1. Background
Metabolic syndrome (MetS) is a cluster of metabolic abnormalities linked to an increased risk of developing type 2 diabetes (T2D) and cardiovascular disease (CVD). It is characterized by high blood sugar levels, elevated blood pressure, raised triglyceride levels, low levels of HDL cholesterol, and obesity, particularly central obesity (1). Among the various guidelines for metabolic syndrome, the national cholesterol education program (NCEP) adult treatment panel (ATP III) is the most relevant (2). Obesity is widely recognized as the primary risk factor for metabolic syndrome (3). According to the World Health Organization, global obesity rates have nearly tripled since 1975 (4). This surge in obesity has contributed to approximately 34% of adults being affected by metabolic syndrome, indicating a rising prevalence (5). An analysis of NHANES data from 2011 to 2016 revealed that 34.7% of participants met the ATP III criteria for metabolic syndrome, a significant increase compared to the 22% observed in the 1988- 1994 NHANES data (6, 7).
Obesity, particularly central obesity, has been linked to a reduced responsiveness to insulin, resulting in insulin resistance, which often leads to type 2 diabetes. Insulin resistance, along with elevated levels of insulin, glucose, and adipose cytokines, can negatively affect blood vessel function, lipid levels, and lead to conditions like high blood pressure, inflammation, and atherosclerotic cardiovascular disease (8, 9). As a result, metabolic syndrome is a crucial risk factor for both type 2 diabetes and cardiovascular diseases. Studies, including systematic reviews and meta-analyses, demonstrate the preventive and therapeutic benefits of exercise (10, 11) and leisure-time physical activity (12) in combatting major chronic diseases like metabolic syndrome. According to WHO guidelines on physical activity and sedentary behavior, the hazards of inactivity (13) and the importance of reducing sedentary behavior (14) are emphasized alongside the advantages of regular exercise. Recent research indicates that engaging in moderate to vigorous physical activity (MVPA) can lower the likelihood of developing metabolic syndrome, regardless of aerobic fitness or obesity (15-17). This type of physical activity also helps in preventing chronic diseases like type 2 diabetes and MetS (18). Additionally, a beneficial change in blood pressure indicates a link between physical activity and hypertension, as exercise impacts blood pressure and prehypertension (19). Engaging in 150 minutes of physical activity per week is associated with reduced diastolic blood pressure, increased HDL cholesterol levels, and lower overall cholesterol (20).
Dietary behaviors, defined as intentional and recurring actions influenced by social and cultural factors, play a significant role in selecting, consuming, and utilizing particular foods or diets (21). These behaviors are shaped by cultural, social, economic, and environmental influences, along with individual preferences and beliefs (22). Optimal dietary habits typically involve a balanced selection of nutrient-rich foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats. Consistent meal schedules, mindful eating practices, and proper hydration also contribute to healthy eating. On the contrary, poor dietary habits often involve excessive consumption of calorie-laden, nutritionally deficient foods rich in sugar, salt, and unhealthy fats, along with erratic eating patterns (23). Such unhealthy dietary habits are linked to a variety of health issues, including obesity, metabolic disorders, heart disease, and diabetes (24). The development and progression of metabolic syndrome involve a complex interplay of genetic and environmental factors (25), with diet being a key modifiable environmental factor (26). Research indicates that poor dietary choices contribute to the onset and worsening of metabolic syndrome (27, 28). Individuals with metabolic syndrome tend to consume high amounts of fatty and sugary foods, exhibit unhealthy eating behaviors, and have inadequate intake of vegetables. Additionally, diets high in salt, meat, fried foods, and typical Western dietary patterns are linked to an increased risk of metabolic syndrome (28, 29).
Given the rising prevalence of heart disease and diabetes in recent years, and the high prevalence of metabolic syndrome in Iran, particularly in Mazandaran province with its high rates of hypertension, hyperglycemia, and obesity, it is crucial to explore the connection between metabolic syndrome, dietary patterns, and physical activity levels among individuals enrolled in the Tabari cohort study.
2. Objectives
To reduce deaths from type 2 diabetes and heart disease, this study was conducted to determine the relationship between metabolic syndrome, physical activity, and eating habits in participants of the Tabari cohort study.
