1. Introduction
The term ‘pemphigus’ is derived from the Greek word pemphix, meaning blister or bubble. The incidence of the disease is 0.09 to 1.8% (1), usually seen in between the fourth and sixth decade of life; however, it may occur in any age group (2). It seems to affect men and women equally though some studies have suggested a slight female dominance (3, 4). Desmogleins 1 and 3 are desmosomal glycoproteins that belong to the cadherin family of calcium-dependent cell-cell adhesion molecules that contribute to the structure of the desmosomes, expressed on the epithelial cells of the skin and mucosa. Pemphigus is caused by autoantibodies directed against desmogleins (Dsgs), resulting in acantholysis.
Pemphigus vegetans is a less common variant of pemphigus vulgaris that comprises only 1% to 2% (5, 6). Pemphigus vegetans clinically manifests as heaped-up, cauliflower-like vegetating plaques commonly in flexures. This disorder affects chiefly middle-aged adults. It is caused by autoantibodies directed transmembrane glycoproteins and results in loss of intercellular adhesion between intact keratinocytes, which results in acantholysis. This disease occurs mainly on intertriginous areas, scalp, and face but may occur anywhere on the skin surface (7-9). The oral, gastrointestinal, respiratory, genital, and conjunctival mucosa can also be affected. According to the clinical manifestations, there are two subtypes: (1) the Neumann, and (2) Hallopeau subtypes. The Neumann type is characterized by bullae that extend and coalesce; later progressing to vegetating masses or plaques, which become dry, hyperkeratotic, and fissured (10).
Cerebriform tongue, a morphology with a typical pattern of sulci and gyri over dorsum of the tongue, is common in pemphigus vegetans. Approximately 50% of the cases of the Neumann type show cerebriform tongue. The Hallopeau type is characterized by a polycyclic eruption of pustules that form firm pink papillomas, which progressively flatten and change to dark brown plaques. The present case had vegetative plaques limited to lips, and the common sites like flexural and intertriginous areas were spared, making it a rare presentation.
2. Case Presentation
A 62-year-old female, hailing from a rural area, presented with the chief complaints of swelling over upper and lower lips with fissures and raw areas from two months ago. The patient also complained of oral intolerance to spicy food from two months ago. The patient was apparently alright two months back when she started developing fluid-filled lesions over upper lip, which ruptured spontaneously to form raw areas with slight swelling. The lesion gradually progressed to involve the lower lip. The lesions gradually increased in size to present size with cauliflower-like growth over both lips. The patient also complained of intolerance to spicy food from two months ago. In the past, the patient had similar lesions over lips, which resolved after treatment (details of which are not available). There was no history of intake of medication prior to the onset of symptoms.
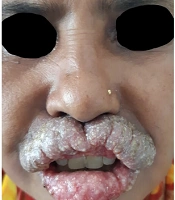
On cutaneous examination, upper lip was grossly edematous. Vegetative plaques with areas of erosions, fresh bleeding points, oozing, and yellowish crusts extending beyond the vermillion border were seen. Fissures were seen over vegetative plaques on the vermillion border of upper lip. The lower lip was also slightly edematous with vegetative plaques and erosions. Oral mucosa examination revealed erosions in the buccal mucosa (Figure 1). Examination of flexural and intertriginous areas such as axilla, groin, web spaces of feet revealed no lesions. On the basis of history and clinical examination, differential diagnoses were considered pemphigus vegetans, paraneoplastic pemphigus, granulomatous cheilitis, graft versus host disease (GVHD), pyostomatitis vegetans.
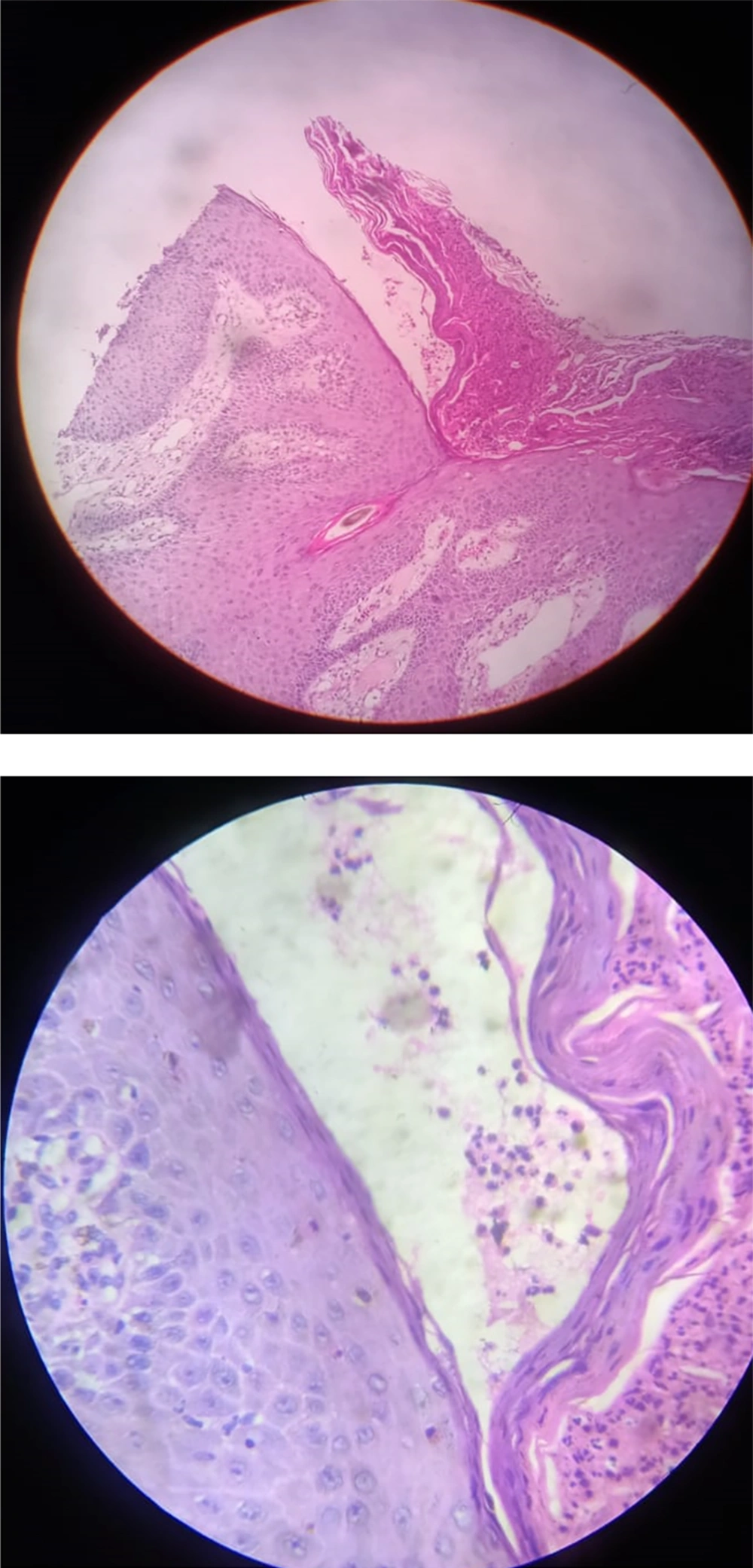
