1. Background
Nurse-patient communication denotes the relationship and engagement between nursing professionals and patients. Nursing practice should sustain effective communication with patients to optimize nursing care and patient outcomes (1). Proper communication is particularly important when interacting with patients to understand their conditions. Nurses should approach patients with kindness, sincerity, and courtesy, leveraging their education and experience to develop effective communication skills, especially during critical stages of care (2).
Communication is frequently perceived as an interactive process within a social context, involving a sender and a receiver who exchange signals. These signals can be verbal or non-verbal, including gestures or visual representations (e.g., photographs). Ultimately, communication involves the use of codes expressed through visual signals, physical movements, or spoken sounds (3, 4).
Patient satisfaction is an important indicator of communication engagement, relationships, experiences, and nursing care quality. It influences medical malpractice claims, efficiency, patient retention, and clinical outcomes (5, 6). Moreover, patient satisfaction reflects concerns about healthcare experiences across different departments. As a multidimensional concept, it encompasses perceptions of information, technical skills, and communication. Healthcare professionals, such as nurses, use patient satisfaction levels to assess their skills and interventions in meeting the expectations of patients and their families (7).
Factors such as waiting times, communication with nurses and other healthcare professionals, amenities, and quality improvement measures shape patient satisfaction levels (6). The emergency department (ED) is among the departments requiring effective nurse-patient communication (8). This communication helps establish rapport during history-taking, facilitates information gathering, and maintains collaboration throughout care (9, 10).
Successful communication in the ED is critical for nurses and other healthcare professionals to provide timely and effective care to save lives. Effective engagement among healthcare providers in the ED influences their decisions and responses to incidents affecting patient care, safety, and overall outcomes (11). Given the demanding and critical environment of the ED, clear communication is necessary before, during, and after procedures for healthcare teams to understand patient preferences. Nurses should also communicate with patients to prevent adverse incidents or conflicts, particularly those arising from spiritual and cultural preferences in interventions (12).
Poor nurse-patient communication in the ED remains prevalent, despite its critical role in the success of care interventions. Barriers such as language differences between nurses and patients and low self-confidence among nurses complicate the communication process (13). Additionally, the demanding and overcrowded nature of the ED increases the workload of nurses. Communication challenges also arise due to environmental factors and patient-related issues (14).
A study has identified insufficient communication between nurses and patients as a significant factor contributing to low patient satisfaction scores. This issue is particularly evident in specialized care environments, where ineffective communication can result in negative patient outcomes and dissatisfaction (15). Studies have yet to explore the link between nurse-patient communication and patient satisfaction in the ED. For example, in the West Bank, Al-Kalaldeh et al. (16) found knowledge gaps, psychological instability, economic barriers, and social issues affecting communication. They acknowledged the existence of nurse-patient communication in the ED but did not address its effect on patient satisfaction.
Contrastingly, Alshehry (17) surveyed Saudi Arabian nurses, who reported communication contradictions, mistrust, poor teamwork, and incompetence in their roles. These challenges instigated patient-nurse conflicts, resulting in poor outcomes, but the focus was on general wards rather than the ED and patient satisfaction. The aforementioned gaps highlight the need to understand how nurse-patient communication affects patient satisfaction in the ED.
The King Abdullah Medical Complex–Jeddah is among the healthcare institutions in Saudi Arabia seeking to optimize care through effective communication and patient satisfaction. Thus, the study aimed to evaluate the impact of nurse-patient communication on patient satisfaction in the ED. The research question was: What is the impact of nurse-patient communication on patient satisfaction in the ED?
2. Objectives
This study identifies the factors influencing nurse-patient communication on patient satisfaction in the ED.
3. Methods
3.1. Study Design
The study adopted a quantitative cross-sectional design, which is frequently selected for descriptive or exploratory aims due to its cost-effectiveness and accessibility. However, such designs face limitations in their ability to evaluate causal processes and track individual changes over time (18). The research design and reporting adhered to the EQUATOR reporting guidelines, specifically following the strengthening the reporting of observational studies in epidemiology (STROBE) checklist (19).
3.2. Study Setting and Participants
The study was conducted in the ED at the King Abdullah Medical Complex–Jeddah over a one-year period, from September 19, 2023, to September 30, 2024. The study participants included ED nurses and admitted patients. The sample size was determined using the Raosoft sample size calculator (20). A convenience sampling method was employed to select participants who were readily accessible and met the inclusion criteria. The sample consisted of 401 patients and 60 nurses.