3. Methods
Data from the Tabari Cohort study (TCS) was utilized in this research. The purpose and structure of the Tabari Cohort have been described in previous publications (30). Details of the PERSIAN cohort study can also be found elsewhere (31, 32). The TCS registration period began in June 2015 and concluded in November 2017. Sampling was conducted through a census approach. Health volunteers in urban areas and medical personnel in mountainous regions recruited eligible individuals to the cohort center. Of the 12,191 qualified urban residents, 7,012 were included in the Tabari cohort. In mountainous areas, 4,417 individuals were eligible, with 3,243 being admitted into the cohort. Therefore, a total of 10,255 participants aged 35 to 70 were enrolled during the initial phase of the TCS (33).
3.1. Research Community
This study utilized data from the first cohort study of Mazandaran's urban and mountain population (the first phase took place between June 1, 2015, and November 9, 2017).
3.2. Research Sample
Sampling was based on the census method, with 10,255 adults participating in the Tabari Cohort study.
3.3. Inclusion and Exclusion Criteria
Inclusion criteria: All participants in the Tabari cohort study. Exclusion criteria: individuals with autoimmune, malignant, or endocrine diseases; those taking corticosteroids or antipsychotic drugs; pregnant and lactating women; and individuals who had taken nutritional supplements or herbal medicines in the last six months.
3.4. Data Collection
Data collection was carried out using a standardized questionnaire at the Tabari Cohort center. Information such as underlying diseases, height, weight, waist circumference, Body Mass Index, blood pressure, blood sugar, triglycerides, and HDL cholesterol were measured and recorded. Participants' eating habits were assessed using the food habit questionnaire (34), and their physical activity was measured using the Cohort Physical Activity Questionnaire. Physical activity was measured using the metabolic equivalent rates (METs) of self-reported daily activities in the PERSIAN cohort (30-32). Anthropometric measurements such as height, weight, and waist circumference were assessed following established guidelines (30, 32, 35). The height of patients was measured using the SECA 226 (SECA, Hamburg, Germany), and their weight was measured using the SECA 755 (SECA, Hamburg, Germany). All patients were asked to stand still with minimal clothing and no shoes, maintaining balance in the center of the scale until the measurement was taken. Waist circumference was measured transversely at the upper border of the iliac crest using the NIH index (30, 32). In the first step, all participants were examined for metabolic syndrome based on the ATP III criteria. The nutritional patterns and physical activity levels of individuals with metabolic syndrome were investigated using data from the Tabari cohort study, which was collected and recorded by experts using standardized questionnaires.
Metabolic Equivalent of Task Index (MET): The MET Index quantifies the energy expenditure rate during a specific physical activity relative to energy expenditure at rest, typically set at 3.5 mL/kg per minute. This index is a valuable tool for assessing physical activity levels in the general population, particularly in epidemiological studies (36). Extensive information on MET values for various activities is available in online compendiums (37).
Historically, MET was defined as a multiple of an individual's resting metabolic rate (RMR), which can be determined through gas exchange measurement, heat output assessment, or steady-state diet assessment in sedentary conditions. It can also be estimated based on age, gender, height, weight, and fitness level. In essence, 1 MET represents the ratio between the metabolic rate during activity and at rest, with 1 MET being equivalent to the energy expenditure of sitting still. Additionally, 1 MET corresponds to an oxygen consumption rate of 3.5 mL/kg/min, which is the oxygen cost of sitting quietly. Originally developed for epidemiological surveys, the MET allows participants to report the duration of specific physical activities they engage in.
3.5. Data Analysis
The data were analyzed using SPSS V.23 software. Qualitative variables were described using frequency and percentage, while quantitative variables were summarized using mean and standard deviation. Demographic and epidemiological variables were compared between two groups using the chi-square test, and quantitative variables were compared using the independent t-test. A P-value of less than 0.05 was considered statistically significant.
3.6. Ethical Considerations
This descriptive cross-sectional study was conducted with ethical approval from the research ethics committee of Mazandaran University of Medical Sciences (code: IR.MAZUMS.IMAMHOSPITAL.REC.1402.062). All participants provided written consent, were informed about the study, and were assured of confidentiality. No fees were charged to participants for their involvement in the study.
