1. Background
Preterm birth (PB), defined as delivery before 37 weeks of gestation, is a critical public health issue associated with significant morbidity in surviving infants (1, 2). The prevalence of preterm delivery in various Iranian cities ranges from 5.6% to 39.4% (3). Despite substantial improvements in the care of premature newborns over recent decades, PB remains a leading cause of neonatal morbidity (4). Preterm birth can be classified into two types: Spontaneous and iatrogenic. Spontaneous PB, the most common form, accounts for approximately 75% of cases and typically lacks a clear cause (5). Given the uncertain pathogenesis of spontaneous preterm labor, there is a growing focus on PB prediction using various factors to identify at-risk women, allowing for preventive interventions such as progesterone administration or cerclage procedures (6). Measuring cervical length is one of the most important methods for predicting PB (5, 6).
In 1990, Andersen et al. demonstrated that a cervical length below the 50th percentile at 30 weeks of pregnancy was associated with a 3.7-fold increased risk of PB. They further noted that a cervical length of less than 39 mm predicted PB before 37 weeks with 76% sensitivity and 59% specificity (7). Additionally, previous studies have reported an inverse relationship between cervical length during pregnancy and the frequency of PB (8, 9).
Ultrasound measurement of cervical length provides a precise assessment of cervical competence and should be integrated into clinical examinations (10-12). Although there is no established standard for cervical length at different gestational ages, transvaginal ultrasound (TVS) studies in large populations of women with singleton pregnancies have proposed various cervical length ranges (8, 13).
Transvaginal ultrasound measurement of cervical length in the first trimester is widely used to identify patients at risk for spontaneous PB (14). Numerous meta-analyses have shown that TVS cervical length measurement at 18 - 24 weeks of gestation is among the most robust and consistent predictors of preterm delivery in asymptomatic women with singleton pregnancies (15-18). Furthermore, several studies have indicated that serial cervical length measurements via TVS may improve the accuracy of PB prediction (19, 20).
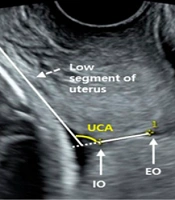
Beyond cervical length, the anterior uterocervical angle (UCA) has also emerged as a parameter for predicting spontaneous preterm labor and the likelihood of cerclage procedure failure (21-23). Uterocervical angle is defined as the angle between a hypothetical line drawn from the internal to the external cervical os and a line parallel to the lower edge of the anterior uterine wall (24). This has led to the hypothesis that an acute UCA (compared to a more open UCA) may act as anatomical support, potentially preventing cervical deformation and, consequently, PB (25). While cervical length measurement is commonly used to predict PB in high-risk pregnancies, limited studies exist on the impact of UCA on preterm delivery, leaving this area without conclusive evidence.
2. Objectives
The present study aimed to determine the role of the anterior UCA in the incidence of PB.
3. Methods
This prospective descriptive-analytic study was conducted on pregnant women who were referred to the prenatal care clinic of Yas Hospital Complex affiliated with Tehran University of Medical Sciences, Tehran, Iran, in 2021 - 2022. Inclusion criteria were primiparous pregnant Iranian women referred for the first trimester (gestational age 11 to 13 weeks) screening test. Women having multiple pregnancies, a history of abortion, and abnormalities in their fetuses, as well as being unwilling to participate, were excluded from the study. Furthermore, the sample size was calculated as 151 according to PB prevalence (11.1%) reported in a previous study (10), a confidence level of 95%, and an acceptable difference for PB prevalence (d) of 0.05. The formula used to calculate the sample size:
After assessing the pregnant women regarding inclusion and exclusion criteria, participants were selected through the convenience sampling method. The chosen women underwent a TVS device (Philips, Affinity 50, USA) with a 6 MHz probe to measure the cervical parameters: Length, Angle, and Width of the cervix. These parameters were first measured at 11 to 13 weeks, the second time at 18 - 20 weeks, and the third time at 28 - 30 weeks of gestational age. All TVS was done by one expert perinatology fellowship.
To measure the cervical length, the woman was placed in the lithotomy position with an empty bladder. The TVS probe was placed in the anterior fornix (without pressure on the cervix), and the length between the external OS triangle and V notch was measured as cervical length. The width of the cervix was measured at its midpoint. Uterocervical angle was defined as the angle between the line extending from the internal OS to the external OS and the parallel line of the lower segment of the uterus (Figure 1). The measurement was repeated three times to minimize technical errors, and the mean values obtained were used for analysis.