Inclusion criteria included patients admitted to the ED aged 18 - 60 years, with a Glasgow Coma Scale (GCS) score of 15, and categorized under Canadian Triage and Acuity Scale (CTAS) 3 and 4, as well as nurses working in the ED. Excluded were non-emergency patients, those with a GCS score of < 15, patients categorized under CTAS 1 and 2, and nurses working outside the ED.
3.3. Data Collection and Measurement
The research team directly collected data using structured questionnaires. Participants, including patients and nurses in the ED, were approached and provided with a detailed verbal and written explanation of the study's purpose. The questionnaires were distributed, allowing participants to complete them independently or seek assistance from the research team if needed to ensure inclusiveness. Researchers remained on-site to provide clarification and ensure accurate completion of the forms.
Data collection was conducted using three questionnaires. The first focused on demographic data, including patients' sex, marital status, educational level, ED stay, and hospital admissions in the last two years. It also included nurses' sex, age, marital status, nationality, educational level, years of nursing experience, current position, years in the current position, monthly pay, compensation, benefits, and work conditions.
The second questionnaire utilized was the La Monica Oberst Patient Satisfaction Scale (LOPSS), created by La Monica et al. (21) in 1986 to evaluate patient satisfaction concerning nursing care. This tool demonstrates significant reliability and validity, with a Cronbach’s alpha of 0.92, originally included 41 questions with seven response options on a Likert scale ranging from “totally disagree” to “strongly agree”. For the modified version, items 1, 9, 16, 20, 21, 25, 30, 31, 33, 34, 35, 37, 38, 40, and 41 were retained, while the remaining items were removed. This version used a 5-point Likert scale ranging from “totally disagree” to “strongly agree”. The total possible scores ranged from 15 to 75, with higher scores reflecting greater nursing service satisfaction. The modified LOPSS measured discontent (three items), interpersonal support (four items), and pleasant impression (eight items). An expert group examined the content and validity of this version.
The third questionnaire was the Nurse Quality of Communication with Patient Questionnaire (NQCPQ). This questionnaire comprises 25 items and uses a scale of 1 to 5 to assess nurse-patient communication. In this study, items 4, 8, 16, 20, 22, and 24 were modified, and the Likert scale was changed from “excellent” to “poor” (22).
3.3.1. Reliability (Internal Consistency) of the Survey Instruments
The two instruments demonstrated good reliability (Table 1). Cronbach’s alpha coefficients were 0.899 and 0.856 for the LOPSS and NQCPQ, respectively.
| Survey Instruments | Items | Cronbach’s Alpha Coefficient |
|---|---|---|
| LOPSS | 15 | 0.899 |
| NQCPQ | 6 | 0.856 |
Reliability (Internal Consistency) of the Survey Instruments
3.3.2. Validity of the Nurse Quality of Communication with Patient Questionnaire
The validity of the NQCPQ was examined using Pearson’s correlation coefficients to determine the degree of correlation between each item and the overall scale. Table 2 shows that all NQCPQ items highly correlated with the overall scale.
| Items | Correlation Coefficient |
|---|---|
| 1 | 0.623 |
| 2 | 0.521 |
| 3 | 0.709 |
| 4 | 0.776 |
| 5 | 0.574 |
| 6 | 0.757 |
| 7 | 0.706 |
| 8 | 0.764 |
| 9 | 0.775 |
| 10 | 0.772 |
| 11 | 0.768 |
| 12 | 0.620 |
| 13 | 0.750 |
| 14 | 0.731 |
| 15 | 0.756 |
Validity of the Nurse Quality of Communication with Patient Questionnaire
3.3.3. Validity of the La Monica Oberst Patient Satisfaction Scale
All LOPSS items substantially correlated with the overall scale (Table 3), verifying that all items fulfilled the measurement standards.
| Items | Correlation Coefficient |
|---|---|
| 1 | 0.812 |
| 2 | 0.856 |
| 3 | 0.850 |
| 4 | 0.755 |
| 5 | 0.827 |
| 6 | 0.817 |
Validity of the La Monica Oberst Patient Satisfaction Scale
3.4. Data Analysis
The demographic data were presented as frequencies and percentages. The scores for each item in the LOPSS and NQCPQ were interpreted using means and standard deviations (SDs). Cronbach’s alpha coefficients and Pearson’s correlation coefficients were calculated to measure the reliability and validity of the instruments, respectively. Analysis of variance (ANOVA) was used to determine any significant correlations between patient satisfaction and nurse-patient communication and differences according to demographic factors such as sex, marital status, educational level, and age.
