on Sexual Arousal in the Posttest
A meta-analysis of six studies involving 213 participants revealed a positive effect of telemedicine on sexual arousal compared to the level of sexual arousal before the intervention (33-37, 42). The heterogeneity value was 88.8% according to the I² calculation and Higgins classification, indicating substantial heterogeneity between the results of the studies in the posttest (SMD = 0.97, 95% CI = 0.42, 1.53) (Figure 2).
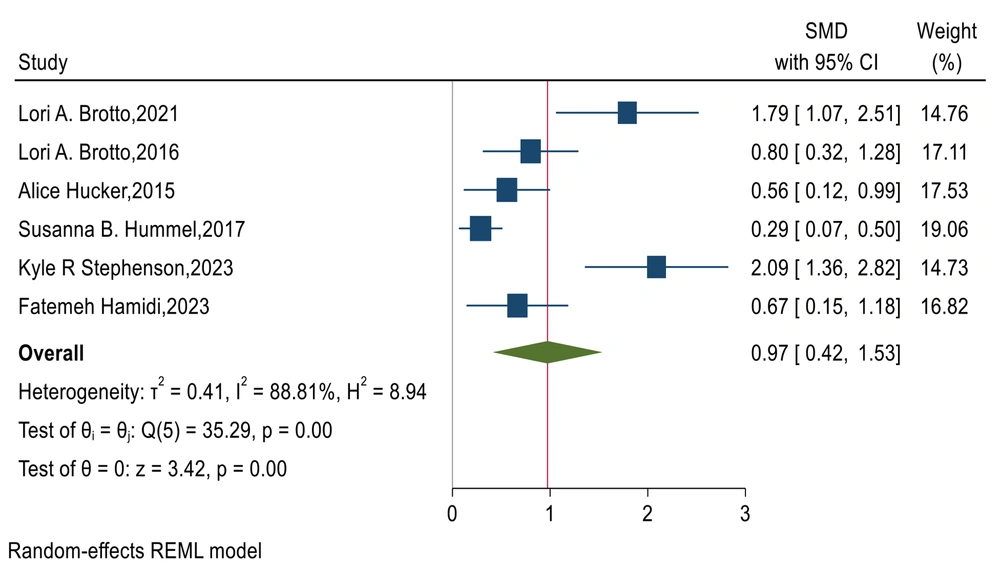
4.3. The Effects of Interventions on Vaginal Lubrication in the Posttest
A meta-analysis of six studies involving 212 participants revealed a moderate effect of telemedicine interventions on vaginal lubrication after the intervention compared to before the intervention (SMD = 0.41, 95% CI = 0.23, 0.59) (33-37, 42). According to the value of the test statistic, the difference in the results of the studies was not random and was statistically significant. The Higgins heterogeneity value was 12.72%, indicating relatively homogeneous conditions among the studies included in the meta-analysis (Figure 3).
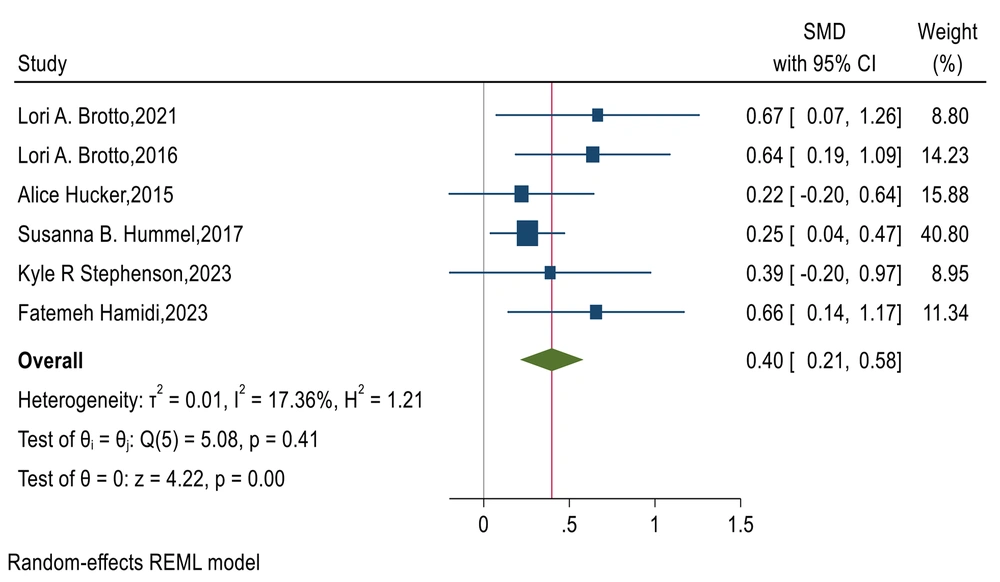
4.4. The Effects of Interventions on Orgasm in the Posttest
A meta-analysis of six studies involving 213 participants revealed an average effect of telemedicine interventions on orgasm after the intervention compared to before the intervention (33-37, 42). The heterogeneity value was 17.37% according to the Polycystic ovary syndrome calculation and Higgins classification, indicating low heterogeneity between the study results in the posttest (SMD = 0.40, 95% CI = -0.21, 0.58) (Figure 4).
