1. Background
During the postpartum period, mothers undergo significant physiological and psychological changes, necessitating physical and mental support both in hospitals and clinics as well as at home (1). Hormonal fluctuations during pregnancy, childbirth, and the irregular sleep patterns of an infant can contribute to sleep deprivation in mothers (2). Severe hormonal changes after childbirth, particularly involving progesterone, may significantly disturb mothers' sleep due to its anti-anxiety properties, its metabolites, and the loss of its sedative effect (3). During the postpartum period, 60% of women experience sleep disorders and poor sleep quality (4). Chronic sleep disorders, resulting from prolonged sleep deprivation and fragmented sleep, can exacerbate mood disorders (5). Additionally, sleep deficiency can impair memory, daily functioning, and lead to excessive fatigue and the development of mental illnesses (6). Sleep disorders are generally more prevalent in women than in men (7).
Since December 2019, the world has been severely impacted by COVID-19, a novel coronavirus first reported in Wuhan, China, leading to a global health crisis (8). In addition to the prevalence and mortality associated with this infection, measures such as social distancing and the closure of non-essential services and schools to mitigate the spread of the disease have disrupted everyday routines, social interactions, and education (9). Studies have shown that COVID-19 has led to an increase in mental disorders across various segments of society, including healthcare workers and the general population, with heightened psychological issues such as anxiety and depression. Research conducted in China, Italy, Greece, and England reveals increased symptoms of depression, anxiety, and insomnia (10, 11). Pandemic-related stressors have affected nearly everyone, with pregnant women being particularly vulnerable due to the physiological changes occurring during pregnancy (12).
The unpredictability of the coronavirus, uncertainty about when the disease will be controlled, and the severity of the associated risks have made it one of the most stressful conditions (13). Stress and anxiety during crises are inevitable (14). Furthermore, exposure to uncontrollable and unpredictable stressors can negatively impact sleep quality. Generally, as stress and anxiety increase, sleep quality worsens; conversely, improved sleep quality is associated with reduced anxiety (15). Sleep quality is a critical health indicator, reflecting how well sleep is experienced, including feeling refreshed rather than drowsy upon waking. Poor sleep quality or excessive sleepiness diminishes quality of life, raises the risk of mental illnesses, and reduces daytime functioning (16). Research indicates a relationship between COVID-19-related anxiety and sleep quality, with increased sleep disorders and decreased sleep quality observed since the pandemic began (17, 18). Moreover, several studies have identified specific mechanisms, such as increased stress and anxiety, decreased absorption, and reduced physical activity, that explain the sleep disturbances associated with COVID-19 (19, 20).
One method available to improve sleep disorders is mindfulness-based intervention (MBI), which originates from Buddhist practices that promote non-judgmental awareness of present-moment experiences (21). These interventions include educational mind-body programs designed to train the mind through meditation, helping individuals achieve a non-judgmental awareness focused on the present moment (21). This approach has proven beneficial for people with depression and other mental health disorders (20).
Before the coronavirus outbreak, human interactions were primarily physical. However, during the pandemic, social interactions largely shifted to virtual platforms. This shift has underscored the importance of developing virtual approaches for education and counseling. In times of crisis and prolonged school closures, the need for virtual and electronic education has become more pressing (20). Virtual education gained popularity due to its ability to offer flexible access to content and instruction at any time and from any location. Additionally, virtual education helped reduce the spread of the coronavirus (22).
Given the importance of maternal health, the prevention, diagnosis, and treatment of women are crucial concerns. A review of the literature in Iran revealed that mindfulness-based counseling interventions aimed at improving the sleep quality of women with a history of COVID-19 had not been conducted. Due to the significance of this issue, societal conditions, and the need for social distancing to prevent coronavirus infection, virtual interventions (online) were preferred over in-person sessions. This preference is due to their cost-effectiveness, accessibility, better time management, and potential to increase peace of mind during learning.
2. Objectives
This study was conducted to determine the impact of mindfulness-based group counseling on the sleep quality of women with a history of COVID-19 during pregnancy.
