1. Background
Type 2 diabetes (T2D) is a chronic metabolic disorder characterized by insulin resistance, impaired insulin secretion, and elevated blood glucose levels, driven by a complex interplay of genetic, environmental, and lifestyle factors (1). It requires lifelong management to prevent severe complications, including cardiovascular disease, neuropathy, retinopathy, and kidney failure, which significantly impact morbidity and mortality (2). Globally, T2D affects approximately 537 million adults, with projections estimating a rise to 783 million by 2045 (3). Women face unique risks, including a higher incidence of T2D-related complications and greater challenges in achieving glycemic control compared to men (4). These disparities are attributed to physiological differences, such as hormonal influences, and social factors, including caregiving responsibilities (5).
The burden of T2D is multifaceted, encompassing physical, psychological, and economic dimensions. Physically, T2D increases the risk of cardiovascular mortality by 1.5 - 2 times and reduces life expectancy by 5 - 10 years, particularly in women (6). Complications such as diabetic neuropathy and retinopathy contribute to disability and reduced functional status. Psychologically, T2D is associated with elevated rates of depression, anxiety, and diabetes distress, affecting up to 40% of patients and impairing self-management behaviors (7). Economically, T2D incurs global healthcare costs of approximately $412.9 billion annually, driven by hospitalizations, medications, and management of complications (8). Women with T2D face a disproportionate burden, with higher rates of emotional distress and lower adherence to treatment regimens compared to men, often due to gender-specific stressors.
Beyond physical and economic impacts, T2D poses significant psychosocial challenges. Diabetes distress, defined as the emotional burden of managing a chronic condition, affects up to 40% of individuals with T2D and is linked to poor glycemic control, reduced medication adherence, and lower quality of life (9). Women report higher levels of distress, driven by factors such as societal expectations, caregiving roles, and body image concerns related to weight gain or insulin use. Quality of life is further compromised, with T2D patients experiencing reduced physical functioning, social engagement, and overall well-being compared to healthy populations (10).
Spiritual well-being, encompassing a sense of purpose, meaning, or connection to a higher power, has emerged as a potential protective factor against these challenges. Studies suggest that spiritual practices, such as mindfulness or prayer, may reduce stress, enhance coping, and improve health outcomes in chronic illnesses (11). However, the specific role of spirituality in T2D management, particularly among women, remains underexplored. Emerging evidence indicates that spirituality-based interventions, which foster meaning, hope, and resilience, can reduce distress and improve quality of life in chronic illness populations (12). Mindfulness-based interventions with spiritual components have shown promise in reducing stress and improving self-efficacy in diabetes management.
However, few randomized controlled trials (RCTs) have rigorously evaluated spirituality-based interventions in women with T2D, a population with distinct needs due to higher rates of distress and lower treatment adherence (13). Existing studies are limited by small sample sizes, lack of robust control groups (e.g., routine care), or reliance on non-validated measures of spiritual well-being and diabetes-specific outcomes (14, 15). Moreover, the mechanisms by which spiritual well-being may influence T2D outcomes, such as through reduced distress or enhanced coping, remain poorly elucidated, particularly in gender-specific contexts.
2. Objectives
This study aimed to evaluate the efficacy of a 12-week spirituality-based intervention compared to routine care in reducing diabetes distress (primary outcome), improving spiritual well-being, and enhancing quality of life (secondary outcomes) among women with T2D.
3. Methods
3.1. Study Design
This study was a two-arm, parallel-group RCT conducted to evaluate the efficacy of a spirituality-based intervention compared to routine care in improving symptoms among women with T2D. Participants were randomized 1:1 to either the intervention group or the control group. Assessments were conducted at baseline, immediately after the 12-week intervention, and at a 1-month follow-up.
