1. Background
The World Health Organization (WHO) defines dehydration as a condition resulting from excessive loss of body water (1). Dehydration is a common disorder of body fluids encountered in the nursing care of infants and young children. It occurs when the total output of body fluids is greater than the total intake (2). Dehydration is a leading cause of death among children under 5 years of age worldwide. Approximately 760,000 children around the world contract diarrheal diseases annually. A study by Omoke et al. reported a 15.9% prevalence of dehydration in children (3), while Vorlasane et al. observed a higher rate of 48.4% (4). Maleki et al. studied 118 Iranian children under 3 years old with acute gastroenteritis and found mild dehydration in 46.4%, moderate in 35.7%, and severe in 17.9% (5). According to Mosav et al.'s study, among children with gastroenteritis referred to medical centers, 4.4% of patients had mild dehydration, 78.7% had moderate dehydration, and 20.8% had severe dehydration, of which 41.6% of these patients had disorders in sodium levels and 17.2% had disorders in potassium levels (6).
Dehydration in children is mostly caused by acute gastroenteritis, primarily due to infectious agents. In the United States, 75% to 90% of infectious diarrhea is caused by viral infections, while bacterial pathogens and parasites contribute to less than 20% and 5% of cases, respectively (1). The degree of dehydration varies according to age, with infants having a total body water content of 70% to 80% of body weight and older children having 60%. Dehydration is classified as mild (3% to 5% loss of body weight), moderate (6% to 10%), and severe (over 10%) (7). Children experiencing persistent diarrhea who consume excessive water may develop hyponatremic dehydration due to simultaneous loss of sodium and bicarbonate (8). Colleti et al. identified prolonged skin turgor, capillary refill time, abnormal breathing, and decreased serum bicarbonate as signs of dehydration (9). In the study by Maleki et al., rotavirus gastroenteritis was associated with fever (65.5%), vomiting (65.5%), and rhinorrhea (24.1%) (5). Prisco et al. described symptoms of moderate dehydration, including thirst, restlessness, slightly sunken eyes, reduced tears, and mucous membrane adhesion (10). Hoxha et al. listed decreased skin turgor, sunken eyes, weak pulse, tachycardia, impaired breathing, decreased tears, dry mucous membranes, prolonged capillary refill time, and decreased urinary output as dehydration symptoms (11).
Considering the high prevalence of dehydration (3) and the risks caused by it, including the risk of death and the costs imposed on the health and treatment system and families due to the increase in the duration of hospitalization and the return visits of patients, it is necessary to investigate its causes and formulate preventive strategies (6, 12). Amirkola Children's Hospital in Babol, Iran, experiences a high number of dehydration-related emergency visits. Limited studies have been conducted on dehydration factors in Iranian children, emphasizing the need for further research in this area. Additionally, factors contributing to dehydration in children may vary across countries and regions due to differences in cultural, economic conditions, and healthcare facilities.
2. Objectives
The aim of this study was to identify the factors related to dehydration in children admitted to the Emergency Department of Amirkola Children's Hospital, with the goal of providing suitable solutions to prevent dehydration among children in this region and ultimately reduce its prevalence.
3. Methods
3.1. Study Design and Participants
This cross-sectional study assessed all children under 18 years of age (census sampling) with moderate to severe dehydration who were referred to the emergency department of Amirkola Children's Hospital in Babol, Iran, from May 1 to September 15, 2023. Amirkola Children's Hospital is a specialized educational center for children affiliated with Babol University of Medical Sciences. It is the largest specialized children's hospital in the north of Iran, serving many clients from different regions. This center is a specialized hospital that, in addition to general pediatric departments, has specialized departments such as NICU, PICU, oncology, infectious diseases, dialysis, and bone marrow transplant. Census sampling was conducted according to the inclusion criteria. The inclusion criteria included all patients diagnosed with dehydration who were under 18 years of age (13, 14) and had not received intravenous treatment interventions in other medical centers within the last 24 hours. The exclusion criterion was parental unwillingness to participate in the study.