3. Methods
Using convenience sampling, the women were randomly assigned to either the intervention or control group. The mindfulness-based counseling group received eight 45-minute weekly sessions of mindfulness-based counseling over eight weeks, led by the researcher via social messenger. Data were collected using a demographic information questionnaire and the Goldberg General Health Questionnaire, administered before and after the counseling for both groups. Independent t-tests and analysis of covariance (ANCOVA) were used to compare the outcomes between the two groups.
3.1. Study Population
This two-arm randomized controlled intervention study was conducted on 100 women with a history of COVID-19 during pregnancy who were referred to the Mother's Clinic at Yahya Nejad and Ayatollah Rouhani Educational-Treatment Hospital, affiliated with Babol University of Medical Sciences, Iran, from November 2021 to February 2022. The inclusion criteria included women who were willing to participate, had a history of COVID-19 during pregnancy, were literate in reading and writing, did not have mental disabilities or deafness, had no history of mental health problems or drug addiction, were not using anti-anxiety or stress medications or alcohol, had not participated in yoga or mindfulness classes in the past six months, had given birth at the aforementioned hospitals, and scored greater than 23 and less than 60 on the GHQ-28 Questionnaire. Exclusion criteria included attendance in yoga or mind management classes in the last six months, recent bereavement, and failure to complete two or more of the eight mindfulness-based counseling sessions.
This study was a master’s thesis investigating the impact of mindfulness-based counseling on mental health in women with a history of COVID-19 during pregnancy.
3.2. Sample Size
The sample size was determined based on the mean score of mental health, referencing the study by Pan et al. (23). Considering σ1 = 6.25 (mean score of mental health), σ2 = 5.76 (with an assumed 25% improvement due to the intervention), d = 3.5, α = 0.05, β = 0.2, and power = 80%, the sample size was calculated to be 42 per group. To account for variability in mental health and potential attrition (approximately 10%), the final sample size was estimated to be 50 participants per group.
3.3. Random Sampling and Allocation
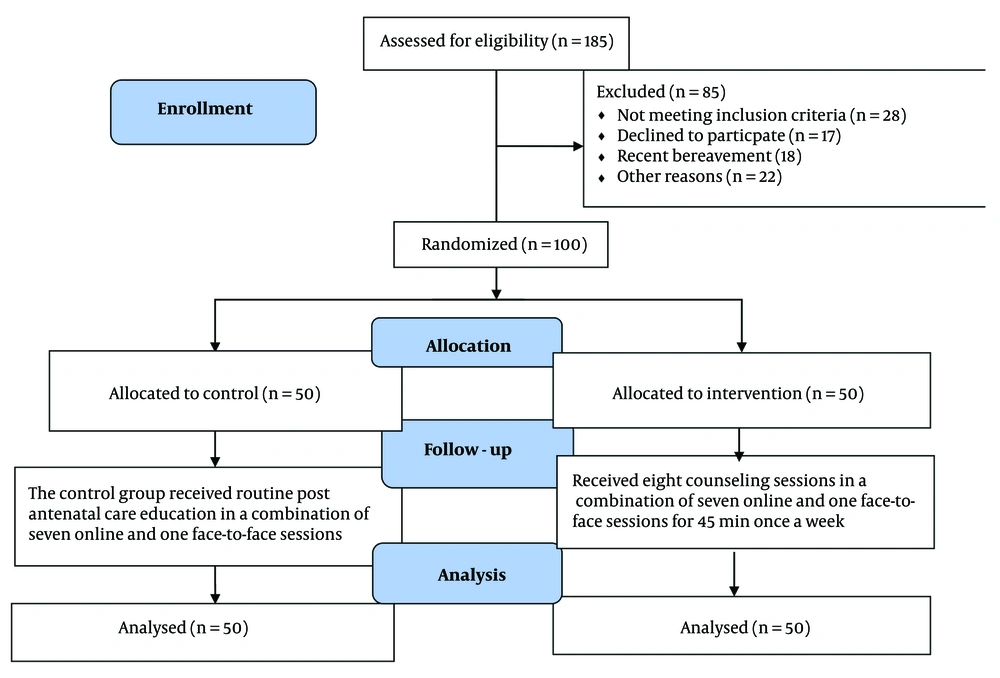
This study was conducted on women with a history of COVID-19 during pregnancy who were referred to the Mother's Clinic at Yahya Nejad and Ayatollah Rouhani Educational-Treatment Hospital, affiliated with Babol University of Medical Sciences, Iran. Sampling was carried out after obtaining approval from the Ethics Committee of the Deputy of Research and Technology at Babol University of Medical Sciences (IR.MUBABOL.REC.1400.252). The researcher, the first author who was a senior student in midwifery counseling and held a certificate in mindfulness-based counseling, attended the Deputy of Treatment at the aforementioned university. She assessed the inclusion criteria for women with a history of COVID-19 during pregnancy. Eligible women were invited to attend a face-to-face session in one of the clinic’s rooms, where the objectives and methods of the trial were fully explained. Written informed consent was obtained from those willing to participate, and they completed a demographic and obstetric characteristics questionnaire. Initially, 185 individuals were selected, but 85 withdrew from the study for personal reasons, leaving 100 participants who accepted the study conditions (Figure 1). Participants were selected using convenience sampling and were assigned to