4. Results
4.1. Profile of Study Participants
A total of 10,255 adults (4,149 males and 6,106 females) between the ages of 35 and 70 participated in this study. After applying the inclusion and exclusion criteria, 9,976 participants were included in the final analysis, including 4,083 individuals with metabolic syndrome and 5,893 healthy individuals. The average Body Mass Index of individuals with metabolic syndrome was 30.6 ± 4.5 kg/m², while healthy individuals had an average BMI of 26.8 ± 4.4 kg/m². No significant difference in BMI was observed between the two groups. However, individuals with metabolic syndrome exhibited significantly higher values for height, weight, and abdominal circumference compared to the control group (P = 0.001) (Table 1).
| Variables | Healthy (N = 5893) | Metabolic Syndrome (N = 4083) | P-Value |
|---|---|---|---|
| Height (cm) | 162.5 ± 9.0 | 159.9 ± 8.8 | 0.001 |
| Weight (kg) | 78.6 ± 13.5 | 70.92 ± 12.7 | 0.002 |
| BMI (kg/m2) | 26.8 ± 4.4 | 30.6 ± 4.5 | 0.138 |
| Waist circumference (cm) | 100.5 ± 8.4 | 106.1 ± 9.3 | 0.001 |
| Abdominal circumference (cm) | 89.4 ± 10.4 | 99.4 ± 9.9 | 0.001 |
| Wrist circumference (cm) | 1.2 ± 16.7 | 1.3 ± 17.1 | 0.081 |
Abbreviation: BMI: Body Mass Index.
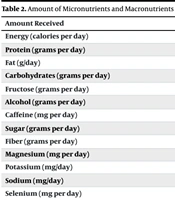
The study's participants were found to engage in an average of 43.03 ± 9.27 MET hours/day, with a median of 40.68 (range: 24 - 103) hours/day. It was noted that 57.0% of individuals with metabolic syndrome and 45.2% of those without had MET values lower than the median (P = 0.001). Regarding dietary habits, the metabolic syndrome group consumed an average total energy intake of 2189.74 ± 721.90 kcal, while the healthy group consumed 2354.92 ± 4.04 kcal, showing a significant difference (P = 0.006). Significant variations were also observed between the groups in the intake levels of carbohydrates, alcohol, caffeine, fiber, potassium, beta-carotene, trans fatty acids, total saturated fats (P = 0.001), and omega-3 (Table 2). However, there were no notable differences in the intake of other nutrients analyzed.
| Amount Received | Healthy (n = 5893) | Metabolic Syndrome (n = 4083) | P-Value |
|---|---|---|---|
| Energy (calories per day) | 2354.92 ± 754.04 | 721.90 ± 2189.74 | 0.006 |
| Protein (grams per day) | 25.43 ± 74.98 | 25.40 ± 71.07 | 0.862 |
| Fat (g/day) | 60.77 ± 23.99 | 55.87 ± 23.86 | 0.100 |
| Carbohydrates (grams per day) | 134.91 ± 390.20 | 126.17 ± 364.97 | 0.001 |
| Fructose (grams per day) | 32.41 ± 18.86 | 34.06 ± 18.90 | 0.143 |
| Alcohol (grams per day) | 0.11 ± 0.03 | 0.10 ± 0.02 | 0.001 |
| Caffeine (mg per day) | 124.52 ± 164.54 | 110.54 ± 152.35 | 0.001 |
| Sugar (grams per day) | 62.74 ± 137.78 | 59.81 ± 130.23 | 0.109 |
| Fiber (grams per day) | 27.91 ± 11.46 | 28.68 ± 11.86 | 0.007 |
| Magnesium (mg per day) | 351.53 ± 116.98 | 344.36 ± 120.31 | 0.097 |
| Potassium (mg/day) | 3787.92 ± 1396.36 | 1461.14 ± 3829.92 | 0.001 |
| Sodium (mg/day) | 4140.39 ± 1756.23 | 1757.85 ± 3941.61 | 0.438 |
| Selenium (mg per day) | 56.86 ± 29.79 | 53.34 ± 29.91 | 0.832 |
| Beta-carotene (micrograms per day) | 4961.50 ± 3538.17 | 3759.06 ± 5412.55 | 0.001 |
| Vitamin E (mg per day) | 3.75 ± 7.27 | 3.81 ± 7.19 | 0.782 |
| Vitamin D (micrograms per day) | 1.44 ± 0.90 | 1.35 ± 0.96 | 0.432 |
| Vitamin C (mg per day) | 112.91 ± 163.08 | 116.24 ± 172.00 | 0.041 |
| Cholesterol (mg/day) | 264.92 ± 134.57 | 235.94 ± 137.42 | 0.051 |
| Trans fatty acid (grams per day) | 0.29 ± 0.29 | 0.27 ± 0.24 | 0.001 |