3.2. Data Collection
A three-part questionnaire was developed through reviewing relevant sources and consultation with a specialist in pediatric infectious diseases. It was then given to ten members of the pediatric nursing faculty and pediatricians for review and approval. The questionnaire comprised demographic information, basic characteristics, and associated clinical symptoms. Data were collected by the researcher before treatment initiation through reviewing patients' medical records and interviewing the patients' parents or companions. Accompanying clinical symptoms were documented by a pediatrician. Dehydration severity was classified as mild (3% - 5% weight loss), moderate (6% - 10% weight loss), or severe (over 10% weight loss) and was confirmed by a pediatrician. Severe dehydration was identified by the presence of two or more of the following symptoms: Abnormal sleepiness or impaired consciousness, sunken eyes, difficulty drinking, and very slow return of skin to its normal state. Moderate dehydration was characterized by the presence of two or more of these symptoms: Restlessness, irritability, sunken eyes, thirst, and slow return of skin to its normal state (7).
The first part of the questionnaire included the child's demographic characteristics, such as age, sex, birth weight, weight at the time of hospitalization, age at hospitalization, type of maternal delivery and prematurity, place of residence, family income, parental education and occupation, duration of symptoms, recent travel history, and medication due to underlying disease. The second part included basic and background information, encompassing questions about feeding during infancy, duration of exclusive feeding, history of diarrhea in the past month, vaccination history, zinc supplementation, reason for hospitalization, type of illness, oral rehydration solution (ORS) administration, home remedies, probiotic intake, and other relevant aspects. The third part focused on accompanying clinical symptoms, such as fever, diarrhea, nausea and vomiting, abdominal pain, abnormal breathing, heart rate, skin turgor, capillary refill time, blood pressure, tear production, consciousness level, urination frequency, paleness, abdominal distension, and other pertinent factors (1, 15).
It should be noted that all children with dehydration referred to the emergency department were included in the study, and the information related to their medical records, the severity of dehydration, and other clinical symptoms were recorded in the questionnaire.
3.3. Statistical Analyses
Descriptive measures, such as frequency, percentage, mean, and standard deviation, were utilized to depict the demographic and clinical information of patients. Simple logistic regression was initially employed to establish the relationship between each variable under study and the binary outcome. Variables with a significance level below 0.2 in the univariate analysis were subsequently incorporated into a multiple logistic regression model. The effect of the main independent variables was ultimately evaluated using the stepwise-backward method, with confounders controlled, and adjusted odds ratios reported. For quantitative outcomes, adjusted effect sizes were reported using a multiple linear regression model and a zero-inflated negative binomial model. Stata statistical software version 17 was used for data analysis. A significance level of less than 0.05 was adopted for all tests.
3.4. Ethical Considerations
This cross-sectional study was conducted with ethical approval from the Research Ethics Committee of Babol University of Medical Sciences (IR.MUBABOL.REC.1402.094). All participants provided written consent, were informed about the study, and were assured of confidentiality. No fees were charged to participants for their involvement in the study.
4. Results
In this study, 141 children with moderate to severe dehydration were included, with a mean age of 30.60 ± 2.98 months. Of the participants, 41.1% resided in rural areas, and 15.7% had a recent travel history (Table 1).
| Demographic and Basic Data | Values |
|---|---|
| Age (mon) | 30.60 ± 2.98 |
| Weight (kg) | 14.81 ± 7.64 |
| Birth weight (g) | 3132.3 ± 688.41 |
| Gender | |
| Male | 96 (68.1) |
| Female | 45 (31.9) |
| Residence | |
| Urban | 83 (58.9) |
| Rural | 58 (41.1) |
| Family income | |
| Poor | 16 (11.4) |
| Moderate | 86 (61.4) |
| Good | 38 (27.1) |
| Type of delivery | |
| Vaginal | 43 (30.5) |
| Cesarean | 98 (69.5) |
| Mother’s job | |
| Employee | 51 (36.2) |
| Housewife | 90 (63.8) |
| Father’s job | |
| Employee | 43 (30.5) |
| Worker | 33 (23.4) |
| Freelance | 65 (46.1) |
| Mother’s education | |
| Below diploma | 14 (9.9) |
| Diploma | 56 (39.7) |
| University | 71 (50.4) |
| Father’s education | |
| Below diploma | 21 (14.9) |
| Diploma | 48 (34.0) |
| University | 72 (51.1) |
| Recent travel history | |
| Yes | 22 (15.7) |
| No | 118 (84.3) |
| Prematurity | |
| Yes | 15 (10.6) |
| No | 126 (89.4) |
| History of Covid-19 | |
| Yes | 6 (4.3) |
| No | 135 (95.7) |
| Vaccination | |
| Complete | 131 (92.9) |
| Incomplete | 10 (7.1) |
a Values are expressed as mean ± SD or No. (%).