either the intervention or control group in a 1:1 ratio by blocked randomization using random allocation software with a block size of 4. Blocking was performed by a person not involved in sampling or data analysis. Treatment sequences were written on 100 cards based on the randomization list to ensure blinding, with the corresponding coding known only to the study supervisor. When an eligible participant was identified, the study supervisor informed her about the nature of the intervention. Due to the nature of the treatment modalities, blinding was not feasible, so the study employed an open-label design.
3.4. Mindfulness-Based Counseling Intervention
Based on Duncan and Bardacke's (24) work and the MBCP and MBSR programs, a mindfulness-based counseling program was developed and approved by experts in psychology and midwifery. This program consisted of eight 45-minute educational sessions.
The intervention group received eight counseling sessions, comprising seven online and one face-to-face session, each lasting 45 minutes and held once a week. Homework assigned to the mothers was reviewed by the researcher, who provided feedback to each participant. The control group did not receive any counseling during the study (Table 1).
| Topic | Sessions |
|---|---|
| Session 1: Automatic performance and overcoming obstacles | Brief description of 5 therapy sessions and the necessity and logic behind mindfulness therapy, performing meditation by eating a raisin, scanning the body for 30 minutes and discussing the emotions arising from this scan, performing a seated meditation, presenting the task of eating a raisin and body scanning and practicing mindfulness in daily activities as well as examining the obstacles to performing this exercise. |
| Session 2: Mindful breathing and staying in the moment | Gentle mindful movements to soothe somatic symptoms, 2 minutes of non-judgmental seeing and hearing practice, seated meditation, and breathing with attention to bodily sensations. |
| Session 3: Acceptance and allowing | Presenting and performing mindful body movements and seated meditation, presenting a mood exercise, thinking with separate perspectives with the understanding that most thoughts are not real, a 3-minute breathing space exercise, having meditation exercises, and choosing a combination of meditations based on personal preference for home practice, as well as performing a 3-minute breathing space exercise in an unpleasant event and exercising mindfulness in a new daily activity. |
| Session 4 | Reviewing the four-dimensional meditation, finding the best way for self-care, setting a plan with sufficient positive approaches, having a 3-minute breathing space, and discussing ways to deal with meditation obstacles. |
| Sessions 5 to 8 | Reviewing previous session exercises and requesting participants to apply all mindfulness techniques to reduce momentary stress and perform four-dimensional meditations |
The Content of Mindfulness-Based Counseling
3.5. Data Collection Tools
Data were collected using a demographic and obstetric characteristics form and the Pittsburgh Sleep Quality Index (PSQI) Questionnaire. The demographic and obstetric characteristics form was completed before the intervention in both groups, and the PSQI questionnaire was administered before and after the intervention.
3.6. Demographic and Obstetric Characteristics Information Form
The information form included variables such as age and education. Content and face validity were assessed to ensure the validity of the demographic and obstetric characteristics form. The form was reviewed by faculty members, and revisions were made based on their feedback.