The mothers were followed up via phone once about two weeks after their delivery to check for any maternal or neonatal complications. The study outcomes included very preterm (defined as births between 28 weeks and < 32nd week of gestation) and late PB (defined as births between 32 weeks and < 37th week of gestation) (26).
The data collection tool was a researcher-created Questionnaire. The variables of the study were maternal age and weight, placenta location, cervical parameters measurement, gestational ages at delivery time, the neonate weight, Apgar, and NICU hospitalization.
All analyses were performed using SPSS version 24 software, with a significance level set less than 0.05. Descriptive statistics, including mean, standard deviation, absolute, and relative frequency, were used to describe the data. The data were analyzed using the chi-square test or Fisher’s exact test for correlation between qualitative variables. According to the parametric or non-parametric distribution of numeric data (which was assessed with One-Sample Kolmogorov-Smirnov Test), the Independent Samples t-test or Mann-Whitney U in comparing two, and Repeated Measures or Friedman test in more than two variables were used. Receiver Operator Characteristic (ROC) curves were used to compare second and third UCA for prediction of PB incidence.
All participants gave oral and written informed consent and cooperated in the research. No additional costs were imposed on the subjects, and their right to stop participating was guaranteed. Ethical approval of the study was obtained from the Institutional Review Board of Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1400.1022) based on the Declaration of Helsinki.
4. Results
In this study, 181 pregnant women were assessed regarding the inclusion criteria; 12 people did not meet the inclusion criteria (11 due to twin pregnancy and one due to Müllerian anomaly), and 171 women were included. During the study, 6 pregnant women were excluded from the study (2 due to Cerclage, 3 due to preeclampsia, and 1 due to legal abortion performed because of Down syndrome in the fetus). Finally, 165 were included in the final analysis.
The mean age of women was 31.45 ± 6.24 years, ranging from 18 to 44 years. Full-term delivery occurred in 153 cases (92.7%) and PB in 12 (7.3%) cases. Of women with PB, three had very PB, and nine had late PB. The demographic and pregnancy variables were compared between women with term or pre-term delivery (Table 1).
| Variables | Full-Term | Pre-term | P-Value |
|---|---|---|---|
| Age (y) | 31.52 ± 6.27 | 30.58 ± 6.09 | 0.626 |
| Weight (kg) | 71.21 ± 12.2 | 74.75 ± 7.92 | 0.090 |
| Placenta location | 0.802 | ||
| Posterior | 77 (50.3) | 5 (41.7) | |
| Anterior | 75 (49) | 7 (58.3) | |
| Fundal | 1 (0.7) | 0 | |
| Gestational hypertension | 9 (5.9) | 0 | 1.000 |
| Gestational diabetes | 16 (10.5) | 1 (8.3) | 1.000 |
| Neonatal weight (gr) | 3126.98 ± 448.97 | 2127.91 ± 687.77 | < 0.001 |
The Demographic and Pregnancy Variables Between Women with Full-Term or Pre-Term Delivery a
In both term and preterm pregnant women, during the pregnancy (11 - 13 weeks, 18 - 20 weeks, and 28 - 30 weeks of gestational age, respectively), the mean of cervical length (36.72 ± 3.44, 35.18 ± 3.88, 33.00 ± 3.92 mm) and width (17.50 ± 3.44, 16.94 ± 3.71, 16.41 ± 3.75 mm) were significantly (P < 0.001) decreased, and the mean of UCA (75.50 ± 14.00, 85.95 ± 15.13, 99.57 ± 16.68 degrees) was significantly (P < 0.001) increased.