| Saturated fatty acid (g/day) | 22.67 ± 10.33 | 9.82 ± 20.49 | 0.001 |
| Monounsaturated fatty acid (g/day) | 18.84 ± 8.04 | 8.31 ± 17.26 | 0.471 |
| Polyunsaturated fatty acid (g/day) | 12.71 ± 5.76 | 5.81 ± 11.94 | 0.914 |
| Three-Total Omega (grams per day) | 0.033 ± 0.044 | 0.037 ± 0.043 | 0.027 |
| Docosahexaenoic (acid grams per day) | 0.024 ± 0.029 | 0.025 ± 0.032 | 0.001 |
| Cozapentanoic acid (grams per day | 0.49 ± 0.35 | 0.45 ± 0.33 | 0.167 |
| Alphalinolic acid (grams per day) | 11.86 ± 11.17 | 11.15 ± 12.37 | 0.767 |
| Omega 6 (grams per day) | 5.22 ± 3.73 | 3.70 ± 4.78 | 0.068 |
Based on this research, significant differences were found between the two groups in terms of salt usage in food, consumption of fried foods like potatoes, onions, vegetables, and the type of oil used (P = 0.001). The study revealed that individuals with metabolic syndrome had lower rates of constantly (8.7%) or sometimes (16.4%) adding salt to their meals compared to the healthy group, where continuous (12.6%) and occasional (21.6%) salt addition was more common. Additionally, the consumption of fried foods 1 - 3 times a week was notably higher in the metabolic syndrome group (49.4%) compared to the healthy group (46.5%) (P = 0.001) (Table 3).
| Variables | Healthy (N = 5893) | Metabolic Syndrome (N = 4083) | P-Value |
|---|---|---|---|
| Number of meals per day | 0.163 | ||
| Three meals (breakfast, lunch and dinner) | 720 (12.2) | 436 (10.7) | |
| Four meals (three meals plus a snack) | 2292 (38.9) | 1607 (39.4) | |
| Five to six meals (three meals plus 2 - 3 snacks) | 2548 (43.2) | 1821 (44.6) | |
| More than 6 servings | 272 (4.6) | 181 (4.4) | |
| Less than 3 servings | 61 (1.0) | 38 (0.9) | |
| Adding salt to food | 0.001 | ||
| Yes | 741(12.6) | 354 (8.7) | |
| Sometimes | 1270 (21.6) | 670 (16.4) | |
| No | 3881 (65.9) | 3059 (74.9) | |
| Eating grilled foods | 0.595 | ||
| Never | 125 (2.1) | 106 (2.6) | |
| Less than once a month | 1525 (25.9) | 1068 (26.2) | |
| One to three times a month | 2946 (50.0) | 2031 (49.7) | |
| One to three times a week | 1284 (21.8) | 870 (21.3) | |
| Daily | 13 (0.2) | 8 (0.2) | |
| Eating fried foods | 0.001 | ||
| Never | 32 (0.5) | 50 (1.2) | |
| Less than once a month | 43 (0.7) | 41 (1.0) | |
| One to three times a month | 279(4.7) | 299 (7.3) | |
| One to three times a week | 2743 (46.5) | 2018 (49.4) | |
| Daily | 2796 (47.4) | 1675 (41.0) | |
| Consumption of french fries | 0.001 | ||
| Slightly fried | 417 (7.1) | 353 (8.6) | |
| Semi-fried | 4165 (70.7) | 2762 (67.6) | |
| Fully fried | 1231 (20.9) | 830 (20.3) | |
| No consumption | 80 (1.4) | 138 (3.4) | |
| Eating fried onions | |||
| Slightly fried | 1028 (17.4) | 805 (19.7) | |
| Semi-fried | 4211 (71.5) | 2814 (68.9) | |
| Fully fried | 614 (10.4) | 403 (9.9) | |
| No consumption | 40 (0.7) | 61 (1.5) | |
| Eating fried vegetables | 0.001 | ||
| Slightly fried | 4190 (71.1) | 2742 (67.2) | |
| Semi-fried | 998 (16.9) | 737 (18.1) | |
| Fully fried | 502 (8.5) | 407 (10.0) | |
| No consumption | 203 (3.4) | 197 (4.8) | |
| Consumable oil | 0.001 | ||
| Solid | 1360 (23.1) | 844 (20.7) | |
| Semi solid | 191 (3.2) | 104 (2.5) | |
| Liquid | 382 (6.5) | 333 (8.2) | |
| Fried | 3840 (65.2) | 2664 (65.2) | |
| Other types of oil | 111 (1.9) | 111 (2.7) | |
| No oil consumption | 9 (0.2) | 27 (0.7) | |
| Used oil consumption | 0.270 | ||
| Yes | 4049 (68.7) | 2874 (69.7) | |
| No | 1844 (31.3) | 1235 (30.3) | |