3.2. Participants
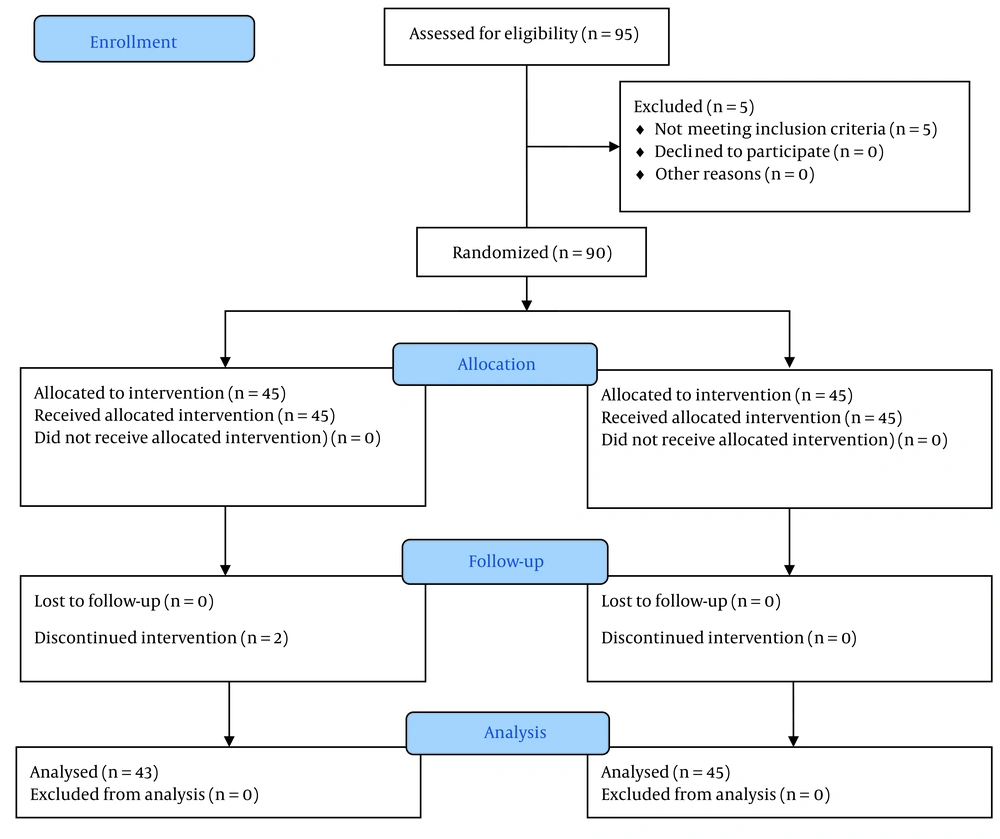
Participants were recruited from a single outpatient clinic in Bandar Abbas, Iran, between November 2024 and May 2025 using an accessible sampling method. Recruitment strategies included distributing flyers, obtaining physician referrals, and screening electronic medical records to identify eligible women. A total of 90 participants were initially enrolled, with 88 completing the study (intervention: n = 43; control: n = 45) after accounting for attrition. Figure 1 shows the process of the study.
Eligible participants were women aged 18 - 75 years diagnosed with T2D (confirmed by medical records or physician diagnosis) for at least 6 months. Inclusion criteria included: (1) Ability to provide informed consent, (2) fluency in the Persian language, and (3) willingness to participate in group-based sessions (for the intervention group) or routine care. Exclusion criteria were: (1) severe psychiatric disorders (e.g., schizophrenia, bipolar disorder), (2) significant cognitive impairment (e.g., dementia), (3) participation in other diabetes-related intervention studies, or (4) major medical comorbidities precluding participation (e.g., advanced heart failure).
3.3. Randomization and Blinding
Participants were randomized using a computer-generated random number sequence with permuted block randomization (block size = 4) to ensure balanced allocation. The randomization sequence was concealed in sealed, opaque envelopes until assignment. Outcome assessors and data analysts were blinded to group assignment to minimize bias. Participants and intervention facilitators were not blinded due to the nature of the interventions.