3.5. Ethical Considerations
Ethical considerations were strictly adhered to, including approval from the Research Ethics Committee at the Directorate of Health Affairs in the Jeddah region (approval number: A01712), obtaining informed consent, and maintaining participant confidentiality.
4. Results
4.1. Demographic Information
4.1.1. The Demographic Information of the Patients
Table 4 shows that most of the study participants were male (56.1%), and the majority were married (59.1%). In terms of educational background, a large proportion of patients held a bachelor’s degree (41.1%), followed by those with a secondary education (33.2%). Regarding their ED visits, over one-third (34.2%) had a length of stay between 5 and 6 hours, and 31.7% had only one hospital admission in the last two years.
| Characteristics | No. (%) |
|---|---|
| Sex | |
| Male | 225 (56.1) |
| Female | 176 (43.9) |
| Marital status | |
| Married | 237 (59.1) |
| Single | 122 (30.4) |
| Widowed | 29 (7.2) |
| Divorced | 13 (3.2) |
| Educational level | |
| Illiterate | 30 (7.5) |
| Primary education | 52 (13.0) |
| Secondary education | 133 (33.2) |
| Bachelor’s degree | 165 (41.1) |
| Other | 21 (5.2) |
| Length of stay in the ED (h) | |
| 1 - 2 | 36 (9.0) |
| 3 - 4 | 117 (29.2) |
| 5 - 6 | 137 (34.2) |
| > 6 | 111 (27.7) |
| Number of hospital admissions in the last 2 years | |
| 1 | 127 (31.7) |
| 2 | 109 (27.2) |
| 3 | 75 (18.7) |
| > 3 | 90 (22.4) |
Patients’ Demographic Characteristics
4.1.2. The Demographic Information of the Nurses
Table 5 displays that most of the nurses in this study were female (93.3%), single (65.0%), and held a bachelor’s degree (86.3%). More than half (56.7%) were between 21 and 30 years old, and the majority (53.3%) had 1 - 5 years of nursing experience. In terms of their roles, most (78.3%) served as staff nurses, followed by charge nurses (20.0%) and team leaders (1.7%). Table 5 provides a detailed breakdown of the nurses’ demographic characteristics.
| Characteristics | No. (%) |
|---|---|
| Sex | |
| Male | 4 (6.7) |
| Female | 56 (93.3) |
| Marital status | |
| Married | 19 (31.7) |
| Single | 39 (65.0) |
| Divorced | 2 (3.3) |
| Educational level | |
| Diploma | 3 (5.0) |
| Bachelor’s degree | 52 (86.3) |
| Master’s degree | 5 (8.7) |
| Age (y) | |
| 21 - 30 | 34 (56.7) |
| 31 - 40 | 21 (35.0) |
| 41 - 50 | 5 (8.3) |
| Total years of nursing experience (y) | |
| 1 - 5 | 32 (53.3) |
| 6 - 10 | 13 (21.7) |
| 11 - 15 | 8 (13.3) |
| > 15 | 7 (11.7) |
| Current nursing position | |
| Staff Nurse | 47 (78.3) |
| Charge nurse | 12 (20.0) |
| Team leader | 1 (1.7) |
Nurses’ Demographic Characteristics
4.2. Patient Satisfaction
4.2.1. La Monica Oberst Patient Satisfaction Scale Scores
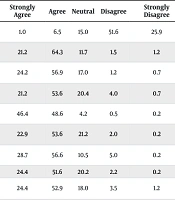
Table 6 shows that the patients were satisfied with nursing care (3.80 ± 0.44). The item “The nurse treats me with respect” was notable, with a mean score of (4.40 ± 0.62). Ninety-five percent of the patients felt valued by nurses. The patients also felt secure under the nurses, with a mean score of (4.12 ± 0.66), confirming their contentment with care. Notably, 71.8% of the patients reported that nurses provided the finest treatment, indicating satisfaction.