| Consumption of smoked foods | 0.769 | ||
| Never | 5652 (95.9) | 3895 (95.4) | |
| Less than once a month | 208 (3.5) | 161 (3.9) | |
| One to three times a month | 23 (0.4) | 20 (0.5) | |
| One to three times a week | 5 (0.1) | 3 (0.1) | |
| Daily | 5 (0.1) | 4 (0.1) | |
| Eating fresh vegetables | |||
| Yes | 302 (5.1) | 198 (4.8) | 0.544 |
| No | 5590 (94.9) | 3885 (95.2) | |
| The temperature of tea consumed | 0.068 | ||
| Very hot | 1984 (33.7) | 1282 (31.4) | |
| Hot | 3617 (61.4) | 2579 (63.2) | |
| Cold | 249 (4.2) | 196 (4.8) | |
| Not drinking tea | 43 (0.7) | 26 (0.6) | |
| The temperature of the soup | 0.280 | ||
| Very hot | 1673 (28.4) | 1130 (27.7) | |
| Hot | 3936 (66.8) | 2781 (68.1) | |
| Cold | 259 (4.4) | 161 (3.9) | |
| Not drinking tea | 25 (0.4) | 11 (0.3) |
5. Discussion
Considering the increase in the prevalence of heart diseases and diabetes in recent years, and the high prevalence of metabolic syndrome in Iran, especially in Mazandaran province—with its high rates of hypertension, hyperglycemia, and obesity—the study aimed to explore the connection between metabolic syndrome, dietary habits, and physical activity levels among individuals enrolled in the Tabari cohort study. Bread and rice are among the main food staples in Mazandaran, and reducing the prevalence of metabolic syndrome is essential for significantly reducing deaths caused by heart diseases and diabetes.
The study indicated a direct correlation between lower physical activity levels and increased susceptibility to coronary heart disease. Engaging in moderate physical activities, such as walking, was linked to a notable reduction in the risk of coronary heart disease. Vigorous activities with MET levels in the range of 5 - 9 were associated with a significant reduction in risk factors, such as high BMI, heart rate, systolic and diastolic blood pressure, and low HDL cholesterol levels among individuals with metabolic syndrome. Similar trends were observed in individuals with low physical activity levels and limited cardiorespiratory fitness (38). This aligns with the present study's findings, where patients diagnosed with metabolic syndrome exhibited a significantly lower MET Index compared to healthy individuals (38).
Zhang et al.'s meta-analysis revealed a direct correlation between leisure-time physical activity (LTPA) and the prevalence of metabolic syndrome. For every additional 10 hours per week of increased MET in LTPA, there was an 8% decrease in the risk of developing metabolic syndrome. Furthermore, meeting the recommended guidelines of 150 minutes of moderate physical activity per week (equivalent to 10 MET hours per week) resulted in a 10% decrease in the risk of metabolic syndrome onset compared to being inactive. Exceeding the recommended physical activity levels led to further reductions in the risk of metabolic syndrome, consistent with the findings of this study (12).
In another study by Sayon-Orea et al. (39), the relationship between metabolic syndrome and the consumption of fried foods was examined. Regular consumption of fried foods did not show a significant link to the development of metabolic syndrome (HR = 0.98, 95% CI 0.77-1.26, P = 0.862 for trend). However, central obesity and hypertension demonstrated a positive correlation with fried food intake. Individuals who fried foods using oils or fats other than olive oil had a higher risk of metabolic syndrome, though these associations were not statistically significant.