3.4. Interventions
3.4.1. Intervention Group
The intervention group received a 12-week, group-based spirituality intervention designed to enhance spiritual well-being and improve T2D symptoms. Weekly 90-minute sessions, delivered at the outpatient clinic in Bandar Abbas, Hormozgan, were facilitated by research team members with specialized training in spiritual care and behavioral health. The intervention was grounded in the biopsychosocial-spiritual model, aiming to foster spiritual coping and resilience alongside T2D self-management.
The intervention was designed to ensure consistency, with a detailed protocol outlining session content, facilitator scripts, and participant materials. Fidelity was monitored by recording all sessions and reviewing 10% of recordings by an independent auditor to confirm adherence to the protocol. Participants received workbooks and access to recorded mindfulness sessions to support engagement. More details regarding the content of the sessions are provided in Table 1.
| Weeks | Session Components | Topics Covered/Activities |
|---|---|---|
| Week 1 | Introduction and orientation | Overview of program goals and structure; introduction to mindfulness and spirituality in chronic illness; group norms and expectations |
| Week 2 | Mindfulness meditation + psychoeducation | Guided meditation on gratitude; introduction to T2D and the role of stress; spiritual principle: Self-awareness and compassion |
| Week 3 | Reflective journaling + group discussion | Journaling: “What gives your life purpose?”; group sharing on sources of hope and personal values |
| Week 4 | Mindfulness meditation + psychoeducation | Guided meditation on inner peace; T2D self-care practices (medication adherence); spiritual framing: Caring for the body as a sacred act |
| Week 5 | Journaling + group discussion | Journaling: “How do your beliefs support your diabetes management?”; discussion on faith, control, and surrender in facing illness |
| Week 6 | Meditation + psychoeducation | Meditation on connection to a higher power or purpose; nutrition and dietary management; framing dietary discipline as spiritual self-care |
| Week 7 | Group discussion + reflective journaling | Group sharing: Spiritual challenges in living with T2D; journaling on finding meaning in daily challenges |
| Week 8 | Meditation + psychoeducation | Meditation on hope and resilience; importance of physical activity; spiritual motivation to stay active |
| Week 9 | Journaling + group discussion | Journaling: “What does healing mean to you?”; group dialogue on emotional well-being, forgiveness, and spiritual acceptance |
| Week 10 | Meditation + psychoeducation | Meditation on self-compassion; addressing emotional eating and body image; integrating faith/spirituality with emotional regulation |
| Week 11 | Reflective journaling + group sharing | Journaling: “What spiritual practices help you cope?”; peer encouragement and community-building through shared practices |
| Week 12 | Integration + closing | Final meditation on gratitude and connection; recap of key spiritual and self-management lessons; commitment statements and farewell sharing |
Weekly Structure of the 12-Week Spiritual Mindfulness Intervention for Women with Type 2 Diabetes
3.4.2. Control Group
The control group received routine care, consisting of standard medical management for T2D as provided by their healthcare providers. This included regular physician visits, medication management, and access to usual care resources (e.g., dietary counseling, glucose monitoring) without additional structured group sessions or spiritual components. To ensure ethical treatment, control participants were offered the opportunity to join the spirituality intervention after study completion.
3.5. Outcome Measures
Data were collected at baseline, immediately after the intervention (12 weeks), and at a 1-month follow-up using validated self-report questionnaires administered by blinded assessors. All instruments underwent validity and reliability testing in the study sample to confirm psychometric properties.
3.5.1. Demographic Characteristics
Collected at baseline, including age, marital status, education level, employment status, number of children, Body Mass Index (BMI), and T2D duration.