3.7. The Pittsburgh Sleep Quality Index Questionnaire
This study used the PSQI to assess participants' sleep quality and patterns over the past month. The 18-item questionnaire evaluates seven factors: Sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction. Participants rated items from none (score of zero) to less than once a week (score of one), once or twice a week (score of two), and three or more times a week (score of three). A total score higher than 5 indicates poor sleep quality. The Cronbach's alpha coefficient for the components of the questionnaire was estimated to be 0.83, reflecting high internal consistency. The internal consistency for the Persian version was also acceptable, with a Cronbach's alpha of 0.77 (25).
3.8. Statistical Analysis
Statistical analysis was conducted using SPSS version 26. Descriptive statistics included the mean and standard deviation for quantitative data and frequency and percentage for qualitative data. Data normality was assessed using the Kolmogorov-Smirnov test. To examine differences between baseline variables, the t-test and chi-square test were used; in cases of non-normality, the Mann-Whitney U test and Fisher's exact test were employed. Analysis of covariance was utilized to analyze the effect of the intervention in the two study groups. Results were reported with a 95% confidence interval and a significance level of 0.05.
4. Results
The present study was conducted with 100 women who had a history of COVID-19 infection during pregnancy. Participants were divided into an intervention group (50 participants) and a control group (50 participants) at Babol University of Medical Sciences in 2022. Data normality was assessed using the Kolmogorov-Smirnov test. Table 2 compares the demographic characteristics of the two groups, showing no significant differences between them.
| Maternal Characteristics | Intervention Group (n = 50) | Control Group (n = 50) | P-Value |
|---|---|---|---|
| Mother's age (y) | 30.48 ± 4.36 | 29.98 ± 3.49 | 0.638 |
| Disease infection-intervention period (months) | 8.05 ± 3.24 | 8.05 ± 2.09 | 0.943 |
| Time of disease | 0.649 | ||
| First trimester | 12 (24) | 9 (18) | |
| Second trimester | 21 (42) | 23 (46) | |
| Third trimester | 17 (34) | 18 (36) | |
| Education | 0.250 | ||
| < Diploma | 19 (38) | 10 (20) | |
| ≥ Diploma | 31 (62) | 40 (80) | |
| Economic Status | 0.920 | ||
| Low | 9 (18) | 8 (16) | |
| Middle/good | 41 (82) | 42 (84) | |
| Gravida | 0.117 | ||
| ≤ 2 | 42 (84) | 45 (90) | |
| < 2 | 8 (16) | 5 (10) | |
| Parity | 0.135 | ||
| 1 | 22 (44) | 24 (48) | |
| < 1 | 28 (56) | 26 (52) | |
| Planned pregnancy | 0.444 | ||
| No | 11 (22) | 8 (16) | |
| Yes | 39 (78) | 42 (84) | |
| Job | 0.178 | ||
| Employee | 6 (12) | 8 (16) | |
| Freelancer | 5 (10) | 11 (22) | |
| Unemployed | 39 (78) | 31 (62) | |
| Hometown | 0.151 | ||
| City | 27 (54) | 34 (68) | |
| Village | 23 (46) | 16 (32) |
Baseline Characteristics of Participants a
Regarding sleep quality, the intervention group exhibited a significant decrease of 3.00 in the average score after the intervention compared to before (P < 0.001). In contrast, the control group showed a minimal change of 0.18, which was not significant (P = 0.820). Prior to the intervention, there was no significant difference in the average sleep quality scores between the intervention and control groups (P = 0.068) (Table 3).
Comparing the Mean Variable of Sleep Quality in the Two Study Groups Before and After the Intervention
Analysis of covariance was employed to compare the groups after the intervention, accounting for the effects of pre-intervention scores. This test examines whether the adjusted mean scores of the groups differ significantly, controlling for the potential effect of pre-intervention scores. Analysis of covariance provides more reliable results and enhances the validity and generalizability of the study. The test assumptions, including the equality of variances and the homogeneity of regression slopes, were confirmed using the Levene's test and the homogeneity of regression slopes test, respectively.