In this study, 61% of patients visited the emergency department 48 hours after symptom onset. Notably, 44% of participants did not receive zinc supplements, and 59.6% of families were unaware of the significance of ORS administration. Additionally, 19.9% of mothers did not wash their hands before preparing food (Table 2).
| Data Related to Dehydration | Values |
|---|---|
| Duration of exclusive breastfeeding (mon) | 3.3 ± 2.5 |
| Duration of hospitalization in the emergency department (d) | 5.1 ± 2.5 |
| Referral time after the onset of symptoms (h) | |
| < 24 | 35 (24.8) |
| 24 - 48 | 20 (14.2) |
| > 48 | 86 (61.0) |
| Type of feeding during infancy | |
| Breastfeeding | 45 (32.1) |
| Formula | 61 (43.6) |
| Both | 34 (24.3) |
| History of diarrhea in the last month | |
| Yes | 29 (20.6) |
| No | 112 (79.4) |
| Zinc supplement | |
| Yes | 79 (56.0) |
| No | 62 (44.0) |
| Home treatment | |
| Yes | 100 (70.9) |
| No | 41 (29.1) |
| Awareness of ORS consumption | |
| Yes | 57 (40.4) |
| No | 84 (59.6) |
| Hand Washing by mother | |
| Yes | 113 (80.1) |
| No | 28 (19.9) |
| Antibiotic therapy | |
| Yes | 77 (54.6) |
| No | 64 (45.4) |
| Inpatient status | |
| Discharge | 11 (7.8) |
| Transfer to the ward | 130 (92.2) |
| Take probiotics | |
| Yes | 52 (36.9) |
| No | 89 (63.1) |
| Receive anti-nausea medication | |
| Yes | 26 (18.4) |
| No | 115 (81.6) |
| Receiving anticholinergic medication | |
| Yes | 5 (3.5) |
| No | 136 (96.5) |
Abbreviation: ORS, oral rehydration solution.
a Values are expressed as mean ± SD or No. (%).
In this study, 79.9% of the referred children had fever, 69.5% had nausea, 30.5% had abdominal distention, and 61.7% had abnormal skin turgor. Other symptoms associated with dehydration are listed in Table 3.
| Clinical Symptoms Combined with Dehydration | Values |
|---|---|
| Fever | |
| Yes | 100 (70.9) |
| No | 41 (29.1) |
| Vomiting | |
| Yes | 98 (69.5) |
| No | 43 (30.5) |
| Abdominal pain | |
| Yes | 67 (47.5) |
| No | 74 (52.5) |
| Dyspnea | |
| Yes | 25 (18.0) |
| No | 114 (82.0) |
| Seizures | |
| Yes | 4 (2.8) |
| No | 137 (97.2) |
| Skin turgor | |
| Normal | 54 (38.3) |
| Abnormal | 87 (61.7) |
| Capillary filling time (sec) | |
| < 3 | 22 (15.6) |
| > 3 | 119 (84.4) |
| Tearing | |
| Yes | 6 (4.3) |
| No | 135 (95.7) |
| Oliguria | |
| Yes | 56 (39.7) |
| No | 85 (60.3) |
| Paleness | |
| Yes | 68 (48.2) |
| No | 73 (51.8) |
| Abdominal distension | |
| Yes | 43 (30.5) |
| No | 98 (69.5) |
| Blood pressure | |
| Systole | 89.3 ± 11.4 |
| Diastole | 60.2 ± 7.0 |
| Frequency of nausea and vomiting b | 4.12 ± 3.45 |
| Frequency of diarrhea | 6.02 ± 5.60 |
| Heart rate | 97.11 ± 14.15 |
a Values are expressed as mean ± SD or No. (%).
b Among patient who had nausea and vomiting.
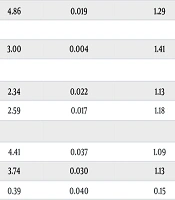
The likelihood of dyspnea in patients with a history of drug use was 4.86 times higher than in those without such a history [odds ratio (OR), 4.86; 95% confidence interval (CI), 1.29 - 18.23]. Rural patients demonstrated a threefold increased likelihood of abnormal skin turgor compared to urban patients. Additionally, children who did not receive zinc supplements (OR, 1.33), resided in rural areas (OR, 1.35), or had mothers who did not wash their hands before food preparation (OR, 1.48) were more likely to experience diarrhea (Table 4).
