1. Background
Pre-eclampsia (PE) is a leading cause of maternal and neonatal mortality, with a prevalence of 2% - 7% across high- and low-to-middle-income countries (1-4). It is categorized into early-onset pre-eclampsia (EOPE) and late-onset pre-eclampsia (LOPE), occurring in a 1: 6 ratio. This condition is characterized by the onset of clinical signs and symptoms and delivery before (EOPE) or after (LOPE) 34 weeks of gestation. Early-onset pre-eclampsia is associated with higher maternal and neonatal morbidity and mortality rates compared with LOPE (1-3). Neonates born to mothers with EOPE are at greater risk of respiratory distress, asphyxia, and prolonged hospital stays compared with those born to mothers with LOPE (1, 5-7). Additionally, women with EOPE are more likely to experience severe complications, such as hemolysis, elevated liver enzymes, low platelet count (HELLP syndrome), antepartum hemorrhage, cardiovascular disease, and organ dysfunction. By contrast, LOPE is typically associated with prolonged maternal care due to various complications (8).
The risk factors for PE include personal behaviors, lifestyle, environmental exposure, and hereditary traits (9). Three systematic reviews have identified 17 risk factors for PE (9, 10). Prevention of PE, particularly among high-risk individuals, can significantly reduce maternal and fetal morbidity and mortality during pregnancy or outside of pregnancy (11). Midwives play a crucial role in preventing PE by identifying these risk factors in primary healthcare settings. However, insufficient knowledge and skills among midwives remain a major barrier to effective PE management (12-14). Midwives worldwide often lack sufficient knowledge regarding various aspects of PE diagnosis and management (15). To address this gap, training policies should incorporate non-traditional approaches that enhance midwives’ knowledge. Continuous and impactful training in power-implemented health is essential to improve knowledge and skills in the management of PE (16-20). In Indonesia, existing policies promote the screening of PE risk factors among primary care physicians (20, 21).
2. Objectives
The present study aimed to evaluate the improvement in knowledge among midwives after receiving training in EOPE risk factor screening within primary healthcare settings as part of broader preventive efforts.
3. Methods
3.1. Research Design
This quantitative study used a quasi-experimental, one-group pretest-posttest design to examine the differences in midwives’ knowledge of EOPE risk factor screening before and after training.
3.2. Setting and Samples
This study was conducted at 40 public health centers in Banyumas city, Central Java, Indonesia, in October 2021. The target study population comprised all midwives employed at these health centers. Midwives with more than 5 years of professional experience and who were willing to participate in the study were enrolled. The minimum sample size of 85 participants was determined using the formula for categorical pair comparison (confidence interval 95% with power 80%). A non-probability consecutive sampling technique was utilized for participant recruitment (21).
Where:
n: Minimal sample
Zα: Confidence interval 5% = 1.96
Zβ: Beta standard values 20% = 0.84
P1: The proportion of knowledge on measurement of knowledge before training = (P2 - 0.20) = 0.657
Q1: 1 - P1 = 1 - 0.657 = 0.343
P2: Proportions on measurement knowledge after training, based on a previous study (22) = 0.857
Q2: 1 - P2 = 1 - 0.857 = 0.143
P1 - P2: The minimum difference in knowledge considered meaningful between before and after the training was set by = 0.20
3.3. Intervention
The intervention administered to the participants consisted of training on EOPE risk factor screening. A paper and case-based learning approach was used as the instructional method. The training covered several key topics, including definition, pathophysiology, signs and symptoms, maternal and infant complications, risk factor screening, and EOPE preventive management. The training was delivered in two sessions: The provision of instructional material (first day) and case-based learning (second day). Each session began with a lecture by the instructor, followed by a discussion of the corresponding material or case. For the case-based learning component, cases were drawn from the Maternal and Child Health Handbook (23).