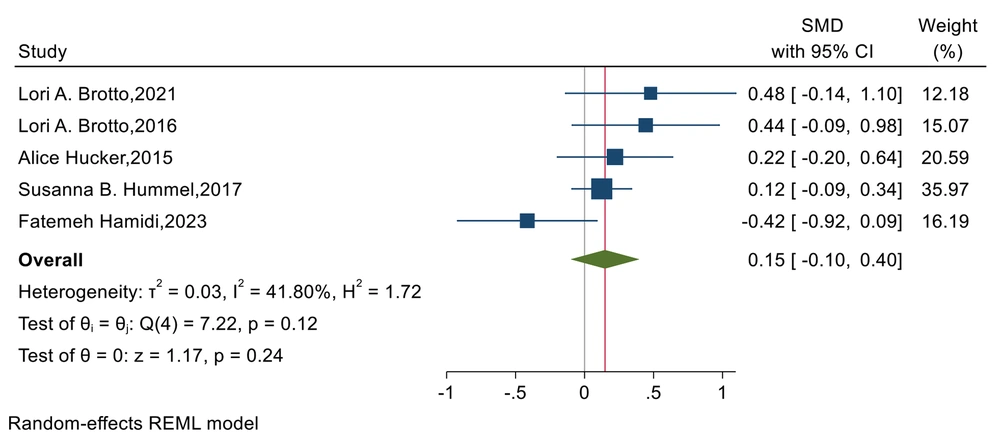
4.5. Effects of Interventions on Pain in the Posttest
A meta-analysis of five studies involving 183 participants revealed a lower effect of telemedicine interventions on pain after the intervention compared to before the intervention (33-37). The heterogeneity value was 41.80% according to the I² calculation and Higgins classification, indicating moderate heterogeneity between the results of the studies in the posttest (SMD = 0.15, 95% CI = -0.10, 0.40) (Figure 5).
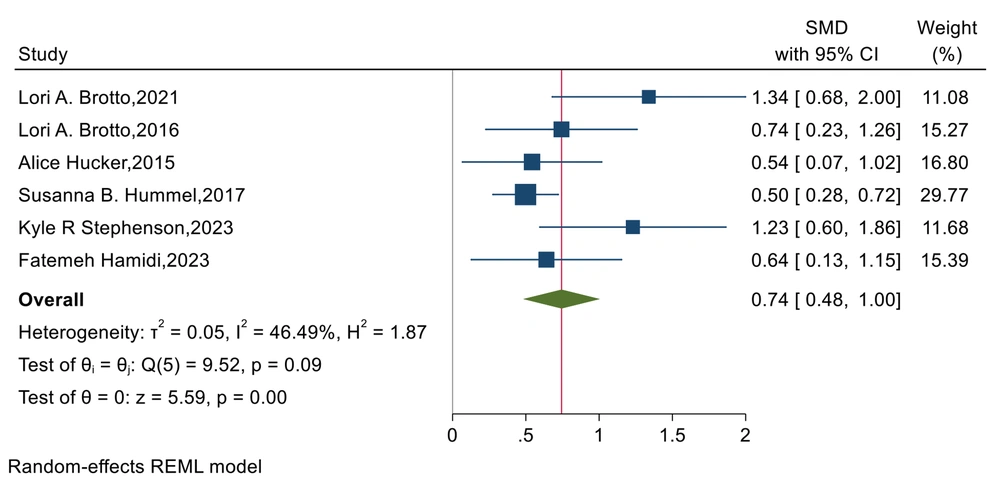
4.6. Effects of Interventions on Posttest Sexual Satisfaction
A meta-analysis of six studies involving 212 participants revealed a greater effect of telemedicine interventions on sexual satisfaction after the intervention compared to before the intervention (33-37, 42). The heterogeneity value was 46.49% according to the I² calculation and Higgins classification, indicating moderate heterogeneity between the study results in the posttest (SMD = 0.74, 95% CI = 0.48, 1) (Figure 6).