There were no significant differences in cervical width and UCA of pregnant women with or without PB. However, cervical length in the second (P = 0.042) and third (P = 0.022) trimesters was shorter in pregnant women with PB (Table 2).
| Variables | First Trimester | Second Trimester | Third Trimester | |||
|---|---|---|---|---|---|---|
| Pre-term | Full- Term | Pre-term | Full- Term | Pre-term | Full- Term | |
| Delivery time | ||||||
| UCA | 78.33 ± 14.34 | 80.37 ± 16.08 | 90.58 ± 17.21 | 88.66 ± 16.76 | 100.25 ± 14.56 | 98.89 ± 17.78 |
| P-value | 0.797 | 0.705 | 0.705 | |||
| Cervical length | 35.25 ± 4.59 | 35.37 ± 4.15 | 32.58 ± 4.77 | 34.68 ± 3.80 | 30.00 ± 4.74 | 32.77 ± 3.88 |
| P-value | 0.774 | 0.042 | 0.022 | |||
| Cervical width | 18.91 ± 3.02 | 16.91 ± 4.93 | 18.08 ± 3.08 | 16.57 ± 4.59 | 17.08 ± 3.44 | 15.47 ± 4.5 |
| P-value | 0.051 | 0.185 | 0.356 | |||
The Trend of Cervical Parameters During Pregnancy According to the Type of Term and Pre-term Delivery a
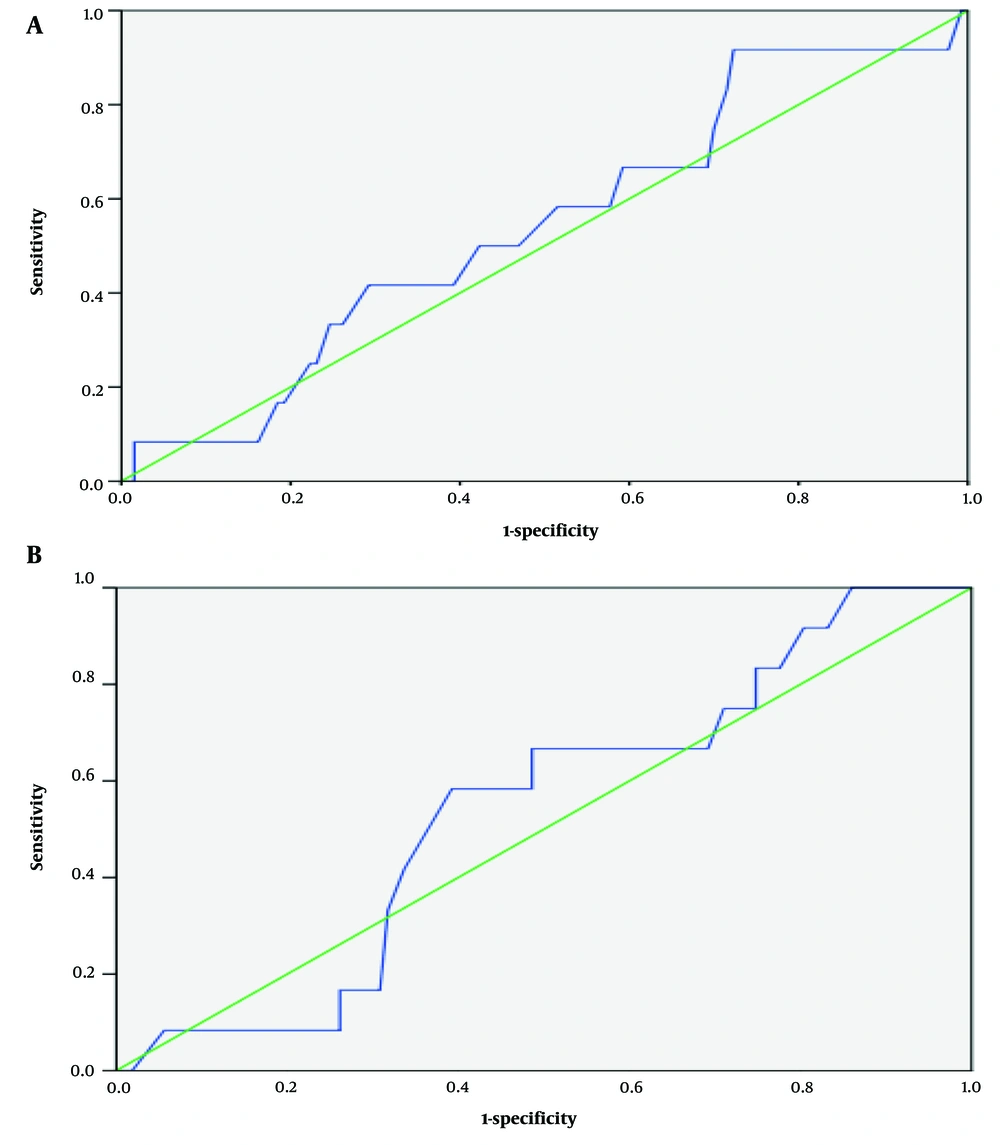
Having UCA greater than 105 in the second trimester with a sensitivity and specificity of 16.7% and 81.5%, respectively, and in the third trimester with a sensitivity and specificity of 58.3% and 60.7%, respectively, can predict PB (Table 3).
