1. Introduction
Seborrheic keratosis (SK) is one of the most common non-cancerous lesions affecting millions of people worldwide. It mostly appears on the sun-exposure areas of the skin, especially the face, trunk, chest, and back. Seborrheic keratosis is the result of hyperproliferation of immature keratinocytes due to various factors like sun exposure (1, 2). Seborrheic keratosis has nine subtypes including acanthotic, reticulate, hyperkeratotic, adamantinoid, desmoplastic, pseudorosettes, clonal, irritated, and inverted follicular keratosis (3). It mostly appears with distinct clinical features but few studies reported malignant changes in SK such as sudden growth, color changes, ulcerations, scarring causing or accompanied by basal cell carcinoma (BCC), squamous cell carcinoma (SCC), keratoacanthoma, Bowen's disease, malignant melanoma, and hamartomas (4-6).
Recently, the number of SK cases with malignant changes has increased by increasing the elderly population. Darkly pigmented lesions like SK and malignant masses may overlap based on clinical manifestations. In this respect, thin SK on the face is a differential diagnosis of malignant lentigo (7). Otherwise, SK has a similar appearance with epidermal moles, condylomata, and warts (2, 8, 9).
Overall, SK may have morphological similarities with other lesions and may develop into cancerous ones. Therefore, performing histopathological investigations and subsequently appropriate treatments are necessary especially for those with high suspicion of malignancy (10, 11). This study reported an 86-year-old man with giant SK on the right flank and significant clinical changes.
2. Case Presentation
The patient was an 86-year-old man, a retired farmer, reported to the dermatologic clinic with a chief complaint of a single lesion on his right flank part, causing discomfort for him recently. The lesion was black-tan, secreting, smelly, and enlarged two-fold during the last three months. It was painless, non-pruritic, and non-hemorrhagic.
The lesion started as a small purple papule on the right flank part in the early 50s, without any secretion or smell at first. He had no history of smoking, alcohol consumption, skin burn, or allergy. There was no significant past medical and drug history. The patient did not undergo any procedure or local or systemic treatment for the aforementioned lesion before reporting to the clinic. No family history of skin disease or malignancies was reported by the patient. There was no evidence of significant weight loss. No fever was detected.
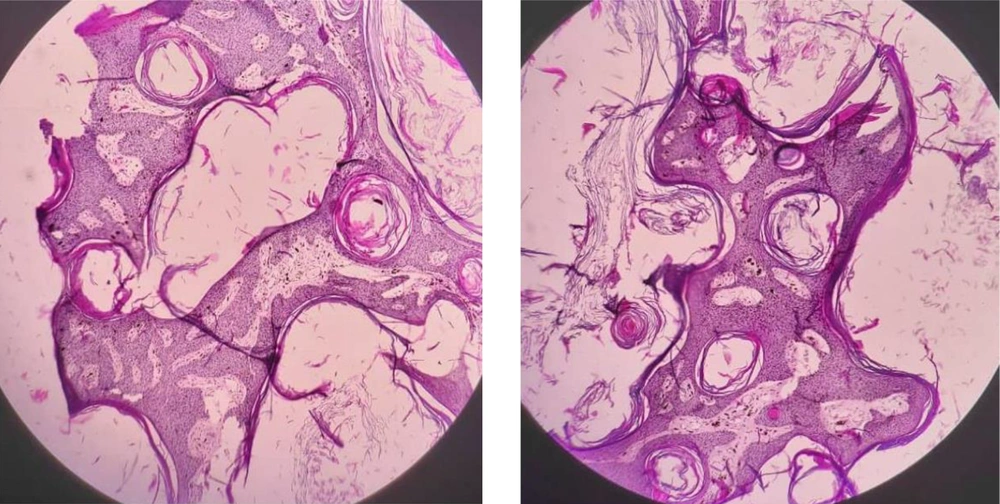
In the physical examination, there was a giant soft plaque of 91 × 65 mm, sharp margin, stuck to the skin, exhibiting a pigmented papillomatosis and verrucous surface. No evidence of cellulitis in the lesion area or further remarkable signs were examined (Figure 1). An incisional biopsy was performed with differential diagnosis of giant condyloma acuminate (Buschke-Lowenstein tumor), verrucous carcinoma, congenital nevus, and giant SK. Also, BCC or SCC arising with SK was a matter of debate. The biopsy revealed an epidermal hyperkeratosis, extensive acanthosis, and papillomatosis of the epidermis, upward growth of basaloid cells with small horn cyst formation and squamous eddies, moderate lymphocytic infiltrate in the dermis, showing irritated SK. There was no evidence of concomitant malignancy (Figure 2).
The patient underwent antibiotic therapy, cephalexin 500 mg per os every 12 hours, for one week for treating the infection. Then, the lesion was totally excised with a 2-mm normal resection margin and the defect was primarily closed, by covering with a partial thickness skin graft. The excision area was evaluated two weeks later and no primary complication like infection was observed.
3. Discussion
Seborrheic keratosis is an important and common benign skin lesion with slow growth. It has different morphological similarities and could be misdiagnosed or accompanied by several malignancies that call for great attention. Therefore, considering the size, number, thickness, location, and progression trend of SK could be helpful for further decisions (2, 3, 10-12).
Seborrheic keratosis typically did not require any treatment but uncertain diagnosis or atypical presentation of SK that carries a higher risk of malignancy, consistent irritated ones, and those causing discomfort for patients warrant histopathological investigations and treatment (10, 11). There are various treatment modalities available for SK such as topical treatment, laser therapy, cryotherapy, and shave or total excision, and physicians choose an appropriate treatment for each patient individually (2, 13).
Giant SK, an atypical SK, is rarely reported on the genitalia, perianal, or face in previous studies (14-17). However, at the time of this study, no case of giant SK was reported on the flank part. This study presented a rare case of irritated giant SK located on a non-sun-exposed body area, with rapid enlargement. The clinical manifestations were in favor of malignancy but there was no evidence of contaminant malignancy in the biopsy report. After excision, the patient underwent physical examinations every month. After one year, he had good outcomes with no recurrence or complication.
In this regard, the American Academy of Dermatology Association announced that SK lesions have a good prognosis (no return after removal) and a low recurrence rate, but still may occur elsewhere (18). Therefore, close follow-ups are necessary. In this regard, Sayan et al. showed that the recurrence rate of SK lesions was only six out of 547 cases (19).