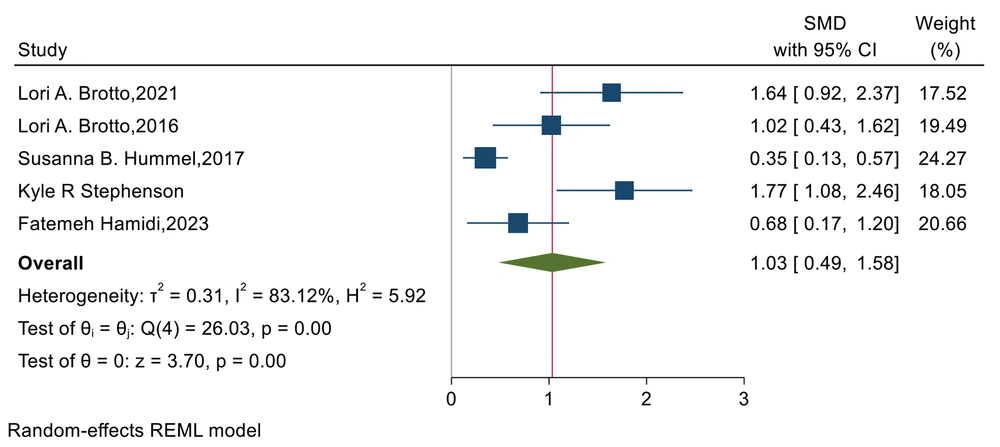
4.7. The Effects of Interventions on the Total Female Sexual Function Index Score in the Posttest
A meta-analysis of five studies involving 179 participants revealed a greater effect of telemedicine interventions on the FSFI after the intervention compared to before the intervention (SMD = 1.03, 95% CI = 0.49 to 1.58, P < 0.001). The heterogeneity value of 1.83%, according to the I² calculation and Higgins classification, indicated low heterogeneity between the study results in the posttest (Figure 7).
5. Discussion
This study assessed the effectiveness of telemedicine interventions in improving women's sexual function, as measured by the FSFI. The results indicated a statistically significant positive impact of telemedicine on sexual performance scores.
5.1. Heterogeneity and Potential Sources
The high heterogeneity observed among the included studies must be acknowledged, indicating variability in the effects of telemedicine interventions on women's sexual function across different factors. Here, we examine some potential sources contributing to this variation:
- Variations in telemedicine interventions: Differences in the design and delivery methods of telemedicine interventions may have varied among studies. Factors such as intervention format (individual vs. couple's therapy), duration, and therapist expertise could potentially influence outcomes.
- Heterogeneity in study populations: The characteristics of the women included in the studies may have differed. Variations in factors such as age, relationship status, specific sexual dysfunctions, and baseline sexual function scores (as assessed by FSFI) could account for the variability in the observed effects.
- Measurement instruments: While all studies utilized the FSFI, potential variations in how the instrument was administered or interpreted could contribute to heterogeneity.
Future research efforts should aim to standardize telemedicine interventions, thoroughly characterize study populations, and ensure consistent application of measurement tools to minimize heterogeneity and facilitate more robust comparisons across studies.