| Outcome and Related Risk Factor | AOR b | P-Value | Lower CI c | Upper CI |
|---|---|---|---|---|
| Dyspnea d | ||||
| History of drug use (no) | 4.86 | 0.019 | 1.29 | 18.23 |
| Turgor | ||||
| Residence (urban) | 3.00 | 0.004 | 1.41 | 6.36 |
| Oliguria d | ||||
| Zinc supplement (yes) | 2.34 | 0.022 | 1.13 | 4.84 |
| Outpatient treatment (yes) | 2.59 | 0.017 | 1.18 | 5.69 |
| Distension d | ||||
| History of drug use (no) | 4.41 | 0.037 | 1.09 | 17.75 |
| Trip history (no) | 3.74 | 0.030 | 1.13 | 12.34 |
| Hand washing (yes) | 0.39 | 0.040 | 0.15 | 0.95 |
| Seizure d | ||||
| History of drug use (no) | 16.00 | 0.009 | 1.98 | 128.85 |
| Diarrhea e | ||||
| Zinc supplement (yes) | 1.33 | 0.029 | 0.99 | 1.79 |
| Residence (urban) | 1.35 | 0.047 | 0.96 | 1.90 |
| Hand washing (yes) | 1.48 | 0.029 | 0.98 | 2.23 |
a Categories of the parentheses are considered reference group in analyses.
b Adjusted odds ratio.
c Confidence interval.
d Multiple logistic regression model stepwise-backward method (effect size is odds ratio).
e Multiple zero-inflated negative binomial model.
5. Discussion
This study explored the factors associated with dehydration in children admitted to the emergency department of Amirkola Children's Hospital, Babol. We found that 61% of children arrived at the emergency department 48 hours after the onset of diarrhea symptoms. This delay in seeking care could be a significant contributing factor to the severity of dehydration observed in these children. Rapid oral rehydration therapy administered over 3 to 4 hours is crucial for treating acute gastroenteritis with dehydration (16). Timely and appropriate referral of children with diarrhea can potentially reduce up to 20% of childhood deaths and prevent its long-term complications (17). Fikire et al. identified several key factors contributing to the delayed referral of children with diarrhea, including the child's gender (female), age (less than 24 months), caregivers without formal education, poor economic status, dissatisfaction with healthcare workers' performance in the past six months, and lack of respect from healthcare providers (18).
In our study, 71% of patients initially attempted home remedies, suggesting that reliance on such methods could be a reason for delayed emergency department visits. Furthermore, over 60% of parents were unaware of ORS treatment for dehydration, highlighting a knowledge gap regarding effective home remedies. Inappropriate home remedies, such as administering opiates, self-administering drugs, temporary serum therapy, and providing oral solutions with high carbohydrate concentrations (e.g., hot plant extracts), not only fail to effectively treat dehydration but can sometimes exacerbate the condition.
In this study, most children exhibited symptoms such as fever (71%), vomiting (69.5%), abnormal skin turgor (61.7%), lack of tears (95.7%), oliguria (35.7%), paleness (48.2%), and abdominal distension (30.5%). The high prevalence of vomiting and fever in our study can be attributed to the inclusion of samples with moderate and severe dehydration. This finding is consistent with Vorlasane et al.'s study, which reported vomiting (66.6%) and fever (60.6%) as the most common symptoms associated with diarrhea in dehydrated hospitalized children (4). Another study revealed that 3% of children referred with diarrhea presented with prolonged capillary refill time, 71% had a thread-like pulse, 97% had dry mucous membranes, 54% had abnormal skin turgor, and 10.5% had oliguria (19). Vorlasane et al. found fever (60%) and vomiting (66%) as the most common symptoms associated with diarrhea (4). In Sharma et al.'s study, abdominal distension (29%), vomiting (71%), fever (87%), and respiratory disorder (27%) were symptoms linked to severe dehydration (20).
History of travel, underlying illness of the child, and the mother's failure to wash hands before preparing food were the most significant factors related to dehydration in our study. Non-observance of public hygiene during travel, such as dining at restaurants, consuming prepared food, and the lack of proper sanitary facilities, may contribute to these findings. Soriano-Arandes et al. also reported travel history as a risk factor for gastroenteritis syndrome (21). Additionally, another study found that 84% of children with diarrhea and dehydration had at least one additional diagnosis, such as malaria, pneumonia, HIV, tuberculosis, anemia, meningitis, rickets, or asthma (22). Furthermore, hand washing has been demonstrated to reduce diarrhea incidence by approximately 30% in high-income countries and low- to middle-income communities (23). Other studies have also highlighted the importance of hand washing, toilet cleanliness, access to safe drinking water, and timely initiation of complementary feeding in reducing gastroenteritis (24, 25). Sharma et al. further identified factors such as living in crowded environments (lack of hygiene), not being exclusively breastfed in the first six months, not receiving ORS solution before referral, and no history of oral zinc supplementation as elements associated with severe dehydration (20).