A study conducted by Jusuf et al. found that the consumption of fatty, cooked, and salty foods was significantly linked to metabolic syndrome (40). Similarly, research by Lutsey et al. found that the intake of red meat, fried foods, and diet soda was positively correlated with metabolic syndrome, whereas consuming dairy products had a protective effect (41). However, in the present study, the consumption of fried foods in the metabolic syndrome group was significantly lower than in the healthy control group. One reason for this contradiction could be that the metabolic syndrome group was undergoing treatment with medication and dietary adjustments. It appears that the participants had recently been informed about their condition and had begun to correct some of their eating habits.
Previous studies show that reducing the intake of saturated fatty acids (SFA) may be more effective in preventing cardiometabolic risk factors (42, 43). However, recent studies have reported conflicting results regarding the effect of SFA consumption on cardiometabolic risk factors—some report no effect (44, 45), while others report a beneficial effect (46). For example, a prospective study examining nutrient interactions and coronary atherosclerosis risk found that SFA intake was associated with less progression of atherosclerosis, but only in those with lower MUFA intake (46).
A systematic review by Julibert et al. found that SFA intake was associated with hypertension and higher fasting triglyceride, HDL, and serum glucose levels (47). Studies have explored the impact of various fat types, showing that a higher unsaturated-to-saturated fat ratio (P/S ratio) positively influenced HDL cholesterol levels (48). However, polyunsaturated fatty acid (PUFA) intake was inversely related to HDL cholesterol and waist circumference (48, 49). Consumption of PUFA n-3 was linked to improved blood pressure, triglyceride levels, glucose tolerance, and reductions in insulin resistance, waist circumference, and obesity prevalence (49, 50). Some studies suggest that higher fish intake may reduce the risk of metabolic syndrome by improving triglyceride and HDL cholesterol levels (49, 51).
However, the present study found that the metabolic syndrome group had lower consumption of trans and saturated fatty acids compared to the healthy group. This discrepancy may be attributed to the fact that some participants were undergoing dietary interventions for metabolic syndrome. The study was conducted during the first phase of the Tabari cohort, which included patients following dietary changes, potentially impacting the outcomes. Further investigation in the cohort’s second phase is necessary for more comprehensive insights.
In this study, fructose consumption was higher among healthy individuals compared to the metabolic syndrome group. Although fructose is a natural sugar found in fruits, excessive consumption has been linked to hyperlipidemia (52), diabetes, obesity, and certain cancers (53). While moderate consumption of fructose does not pose a problem, long-term overconsumption has been shown to increase the risk of obesity and conditions related to metabolic syndrome. Excessive fructose intake can also lead to fat accumulation, insulin resistance, and inflammation (54). Further investigation in future cohort phases is recommended to assess the prevalence of metabolic syndrome and refine dietary recommendations.
5.1. Limitations
Several limitations should be considered when interpreting the study's findings. Eating habits were evaluated only based on food intake, without accounting for dietary behaviors such as meal patterns, snack frequency, and meal timing (55). The study's cross-sectional nature also limits the ability to establish causality. Future studies should assess the relationship between dietary habits and metabolic syndrome in a prospective manner. Additionally, the findings cannot be generalized to the entire country, as eating habits are influenced by socio-economic factors. Nonetheless, participants from different regions with varying socio-economic statuses were included. Lastly, although we controlled for many confounding variables related to lifestyle, genetic factors were not accounted for, and they may confound the relationship between diet and metabolic syndrome.
5.2. Conclusions
The Tabari cohort study highlights the high prevalence of metabolic syndrome in Mazandaran, underscoring the importance of prevention and screening programs. Metabolic syndrome is a significant risk factor for diabetes and cardiovascular diseases, which have a high economic burden on individuals and healthcare systems. Contrary to previous studies, the present research found that the consumption of fried foods, trans fatty acids, and calories, as well as fructose intake, were lower in the metabolic syndrome group compared to the healthy group, indicating the positive effects of treatment programs in Mazandaran province. Based on the findings of this cross-sectional descriptive study, conducted during the first phase of the Tabari cohort, it is recommended that further studies be carried out to verify the types of food ingredients consumed in the current period (e.g., frying ingredients, trans fats, fructose intake, etc.). Future research should also evaluate the effects of dietary and lifestyle changes among individuals with metabolic syndrome, and their impact on preventing metabolic diseases such as diabetes and cardiovascular diseases. This should be explored in the second phase of the Tabari cohort to help reduce household healthcare expenses and alleviate the health burden on the country’s healthcare system. Additionally, prospective studies are suggested to investigate the influence of these factors on reducing the incidence of related diseases and the associated costs.