| Items | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | Mean ± SD | Ranking |
|---|---|---|---|---|---|---|---|
| The nurse is not as attentive as she/he should be. | 1.0 | 6.5 | 15.0 | 51.6 | 25.9 | 2.05 ± 0.87 | 15 |
| It is pleasant to have a nurse around. | 21.2 | 64.3 | 11.7 | 1.5 | 1.2 | 4.03 ± 0.72 | 6 |
| The nurse appears to be skillful at her/his work. | 24.2 | 56.9 | 17.0 | 1.2 | 0.7 | 4.02 ± 0.73 | 7 |
| The nurse showed me how to follow my treatment program. | 21.2 | 53.6 | 20.4 | 4.0 | 0.7 | 3.91 ± 0.80 | 13 |
| The nurse treats me with respect. | 46.4 | 48.6 | 4.2 | 0.5 | 0.2 | 4.40 ± 0.62 | 1 |
| I can share my feelings with the nurse when I need to talk. | 22.9 | 53.6 | 21.2 | 2.0 | 0.2 | 3.97 ± 0.74 | 9 |
| I am sure that I can get physical assistance from a nurse when I need it. | 28.7 | 56.6 | 10.5 | 5.0 | 0.2 | 4.09 ± 0.75 | 3 |
| The nurse understandably explains things. | 24.4 | 51.6 | 20.2 | 2.2 | 0.2 | 3.97 ± 0.78 | 11 |
| The nurse gives the impression that care is the top priority. | 24.4 | 52.9 | 18.0 | 3.5 | 1.2 | 3.96 ± 0.82 | 12 |
| The nurse gives the impression that my care is the top priority. | 27.7 | 56.4 | 13.2 | 1.5 | 0.2 | 4.09 ± 0.72 | 4 |
| I feel free to ask questions. | 24.2 | 57.4 | 16.2 | 1.7 | 0.5 | 4.03 ± 0.72 | 5 |
| The nurse does not consider my opinions and preferences regarding plans for my care. | 3.5 | 8.2 | 20.0 | 53.1 | 15.2 | 2.32 ± 0.95 | 14 |
| If I needed nursing care again, I would want to come back to this hospital. | 23.9 | 56.6 | 16.0 | 1.7 | 0.7 | 4.00 ± 0.76 | 8 |
| The nurse responds to my call signal promptly enough. | 28.4 | 46.9 | 18.5 | 5.5 | 0.7 | 3.97 ± 0.87 | 10 |
| The nurse makes me feel secure when giving care. | 26.9 | 60.1 | 11.7 | 2.0 | 0.2 | 4.12 ± 0.66 | 2 |
| Overall mean score | - | - | - | - | - | 3.80 ± 0.44 | - |
La Monica Oberst Patient Satisfaction Scale Scores
The patients scored (4.09 ± 0.75) on the item “I am sure that I can get physical assistance from a nurse when I need it,” indicating timely assistance. The item “The nurse gives the impression that my care is the top priority” had a mean score of (4.09 ± 0.72), indicating that most patients thought their care was prioritized. The mean score of (4.03 ± 0.72) for the item “I feel free to ask questions” showed that the patients felt free to ask questions and were satisfied with nurses’ respect and communication. Most patients found having a nurse around reassuring, scoring (4.03 ± 0.72).
The item “The nurse appears to be skillful at her/his work” had a mean score of (4.02 ± 0.73), indicating that most patients thought nurses were skilled. The patients’ attitudes toward returning to the hospital for future care were good, with a mean score of (4.00 ± 0.76). The item “I can share my feelings with the nurse when I need to talk” had a significantly lower mean score of (3.97 ± 0.74), but it still showed that most patients felt comfortable discussing their thoughts with nurses.
Conversely, the item “The nurse does not consider my opinions and preferences regarding plans for my care” yielded a low mean score of (2.32 ± 0.90), showing that many patients felt their opinions were not considered. The item “The nurse is not as attentive as (s)/he should be” earned a mean score of (2.05 ± 0.87), with 77.5% of the patients not satisfied with nursing staff attention.