3.5.2. Diabetes Distress Scale
The primary outcome, a 17-item scale developed by Polonsky et al. to assess diabetes-related distress in four domains: Emotional burden (e.g., feeling overwhelmed by diabetes), physician-related distress (e.g., concerns about healthcare access), regimen-related distress (e.g., challenges with self-management), and interpersonal distress (e.g., lack of social support). Items are rated on a 6-point Likert scale (1 = not a problem, 6 = serious problem), with total scores ranging from 1 to 6 (mean score, higher values indicate greater distress) (16). A score ≥ 2.0 indicates clinically significant distress. In this study, CFA confirmed the four-factor structure (CFI = 0.95, RMSEA = 0.06), and internal consistency was high (Cronbach’s α = 0.89). Subscale reliabilities ranged from 0.82 to 0.87. Also, the scale has been used in Iran, with acceptable reliability and validity (Cronbach's alpha coefficient, McDonald omega coefficient, and ICC showed a value of 0.920, 0.928, and 0.884, respectively for all factors) (17).
3.5.3. Spiritual Well-Being Scale
A secondary outcome, a 20-item scale developed by Paloutzian and Ellison (1982) to measure spiritual well-being in two dimensions: (1) Religious well-being (connection to a higher power, 10 items); and (2) e xistential well-being (sense of purpose and meaning, 10 items). Items are rated on a 6-point Likert scale (1 = strongly disagree, 6 = strongly agree), with total scores ranging from 20 to 120 (higher scores indicate greater well-being) (18). The scale is widely used in health research for its applicability across diverse belief systems. In this study, CFA supported the two-factor structure (CFI = 0.93, RMSEA = 0.07), with excellent reliability (Cronbach’s α = 0.91 for total scale, 0.88 for religious well-being, 0.85 for existential well-being). Also, the scale has been used in Iran, with acceptable reliability and validity (Cronbach’s α greater than 0.85, significant Pearson correlation ranged from 0.33 to 0.53) (19).
3.5.4. Diabetes Quality of Life Measure
A secondary outcome, a 46-item scale developed by the Diabetes Control and Complications Trial (DCCT) Research Group (1988) to assess quality of life in T2D across three domains: Satisfaction (15 items, e.g., satisfaction with treatment), impact (20 items, e.g., interference of diabetes with daily life), and worry (11 items, e.g., concerns about complications). Items are rated on a 5-point Likert scale (e.g., 1 = very dissatisfied, 5 = very satisfied for satisfaction; 1 = never, 5 = always for impact/worry), with total scores transformed to a 0 - 100 scale (higher scores indicate better quality of life) (20). In this study, CFA confirmed the three-factor structure (CFI = 0.92, RMSEA = 0.08), and reliability was strong (Cronbach’s α = 0.90 for total scale, 0.87 for satisfaction, 0.84 for impact, 0.82 for worry). Also, the scale has been used in Iran, with acceptable reliability and validity (Cronbach's α > 0.70 and acceptable CFA) (21).
3.5.5. Sample Size Calculation
Sample size was calculated to detect a clinically meaningful difference in the primary outcome [Diabetes Distress Scale (DDS-17)] of 0.5 points between groups, based on a prior study (22) (SD = 0.8, α = 0.05, power = 80%). The formula is:
A sample of 40 participants per group was required. To account for an anticipated 10% attrition rate, 45 participants per group (total n = 90) were enrolled. After 2 participants were lost to follow-up (1 intervention, 1 control), the final sample was 88 (43 intervention, 45 control), retaining sufficient power for the primary analysis. Figure 1 shows the CONSORT flowchart.
3.6. Statistical Analysis
Baseline characteristics were compared using t-tests for continuous variables and chi-square tests for categorical variables to confirm randomization. Longitudinal changes in DDS-17, Spiritual Well-being Scale (SWBS), and Diabetes Quality of Life Measure (DQOL) were analyzed using mixed-effects linear regression, with group, time, and group × time interaction as fixed effects, participant as a random effect, and adjustments for baseline scores, age, T2D duration, and BMI. Post-hoc tests used Bonferroni correction, and effect sizes (Cohen’s d) were calculated. Mediation analysis (PROCESS macro, Model 4) assessed SWBS’s role in mediating intervention effects on DDS-17 and DQOL, using bootstrapping (5,000 iterations) for 95% confidence intervals. Missing data were handled with multiple imputation, and sensitivity analyses used complete cases. Attrition was compared using chi-square tests. Analyses were conducted in SPSS v28 (P < 0.05, two-sided).