In this study, the likelihood of dyspnea was higher in children who had a history of underlying disease. This problem may be due to the presence of accompanying diseases that have affected the respiratory system. On the other hand, the imbalance of fluids and electrolytes caused by dehydration (metabolic acidosis) can be associated with disturbances in the breathing pattern (26). The findings of our study showed that rural children had more skin turgor disorder. Considering that the disturbance in the intensity of skin turgor depends on the severity of dehydration, rural children probably had more severe dehydration than urban children. Late referral (due to the greater distance of the villagers from the medical centers) or the lower health level of the villagers can justify this issue. In Özdil and Vardar's study, complications of dehydration were more common in rural and suburban children than in urban children (27).
Children who did not take zinc supplements had more oliguria in this study. Since oliguria is seen in people who are more severely dehydrated, oliguria is more common in children who have not taken zinc supplements (28). Zinc supplementation in children who are dehydrated due to diarrhea helps to control diarrhea and the severity of dehydration by accelerating the recovery of intestinal epithelium (29). The results of this study showed that abdominal distension was more common in children who had a history of underlying disease. This is probably because diarrhea (one of the most important causes of dehydration in children) is more severe in children with underlying diseases. Severe diarrhea can cause significant abdominal distension due to the formation of gas, liquids, or excrement in the intestine (30). Travel history and the mother's failure to wash hands before preparing food were related to abdominal distension in the studied children. In Dawson et al.'s study, the symptoms of dehydration were more severe in children who had a history of traveling and did not observe hygiene tips such as hand washing (31). In fact, not washing hands is likely to lead to more severe diarrhea and, as a result, abdominal distension.
Seizures were significantly higher in children who had a history of underlying disease in this study. It is possible that the underlying disease that led to the use of medication played a role in the occurrence of seizures in the present study. Additionally, in the study by Kariuki et al., infectious diseases in childhood and neonatal and perinatal complications are mentioned as seizure risk factors (32). The results of our study showed that the frequency of diarrhea had a significant relationship with not taking zinc supplements. A study in Nigeria found that only about 30% of children with diarrhea received zinc supplements (33). The WHO recommends treating childhood diarrhea with ORS and zinc supplementation (34). Oral rehydration solution and zinc supplementation are easy and effective interventions, and it is estimated that ORS reduces the risk of mortality from diarrhea by 93%, and zinc supplementation reduces the duration of diarrhea, stool output, and the risk of persistent diarrhea (35).
Our study showed that children living in villages and children whose mothers did not wash their hands before preparing food had more diarrhea. In the study by Chatterjee et al. in west Bengal, India, similar results were obtained (36). Of course, one of the possible reasons for this is the lower level of health in the village environment compared to the city and the lower level of knowledge among mothers. One of the strengths of this study is the comprehensive investigation of factors related to dehydration in children. Our study also had some limitations. The majority of children suffering from dehydration had gastroenteritis, and the factors related to other causes of dehydration may have been hidden from the researcher. In this study, only children with moderate and severe dehydration were examined, and the results may not be generalizable to children with mild dehydration. Due to the cross-sectional nature of this study, it is not possible to establish causality, and the long-term effects of the identified risk factors on dehydration cannot be assessed over time.
5.1. Conclusions
In the current study, the late referral of children is expressed as an effective result in the treatment of dehydration. Additionally, history of travel, having an underlying disease, not washing hands before preparing food, rural life, and not taking zinc supplements are the most important factors related to dehydration in children. These findings of this study have presented valuable insights which can be generalized to a broader population of children at risk in similar contexts. Further research may be needed to examine the generalizability of some findings, such as the impact of rural living on the severity of dehydration. The results of this study can provide a basis for government decision-making or inspire future research efforts. Early identification of dehydration symptoms is necessary for preventive measures and timely treatment. Therefore, it is recommended to include preventive educational interventions to prevent dehydration and encourage early referral in family educational programs.