4.3. Nurse-Patient Communication
4.3.1. Nurse Quality of Communication with Patient Questionnaire Scores
Table 7 depicts the nurses’ perspectives on patient communication. Most nurses thought that they communicated well with patients (3.84 ± 0.82). Approximately 45% of the nurses rated their drug administration and monitoring communication as excellent (4.20 ± 0.84), with 76.7% agreeing. The majority indicated that they completely understood their patients’ illnesses, rating their communication as excellent based on patients’ gestures (4.00 ± 0.90); 71.6% of the nurses supported this evaluation.
| Items | Excellent | Very Good | Good | Fair | Poor | Mean ± SD | Ranking |
|---|---|---|---|---|---|---|---|
| The patient shows interest in the hospital regimen and lifestyle during the conversation with me. | 23.3 | 23.3 | 41.7 | 6.7 | 5.0 | 3.53 ± 1.08 | 6 |
| The patient accepts and understands my presence related to his/her illness as: | 28.3 | 23.3 | 33.3 | 10.0 | 5.0 | 3.60 ± 1.15 | 5 |
| My level of communication with the patient during care procedures can be concluded as: | 35.0 | 20.0 | 44.7 | 8.3 | 5.0 | 3.72 ± 1.18 | 4 |
| My level of communication with the patient during care procedures can be concluded as: | 33.3 | 33.3 | 31.7 | 1.7 | 0.0 | 3.98 ± 0.85 | 3 |
| My communication with the patient while administering or monitoring medication seems to be: | 45.0 | 31.7 | 21.7 | 1.7 | 0.0 | 4.20 ± 0.84 | 1 |
| I fully understand the severity of the patient’s illness. Therefore, only by observing the patient’s gestures, I conclude that my communication with him/her is: | 33.3 | 38.3 | 14.0 | 1.7 | 1.7 | 4.00 ± 0.90 | 2 |
| Overall mean score | - | - | - | - | 3.84 | 0.82 | - |
Nurse Quality of Communication with Patient Questionnaire Scores
The nurses rated their communication during care procedures as extremely good, with a mean score of (3.98 ± 0.85). In this scenario, 66.6% and 33.3% rated their communication as outstanding, respectively. The nurses thought that patients accepted and recognized their presence concerning the condition, with a mean score of (3.60 ± 1.15). They also observed that patients showed interest in the hospital regimen and lifestyle during conversations (3.53 ± 1.08), with 41.7% rating this engagement as positive.
4.4. Relationship Between Nurse-Patient Communication and Patient Satisfaction and Differences According to Demographic Characteristics
There is no significant association between nurse-patient communication and patient satisfaction. Pearson’s correlation coefficient was -0.08 (P = 0.56), indicating a non-significant relationship.
4.5. Difference in Patient Satisfaction According to Patient Demographic Characteristics
The t-test revealed that female patients were more satisfied with nursing care than male patients, indicating that sex significantly influenced patient satisfaction. Similarly, a higher educational level significantly affected patient satisfaction. In contrast, marital status did not significantly impact patient satisfaction.
4.6. Difference in Nurse-Patient Communication According to Nurse Demographic Characteristics
The t-test showed no significant difference in nurse-patient communication between male and female nurses, indicating that sex did not significantly impact nurse-patient communication. However, ANOVA revealed that only age and marital status were significantly associated with nurse-patient communication. The nurses’ age and marital status significantly influenced nurse-patient communication, with older and married nurses reporting a higher quality of communication
5. Discussion
This study indicated a notable patient satisfaction level with a generally positive perception of the quality of nursing care provided in the ED. This result aligns with previous reports highlighting the positive impact of nursing care on patient satisfaction (23). The research showed that using nursing theories, like Peplau's interpersonal relations theory, which includes four stages: Orientation, identification, exploitation, and resolution, ensures that patients feel understood and supported, leading to greater satisfaction with their nursing care (24).
Studies have shown that effective nursing care, characterized by respect, attentiveness, and clear communication, significantly affects overall patient satisfaction. According to Ratna Sari et al. (23), effective communication is significantly associated with excellent service quality and increased patient satisfaction with healthcare. In contrast, the present study found no significant relationship between nurse-patient communication and patient satisfaction.
Several factors can be attributed to the lack of a significant correlation between nurse-patient communication in the ED and patient satisfaction. A key factor is the chaotic and rapid dynamics of the ED setting, which frequently obstructs clear communication. The presence of noise and unpredictability poses significant challenges for nurses, hindering their ability to foster meaningful interactions with patients and ultimately impacting the quality of communication (25).