According to the results in Tables 3, and 4, the average sleep quality score in the intervention group was significantly lower than in the control group (F = 41.41, P < 0.001). The effectiveness of the intervention was quantified with an effect size (η2 = 0.299), indicating that 29.9% of the variance in the adjusted mean sleep quality scores was explained by the intervention. The statistical power of this analysis was reported as 0.99 (Table 4).
| Source | Type III Sum of Squares | df | Mean Square | F | P-Value | Partial Eta Squared | Observed Power |
|---|---|---|---|---|---|---|---|
| Sleep Quality; (Before Intervention) | 16.83 | 1 | 16.83 | 4.16 | 0.044 | 0.041 | 0.524 |
| Groups | 167.5 | 1 | 167.5 | 41.41 | < 0.001 | 0.299 | 1.00 |
The Results of Analysis of Covariance Comparing the Scores Before and After the Sleep Quality Variable Intervention
5. Discussion
This study was a controlled interventional or quasi-experimental (pretest-posttest) research using a random convenience sampling method to determine the effect of mindfulness-based counseling on the sleep quality of women with a history of COVID-19 during pregnancy in Babol. Data analysis shows that virtual counseling through a social messaging network (social messenger) significantly affects women's sleep quality. The study's findings are consistent with those of previous research (26-30).
Mindfulness-based therapy is founded on maintaining presence in every moment, preventing rumination, controlling daily events, recognizing automatic thought patterns through focused breathing, and achieving greater concentration and integration. It involves acknowledging and accepting thoughts without judgment, focusing on the present moment, and avoiding evaluation of thoughts as real or false, healthy or unhealthy, or important or unimportant. This approach can help reduce problematic conditions such as stress, anxiety, and recurrent depression, thereby supporting mental health. Mindfulness-based counseling assists individuals in recognizing and managing repetitive cognitive patterns related to COVID-19 that contribute to stress and emotional distress. By participating in these counseling sessions, women learn to alter and control negative attitudes and reduce engagement in distressing and self-destructive thoughts.
Sleep quality is a critical clinical construct, yet it is complex and challenging to define, as it is subjectively evaluated and cannot be precisely measured in a laboratory setting. The variables affecting sleep quality and their significance may differ among individuals. Researchers have long sought to identify the impact of various sleep timing and sleep habits on achieving desirable sleep and preventing sleep deprivation. It remains debatable which specific variables related to sleep timing significantly affect sleep quality and which have minimal or no impact. Additionally, determining the optimal bedtime and the necessary sleep duration for achieving desirable sleep quality is challenging. However, it is clear that uninterrupted sleep is crucial for overall health, regardless of timing, quality, or depth of sleep (23).
For patients with sleep quality disorders, continuous mental rumination about sleep, whether during the day or night, can lead to physical and emotional arousal. Metacognitive thoughts, such as "I shouldn't have these thoughts," can exacerbate agitation. Mindfulness-based exercises, including mindful breathing and body scanning, enhance awareness of various external and internal stimuli, such as thoughts, emotions, and physiological sensations. These exercises help individuals develop skills in attention control by focusing on specific tasks, thereby assisting them in managing their sleep time by directing attention, reviewing, and selectively focusing on internal (feelings) and external (time) signals.
During the course, women learned to alter their relationship with their experiences (thoughts, emotions, or physiological sensations) through acceptance rather than avoidance or control. Acceptance skills were developed by observing thoughts, feelings, or physiological sensations as transient psychological events rather than concrete realities. In essence, participants learned to experience physiological or emotional agitation without evaluating it.
Regarding the strengths and limitations of this study, the Pittsburgh Sleep Quality Index, which is validated and has high sensitivity and specificity, was used to assess sleep quality among postnatal women. Similar to other studies, this study had some limitations. First, due to the study's design and the simultaneous implementation with the outbreak and spread of COVID-19, the researcher had no further meetings with participants beyond the initial face-to-face session. Consequently, there was less participation, collaboration, responsiveness, and engagement during the project, leading to a relatively higher percentage of sample attrition. Another limitation was the researcher's inability to fully monitor the proper implementation of the guidelines. To achieve more accurate results and better assess women's needs, future research with a larger sample size, conducted in various areas, and incorporating innovative counseling methods with a longer follow-up period is recommended to evaluate the effectiveness of the counseling.
5.1. Conclusions
Based on the research findings, mindfulness-based counseling can improve sleep quality, and using existing social networking platforms can enhance women's sleep quality. However, further research is needed in this area.