3.4. Measurement and Data Collection
After the participants agreed to enroll in the study, an interview was conducted to gather demographic data, including age, education, work experience, and workplace. After filling out the demographic questionnaire, the EOPE questionnaire was administered. This questionnaire comprised 34 items: Definition (3 questions), pathophysiology (1 question), complications (4 questions), risk factors (16 questions), decision making (2 questions), and preventive management (9 questions). The questions were structured in a closed format with two response options: Yes or no. Each correct answer was assigned a score of 1. The assessment score was calculated by dividing the number of correct answers by 34 and multiplying the result by 100. The resulting scores were classified as good (if the correct answers exceeded 80 points) and poor (if the correct answers fell below 80 points).
3.5. Data Analysis
Categorical descriptive analyses were conducted using numbers and percentages to characterize the population. Changes in midwives’ knowledge before and after training were assessed using the McNemar test, with the significance level set at a P-value of < 0.05. The Wilcoxon test was used to evaluate improvements across specific criteria in the questionnaire, with the significance level set at a P-value of < 0.05. Data analysis was performed using SPSS version 29.
3.6. Ethical Considerations
The study was reviewed and approved by the Research Ethics Committee of the Faculty of Medicine, Padjadjaran University, Bandung (847/UN6.KEP/EC/2021). This study was conducted in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All participants provided written informed consent.
4. Results
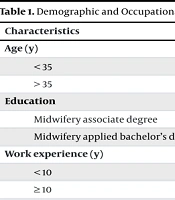
Eighty-five midwives participated in the training intervention. Table 1 outlines the demographic and professional characteristics of the participants. As indicated in Table 2, there was a significant increase in the number of midwives who demonstrated good knowledge after the training (P < 0.001). Table 3 presents detailed improvements across specific knowledge criteria. Midwives showed significant improvement in knowledge regarding EOPE pathophysiology (P ≤ 0.05) and in recognizing critical risk factors such as diabetes mellitus, multiparity with a new partner, maternal age ≥ 35 years, obesity, and elevated mean arterial pressure (MAP). Additionally, knowledge of preventive management also improved significantly, particularly regarding early screening for risk factors before 20 weeks of gestation and primary prevention experience (P ≤ 0.05). However, no significant improvement was observed in knowledge related to twin pregnancies or preventive therapy (P > 0.05).
| Characteristics | No. (%) |
|---|---|
| Age (y) | |
| < 35 | 30 (35.3) |
| > 35 | 55 (64.7) |
| Education | |
| Midwifery associate degree | 79 (92.9) |
| Midwifery applied bachelor’s degree | 12 (14.1) |
| Work experience (y) | |
| < 10 | 19 (22.4) |
| ≥ 10 | 66 (77.6) |
| Workplace | |
| Public health | 40 (47.1) |
| Community | 45 (52.9) |
Demographic and Occupational Characteristics of Participants (n = 85)
| Knowledge | Before | After | P-Value |
|---|---|---|---|
| Good | 35 (41.2) | 84 (98.8) | < 0.001 a |
| Deficient | 50 (58.8) | 1 (1.2) |
Comparison of Midwives’ Knowledge Level Regarding to Early Onset Preeclampsia Risk Factors Before and After Training (n = 85)
| Criteria | Correct Answers | ||
|---|---|---|---|
| Before Training; No. (%) | After Training; No. (%) | P-Value | |
| Pathophysiology | 42 (49.4) | 80 (94.1) | < 0.001 a |
| Risk factors | |||
| Pregnant with twins | 77 (90.6) | 80 (94.1) | 0.405 |
| Diabetes mellitus | 65 (76.5) | 82 (96.5) | < 0.001 a |
| Renal disease | 71 (83.5) | 79 (92.9) | 0.059 |
| Autoimmune conditions, SLE | 48 (56.5) | 79 (92.9) | < 0.001 a |
| APS | 50 (58.8) | 83 (97.6) | < 0.001 a |
| Multiparity with a new partner | 73 (85.9) | 85 (100) | 0.001 a |
| Pregnancy with assisted reproduction | 46 (54.1) | 84 (98.8) | 0.008 a |
| Age ≥ 35 years | 69 (81.2) | 80 (94.1) | < 0.001 a |
| Nulliparity | 41 (48.2) | 84 (98.8) | 0.005 a |