A preliminary diagnosis of pemphigus vegetans was made based on the Tzanck smear test, which revealed multiple acantholytic cells (Tzanck cells). Skin biopsy was sent for histopathological examination for confirmation. A full-thickness biopsy was taken from the vermillion border of the upper lip. Under the microscope, using hematoxylin and eosin (H&E) staining, epidermis showed hyperkeratosis with pointed rete ridges, at places showed verrucous hyperplasia. Also, a collection of polymorphonuclear (PMN) cells along with eosinophils in stratum corneum were seen and two incomplete intraepidermal suprabasal clefts filled with PMNs, eosinophils, and few acantholytic epidermal cells. Papillary dermis showed dense infiltration by PMNs along with eosinophils, and few eosinophilic round structures were noted. These histopathological features confirm the diagnosis of pemphigus vegetans (Figure 2).
Since it was a localized plaque, a decision for intralesional immunosuppressive therapy was made by the authors in order to avoid any systemic side effects of immunosuppressants in the COVID-19 pandemic period. The patient was evaluated for intralesional steroid (ILS) therapy. Her laboratory parameters, chest X-ray, USG (abdomen and pelvis) were all within normal range. Intralesional steroids (injection of triamcinolone acetonide 10 mg/mL every three weeks) were started for the patient. She responded to therapy within three injections with complete resolution of lesions and was followed up to six months with no recurrence.
3. Discussion
Pemphigus vegetans occurs mainly on intertriginous areas, scalp, and face. The present patient had vegetative plaques limited to lips, and the common sites like flexural and intertriginous areas were spared, which makes it a rare presentation. Drugs such as antihypertensives and chelating agents trigger the onset of pemphigus in some cases. This type of disease resolves after the stoppage of medication. In the present case, the patient had no history of intake of a triggering drug. A preliminary diagnosis of pemphigus vegetans was established in this case on the basis of presenting clinical features and a Tzanck smear test, which revealed multiple acantholytic cells (Tzanck cells), and then the diagnosis was confirmed by histopathology. Intertriginous areas, flexural areas, scalp face, and oral lesions are common. Other areas are very uncommonly involved; however, cases with lesions limited to foot, oral mucosa, lips, or toes have been reported rarely (11). Similar to the case reported by Dhamija, Ashish et al. (12), our case is unusual in its presentation of lesions that are limited only to the lips. The tongue, in the present case, does not show typical cerebriform pattern, which is seen in almost 50% of Neumann type cases.
The goal of the treatment is to induce complete remission while minimizing treatment-related adverse effects. Although dexamethasone cyclophosphamide pulse (DCP) therapy remains the mainstay treatment to reduce mortality and morbidity in pemphigus vegetans, (13) intralesional steroids in case of isolated lip lesions may help to reduce the morbidity of disease as well as the side effects of DCP therapy.
3.1. Conclusion
In patients presenting with vegetative plaques over lips, even though the usual sites of the disease are not involved, pemphigus vegetans as one of the differential diagnosis should be taken into consideration. Careful history taking and a high index of suspicion are helpful in reaching the correct diagnosis of a rare disease such as pemphigus vegetans, which may present in an unusual form. A simple tool such as biopsy can confirm the diagnosis in puzzling cases when a rare disease like pemphigus vegetans has a rare presentation. In a case with pemphigus vegetans limited to only one site, it may be advisable to use ILS as a conservative treatment modality to avoid systemic adverse effects of aggressive immunosuppressive therapy.