This systematic review and meta-analysis included six studies involving a total of 229 women. Of these, three studies employed a randomized controlled trial design (35-37), while the remaining three used a quasi-experimental approach (33, 34, 42). One study (37) required additional information for completeness. We contacted the corresponding author and successfully obtained the missing values for the FSFI scale dimensions.
The findings of this meta-analysis indicate that telemedicine approaches can enhance women's sexual function and overall FSFI scores (33-37, 42). These improvements are likely due to telemedicine's ability to increase women's knowledge, awareness, and positive attitudes toward sexual issues (27-32). By addressing spatial, geographical, and time limitations, as well as the lack of access to specialists and the high costs associated with face-to-face services, telemedicine interventions aim to reduce women's embarrassment and anxiety when discussing sexual problems (24-26). Such efforts are crucial for increasing women's acceptance and utilization of these services.
Research findings suggest that telemedicine is an effective approach for enhancing sexual desire, with varying impacts observed across different studies. The study conducted by Brotto et al. (34) reported the most significant impact, while the study by Hummel et al. (35) showed the least. This disparity may result from Hummel's focus on women recovering from breast cancer, who often experience body image distortions that could diminish the intervention's effect on sexual desire, despite its overall effectiveness. In contrast, Brotto and colleagues' study investigated the influence of mindfulness on women with colorectal cancer, revealing that mindfulness practices focusing on present-moment awareness and body acceptance positively affected sexual desire.
Research findings also illustrate the impact of telemedicine on sexual arousal across various studies. Some studies have highlighted that negative beliefs about sexual matters can adversely affect sexual desire in women (34). Informal counseling and training appear to positively influence women's sexual arousal by addressing and attempting to change these negative beliefs. Additionally, focusing on sexual behaviors and activities has been shown to enhance women's sexual arousal, as evidenced by several studies (34, 43, 44).
The meta-analysis indicated that the telemedicine approach has a positive, albeit moderate, effect on vaginal lubrication and the ability to reach orgasm. Many studies included in the analysis focused on women with cancer (33, 35, 37), who often experience sexual dysfunction due to factors such as PCOS, POI, hormonal imbalances, medications like sex hormone inhibitors or hormone therapy, antidepressants, body image concerns, and the impact of surgery and treatments on overall quality of life. While counseling and education may provide some benefit, the moderate impact of the intervention on vaginal lubrication and orgasm may be attributed to these underlying physical factors.
Nevertheless, the results indicated a positive but limited impact of the interventions on pain during intercourse. Brotto's study found that the intervention approach did not effectively alleviate pain during intercourse, resulting in less improvement in this domain compared to others (34). Similarly, Hucker and McCabe's study did not observe a significant reduction in pain during intercourse (36). Stephenson et al.'s study did not report specific findings on pain, which could potentially affect the overall outcomes of the meta-analysis (42). Furthermore, pain, along with issues like orgasm and vaginal lubrication, is strongly linked to physical factors (44-46).
This study demonstrates that telemedicine and online counseling significantly enhance women's sexual performance. These findings underscore the importance of leveraging modern technologies to provide counseling and educational services related to sexual health. They also highlight the necessity for further expansion and development of such services.
5.2. Limitations
This systematic review and meta-analysis have several limitations that should be considered. The relatively small number of identified studies (n = 6) restricts the generalizability of the findings. Additionally, the absence of blinding in all included studies introduces the potential for bias. Furthermore, the studies included varied in sample size, with some being relatively small. Future research could strengthen the evidence base by conducting high-quality RCTs with larger and more diverse participant groups. These RCTs should incorporate blinding procedures to minimize bias. Exploring the effectiveness of alternative interventions, such as mobile apps and other applications, alongside telemedicine approaches, would provide a more comprehensive understanding of treatment options for women's sexual health.
5.3. Conclusions
The findings of this study provide evidence supporting the use of telemedicine as a beneficial therapeutic strategy for enhancing sexual performance. Telemedicine appears to alleviate the challenges associated with face-to-face counseling and therapy. However, these studies primarily focused on specific groups facing physical challenges, such as cancer, diabetes, and kidney disease. It is important to address sexual problems and satisfaction in all couples, regardless of underlying health conditions. Therefore, further RCTs are warranted to strengthen the evidence base.