3.7. Ethical Consideration
The study was approved by the Research Ethics Committees of Hormozgan University of Medical Sciences (IR.HUMS.REC.1403.317) and registered with IRCT20220704055367N6. All participants provided written informed consent. All participants provided written informed consent in Persian after receiving clear information about the study’s purpose, procedures, risks, benefits, and their right to withdraw at any time without affecting their care.
4. Results
The study included 88 women with T2D, randomly assigned to either the intervention (n = 43) or control group (n = 45). Baseline characteristics were well-balanced between groups, with no significant differences in age (intervention: 53.8 ± 8.5 years; control: 54.6 ± 8.9 years), diabetes duration (7.5 ± 4.0 years), marital status (65.9% married), education (70.5% ≥ high school), employment status (58.0% employed), or number of children (2.1 ± 1.2) (all P > 0.05) (Table 2).
| Variables | Intervention (N = 43) | Control (N = 45) | P-Value b |
|---|---|---|---|
| Age (y) | 53.8 ± 8.5 | 54.6 ± 8.9 | 0.64 |
| Married | 28 (65.1) | 30 (66.7) | 0.87 |
| Education ≥ high school | 31 (72.1) | 31 (68.9) | 0.73 |
| Employed | 25 (58.1) | 26 (57.8) | 0.97 |
| Number of children | 2.2 ± 1.3 | 2.0 ± 1.1 | 0.46 |
| BMI (kg/m2) | 30.2 ± 5.1 | 30.7 ± 5.3 | 0.62 |
| T2D duration (y) | 7.6 ± 4.1 | 7.4 ± 3.9 | 0.79 |
Baseline Demographic Characteristics of the Participants a
Analysis of DDS-17 revealed significant improvements in the intervention group. While both groups showed similar baseline scores (intervention: 3.0 ± 0.7; control: 3.1 ± 0.8), the intervention group demonstrated substantially lower distress immediately post-intervention (2.0 ± 0.5 vs. 2.6 ± 0.6; P < 0.001, d = 1.05) and at 1-month follow-up (2.1 ± 0.5 vs. 2.7 ± 0.7; P = 0.001, d = 0.94). Within-group analyses confirmed these reductions were significant for the intervention group (both P < 0.001) but only marginal in controls (P = 0.03 - 0.05) (Table 3).
The SWBS showed even more pronounced effects. From comparable baselines (intervention: 77.2 ± 11.8; control: 76.8 ± 12.0), the intervention group achieved significantly higher scores post-intervention (91.5 ± 10.2 vs. 79.0 ± 11.8; P < 0.001, d = 1.12) and at follow-up (89.8 ± 10.5 vs. 78.5 ± 11.9; P < 0.001, d = 1.00). Mediation analysis indicated SWBS improvements accounted for 65% of the intervention's effect on reducing diabetes distress (P < 0.001) (Table 4).
The DQOL improvements were more modest. Though the intervention group showed within-group improvements from baseline (64.5 ± 13.0) to post-intervention (70.8 ± 11.7; P = 0.02) and follow-up (69.2 ± 11.9; P = 0.04), between-group differences did not reach significance (P = 0.18 - 0.29). A trend toward greater satisfaction was observed but remained non-significant (P = 0.09) (Table 5).
The study maintained excellent retention, with comparable attrition rates between groups (intervention: 4.7%; control: 6.7%; P = 0.69). Sensitivity analyses confirmed the robustness of findings, and no adverse events were reported.
5. Discussion
This RCTs demonstrated that a 12-week spirituality-based intervention significantly reduced diabetes distress and enhanced spiritual well-being in women with T2D, with effects sustained at 1-month follow-up. The finding that spiritual well-being mediated 65% of the intervention's effect on distress reduction provides compelling evidence for the role of spirituality in improving psychological outcomes in chronic disease management, consistent with contemporary biopsychosocial-spiritual models of care.