Furthermore, the intricate nature of communication in the ED is intensified by the varied needs and expectations of patients. Patients exhibit diverse preferences when it comes to communication styles, and what meets the needs of one individual may not necessarily meet the needs of another. This variability may weaken the overall relationship between communication and satisfaction (26). Also, although nurses may exhibit caring behaviors, they may not consistently result in perceived satisfaction if patients do not feel sufficiently informed or engaged in their care choices (27).
Further consideration is the possible disparity between the communication abilities of nurses and the particular requirements of patients, which may result in unfulfilled expectations (28). In this study, patient satisfaction was significantly related to educational level and sex, with greater satisfaction reported among female patients and patients with higher educational levels. This finding aligns with existing evidence suggesting that educated patients have higher expectations regarding their care and are more likely to articulate their needs and preferences (29).
Approximately 95% of the patients in this study confirmed that nurses treated them with respect, indicating that nearly all patients felt respected by nursing staff. According to Karaca and Durna (30), nurses generally adopt a communication style that is respectful and friendly toward patients. However, nurses tend to be less interested in providing explanations about their interventions and communicating with patients who do not meet their expectations. In the current study, the patients indicated receiving the best possible care from their nurses, highlighting their overall satisfaction.
Respectful nurse-patient communication reduces the likelihood of miscommunication, makes patients feel secure during nursing care, enhances patient participation in decision-making, improves adherence to medication and treatment plans, increases safety, and enhances patient satisfaction with care. Therefore, good nurse-patient clinical communication is essential for improving patient-centered care and achieving favorable healthcare outcomes. The results of this study are aligned with those from other studies conducted in a similar direction (31).
Molina-Mula and Gallo-Estrada (32) conducted in-depth interviews to examine the implications of the nurse-patient relationship for clinical practice, care quality, and patient decision-making ability. They found that positive nurse-patient interaction shortened hospital stays and enhanced care quality and satisfaction. Additionally, the patients’ submissive role was a prerequisite for a positive relationship. Based on the findings, the nurse-patient relationship should not aim to alter patients’ beliefs or practices; instead, nurses should act as observers of patients’ and their families’ experiences with the health and illness processes.
Yoo et al. (33) conducted focus group discussions and in-depth interviews to evaluate the communication experiences of critical care nurses in an intensive care unit. They identified three key themes: Dealing with unforeseen communication challenges, acquiring skills through trial and error, and recognizing the importance of communication experiences in providing care. Nurses acknowledged that effective communication is essential for delivering high-quality treatment. The results, aligning with those of the present study, emphasized that nurses should continuously strive to develop new communication skills and improve their existing abilities when interacting with patients and their caregivers.
In the current study, the majority of the nurses reported that their communication with patients during care procedures was generally good. This finding is supported by previous reports suggesting that effective communication in the ED may not always be feasible due to the immediate demands of emergency treatment procedures and the need for external ventilation support (34, 35). Furthermore, prior research indicates that nurses may often prioritize task-oriented care over engaging in conversations with patients, families, and caregivers (36).
There are limitations to this study, including: The cross-sectional design of this study, along with the reliance on convenience sampling, may have led to potential bias, which could restrict the generalizability of the results. Furthermore, the study did not thoroughly examine the relationships between demographic variables (such as sex, age, marital status, and educational level) and nurse-patient communication, which may serve as confounding factors affecting patient satisfaction. Also, using only ANOVA without multivariate regression analysis made it harder to deal with these factors that could affect the results and fully understand how they affected the results.
5.1. Conclusions
Effective communication is essential for achieving positive patient satisfaction; however, this study did not find a direct relationship between nurse-patient communication and patient satisfaction, highlighting the multifaceted and complex nature of care. Demographic factors, such as educational level and gender, significantly influence patient satisfaction and should be considered in tailoring communication strategies. Healthcare organizations should prioritize enhancing nurses’ communication skills through targeted training, reducing workload, and fostering supportive work environments.
Future studies should address these gaps by exploring the interplay between demographic and confounding factors, employing advanced statistical techniques such as multivariate regression, conducting longitudinal research, and utilizing qualitative methods like interviews or focus groups to provide deeper insights into communication challenges and patient preferences.