| Trimester | UCA | Preterm (n = 12) | Sensitivity | Specificity | PPV | NPV | PLR | NLR |
|---|---|---|---|---|---|---|---|---|
| 2 | > 95 | 5 (41.6) | 41.6 | 28.2 | 10.2 | 92.4 | 0.57 | 2.07 |
| 2 | > 105 | 2 (16.7) | 16.7 | 81.5 | 7.6 | 91.3 | 0.90 | 1.02 |
| 3 | > 95 | 8 (66.7) | 66.7 | 41.1 | 11.2 | 91.6 | 1.13 | 0.81 |
| 3 | > 105 | 7 (58.3) | 58.3 | 60.7 | 14.2 | 92.8 | 1.48 | 0.68 |
Sensitivity and Specificity of Uterocervical Angle in Predicting Preterm Delivery
Receiver Operator Characteristic curves were applied to compare the second and third UCAs to predict PB incidence (Figure 2). The second UCA can predict PB with an area under the curve of 0.541 (P = 0.636) compared with 0.537 (P = 0.672) for the third UCA.
5. Discussion
We performed a prospective study to examine the relationship between UCA and the occurrence of preterm delivery. The results of the present study showed that UCA increases significantly with increasing gestational age. It was also found that, based on the size of the UCA in the third trimester of pregnancy, the probability of PB can be predicted. Specifically, UCA values higher than 105 degrees were associated with a sensitivity of 58.3% and a specificity of 60.7% for identifying the risk of PB (before 37 weeks).
In addition, a systematic review of the 2004 to 2018 studies showed that UCA measurement was useful in predicting spontaneous PB before 34 weeks, and the cut-off point of this angle was 95 degrees (27). A study in New York in 2014 - 2015 reported that the anterior cervical angle of 95 degrees or greater is associated with a sensitivity of 80% for PB. An angle of 105 degrees or greater, with 81% sensitivity, is associated with PB before 34 weeks and indicates high predictive accuracy (28). However, in another study (2002), UCA size could not be confirmed as a predictor of PB due to low sensitivity and specificity. One possible reason for this difference may be the variation in anatomical factors among women of different ethnicities (21).
The present study found that the UCA size increased significantly with increasing gestational age in both preterm and term birth groups. It was also found that the LC and WC decreased during pregnancy. These findings are relatively consistent with the results of previous studies; their studies showed that the decrease in the LC reached its lowest value between the 34th and 37th weeks of pregnancy. However, no significant statistical differences were observed regarding the increase in the UCA (22, 23).
The changes in UCA during pregnancy did not differ significantly by the time of delivery, and the passage of time had no substantial effect on UCA. However, changes in the LC during pregnancy, especially in the second trimester, have been shown statistically significant in successive measurements (29).
Having a UCA of 108 degrees in pregnant women candidates for Cerclage can identify patients at risk of PB with a sensitivity of 38% and a specificity of 57% (30). Meanwhile, our study, which was done in low-risk pregnant women for PB, showed that UCA greater than 105 degrees in the second trimester with a sensitivity and specificity of 16.7 and 81.5%, and in the third trimester with a sensitivity and specificity of 58.3 and 60.7%, could predict PB. It seems the medical and obstetric history of pregnant women should be considered in using UCA for distinguishing pregnant women at risk for PB.
5.1. Limitations
The present study had some limitations. The most important limitation is the small sample size of women with PB. Another limitation was that this study was conducted only on Iranian pregnant women, and we had strict inclusion criteria for selecting participants, which reduced the external generalizability of the study. However, measurements of all cervical parameters by a single gynecologist to control inter-observer variability, along with the long follow-up of the participants, were strengths of the study.
5.2. Conclusions
Finally, the results of this research highlighted the importance of frequent measurements of cervical parameters during pregnancy. It seems UCA greater than 105 degrees in the third trimester of pregnancy can be considered a predictor of PB. Future studies are suggested to address our study's limitations and enhance the generalizability of its findings.