| Pregnancy interval > 10 years | 68 (80.0) | 81 (95.3) | < 0.001 a |
| Pre-pregnancy obesity/Body Mass Index > 30 | 72 (84.7) | 81 (95.3) | < 0.001 a |
| MAP ≥ 90 | 67 (78.8) | 85 (100) | 0.003 a |
| Proteinuria | 68 (80.0) | 81 (95.3) | 0.132 |
| Preventive management | |||
| Risk factor screening before 20 weeks of gestation | 76 (89.4) | 81 (95.3) | 0.013 a |
| Preventive therapy | 74 (87.1) | 83 (97.6) | 0.655 |
| Primary prevention of PE | 82 (96.5) | 83 (97.6) | < 0.001 a |
Comparison of Midwives’ Knowledge About Early Onset Preeclampsia Criteria Before and After Training (n = 85)
Before training, knowledge of autoimmune conditions (systemic lupus erythematosus) and antiphospholipid syndrome, assisted reproductive pregnancies, and nulliparity was relatively low (< 60%) compared with other areas. Post-training results also indicated a notable increase in knowledge in these areas (P < 0.05).
5. Discussion
This study demonstrated the effectiveness of training midwives on understanding EOPE risk factors. These results extend previous findings that midwives need health promotion training for PE (24). It is consistent with studies in several countries showing that midwives’ knowledge about PE management can be improved (25, 26). Case-based learning was employed to bridge theory and practice, focusing on two core topics: The pathophysiology of risk factors and preventive management. Case-based learning is an inquiry-based pedagogical approach that prepares students for clinical practice through the use of authentic cases. The implementation of this method can enhance student learning by promoting the acquisition and application of knowledge in patient assessment and problem-solving (27, 28). This study demonstrated that this method enhanced the midwives’ knowledge and assessment of risk factors and supported problem-solving efforts in the prevention of EOPE.
The effectiveness of case-based learning varies depending on the modality used — paper-based and video-based. Video case studies provide a more holistic perspective on labor and delivery care, incorporating psychosocial factors and centering on the experiences of women and their families. By contrast, paper-based case studies tend to emphasize biomedical assessments, offering a more clinically focused learning experience for healthcare providers (29). The paper-based case technique used in this study effectively strengthened participants’ understanding of the pathophysiology associated with several key risk factors. However, certain areas such as the pathophysiology of twin pregnancy, renal disease, and proteinuria were poorly understood. Similarly, knowledge related to preventive therapy did not show significant improvement. This may be attributed to less innovative instructional methods or insufficiently intensive mentorship relationships. Research suggests that incorporating video content can provide additional psychomotor benefits for learners (30).
This study has some limitations. The sample size of 85 participants in this one-group pretest-posttest design was relatively large for the minimal requirement, but there is no comparison with a control group. Additionally, the study focused on participants from a single district encompassing 40 community health centers, which restricts the generalizability of the findings. Additional limitations included the absence of a random sampling method and the lack of long-term follow-up. Future studies should involve larger, more diverse samples across multiple regions to enhance the applicability of the results.
5.1. Conclusions
This study assessed the changes in midwives’ knowledge before and after training on EOPE risk factor screening. The results indicated a significant improvement in midwives’ knowledge, particularly in understanding the pathophysiology of EOPE and preventive management strategies, early screening, and primary prevention. These results suggest that targeted case-based learning training in EOPE risk factor screening can improve the accuracy of EOPE screening in primary care settings. Prompt recognition and intensive interventions may reduce the risk of complications.