Our results align with emerging evidence that spiritually-informed interventions can alleviate psychological distress in chronic illnesses (23). The intervention's success may be attributed to its multi-component design integrating mindfulness, reflective journaling, and group discussions — an approach that builds upon established mindfulness-based interventions for diabetes (24). The use of non-denominational themes appears particularly impactful for women, who face unique diabetes-related stressors including caregiving burdens and societal expectations (25). This gender-sensitive approach may explain our stronger effects compared to previous spirituality interventions in mixed-gender populations.
The significant improvements in spiritual well-being extend previous findings linking spiritual practices to better coping in chronic illness (26). This study's dual focus on existential purpose and transcendent connection appears to have fostered resilience — a finding supported by literature positioning spiritual well-being as protective against stress (27). The mediation analysis provides empirical support for this pathway, suggesting that enhanced spiritual well-being drives distress reduction.
The null finding for quality-of-life contrasts with some previous studies (12, 15), but may reflect important conceptual distinctions. While our intervention successfully targeted emotional and spiritual domains, quality of life encompasses broader physical and social factors that may require longer intervention periods or additional behavioral components (10). The trending improvement in life satisfaction suggests our approach may positively influence specific psychosocial domains worthy of further investigation.
The slightly higher baseline diabetes distress scores in the control group (3.1 ± 0.8 vs. 3.0 ± 0.7, P = 0.58) raised questions about potential sampling bias. However, this difference was not statistically significant, indicating it likely resulted from random variation rather than systematic bias. The study employed permuted block randomization with concealed allocation to ensure balanced group assignment, and baseline demographic characteristics were well-matched (all P > 0.05), confirming effective randomization. Furthermore, statistical analyses adjusted for baseline scores, ensuring that the minor difference did not confound the intervention’s effects. This robust methodological approach minimizes concerns about sampling bias and supports the validity of the observed outcomes.
This study makes three key contributions to the literature. First, it addresses the critical gap in gender-specific T2D interventions by focusing on women's unique psychosocial needs. The study’s focus on women addresses a critical gap in the literature, as prior research has often overlooked gender-specific needs in T2D management (22, 28). Second, it introduces an innovative, structured, gender-specific spirituality-based intervention that systematically enhances spiritual well-being through a manualized protocol integrating mindfulness, reflective journaling, group discussions, and psychoeducation with non-denominational spiritual themes, offering a replicable framework to reduce diabetes distress in women (29, 30). Third, it provides methodological advances through rigorous design elements including randomization, blinding, and validated measures — addressing limitations of prior studies with small samples or weak controls. The current study’s rigorous design, including randomization, blinding, and validated outcome measures, strengthens the evidence for spirituality-based interventions but also underscores the need for larger, multi-site trials to confirm generalizability.
5.1. Conclusions
The 12-week spirituality-based intervention significantly reduced diabetes distress and improved spiritual well-being in women with T2D, with spiritual gains partially mediating distress reduction. Although quality of life improvements were not statistically significant, trends suggest potential benefits worth further study. These results support incorporating spiritual components into diabetes management to better address psychosocial challenges in women. For clinical practice, integrating spirituality-based interventions and training providers in spiritual care may enhance holistic T2D treatment. Future research should test this approach in larger, diverse populations with active controls and longer follow-up to strengthen evidence and explore effects on physical health outcomes, ultimately improving patient-centered care.
5.2. Limitations
This RCT’s strengths include a gender-specific focus, validated outcome measures, an intervention with fidelity monitoring, low attrition, and robust analyses including mediation. Limitations include the relatively short 12-week duration, possibly limiting effects on complex outcomes like quality of life. The single-site design may reduce generalizability across diverse cultural or socioeconomic groups. The control group received routine care without an active comparator, which could overestimate intervention effects. The sample size was sufficient for primary outcomes but may have lacked power for quality of life changes. The exclusion of men limits the applicability of findings to male populations with T2D, who may experience different psychosocial challenges. Lastly, the non-denominational intervention, while inclusive, might not reflect influences of specific religious or cultural practices on diabetes outcomes.