1. Introduction
Squamous cell carcinoma (SCC) is the second most common type of skin cancer in Caucasians (1). Ultraviolet (UV) radiation is a well-established risk factor for SCC, with long-term sun exposure being its main cause (2). The relationship between SCC and ionizing radiation (IR) is less well-established. In fact, some studies report little to no relationship between the two (3-5), while others report an association only for individuals with risk factors for sun sensitivity (6). Despite this unclear connection, SCCs that arise in patients with exposure to ionizing radiation have been characterized as more aggressive and with a higher rate of recurrence and metastasis compared to those in individuals with UV-induced SCC (7, 8). This ultimately results in poorer patient prognoses among those exposed to IR (7). While most of the literature focuses on the relationship between therapeutic or atomic bomb radiation and SCC presentation, lesser-known causes of IR must also be considered.
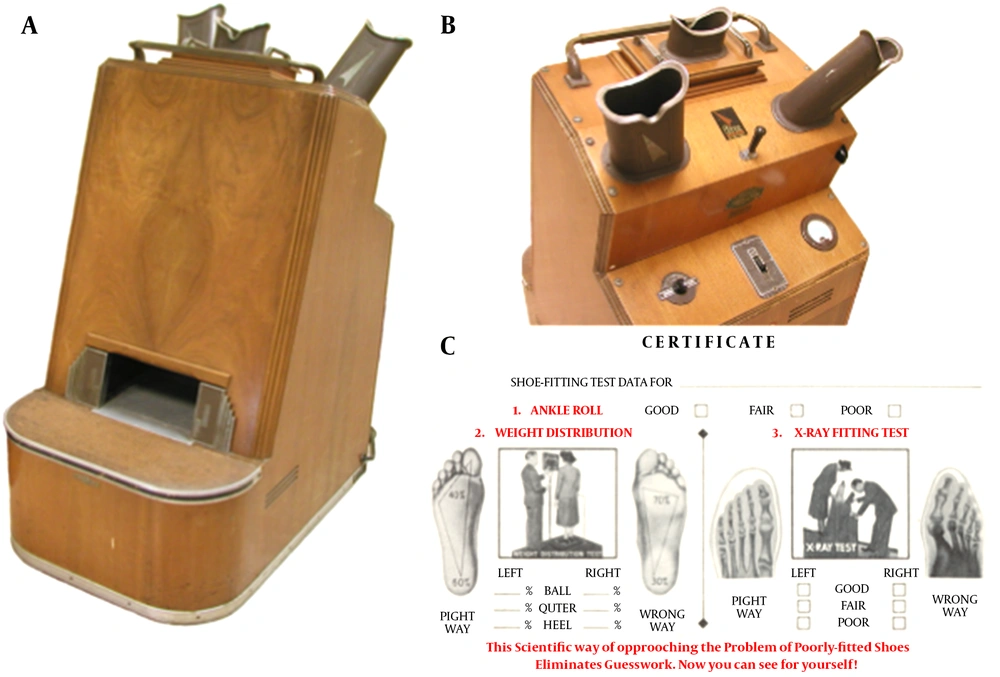
With the discovery of radium in 1898, a wide variety of products and procedures using unregulated radiation were developed in the early 20th century. The shoe-fitting fluoroscope was an invention in popular use between the 1920 - 1950’s (Figure 1A and B) (9). It used low dose X-ray beams to help shoe salesmen and customers see the bones of their feet within the outline of the shoes they were trying on10 (Figure 1C). These machines required customers to stand almost directly on the X-ray tube, but the exact degree of radiation exposure to the feet varied greatly depending on the length of shoe fitting time and the number of fittings (10). Because buying new shoes was an infrequent occurrence for most people, the average customer was at a significantly lower risk of developing fluoroscope-related radiation complications compared to shoe shop employees and customers who repeatedly used the machine over long periods of time (11).
2. Case Presentation
A 78-year-old Caucasian female presented for evaluation of a 25-year history of many scaly papules and bleeding, non-healing ulcers of her bilateral dorsal feet with associated discomfort. This patient’s history included repeated IR exposure to her feet through near daily usage of a shoe-fitting fluoroscope between the ages of 13 and 14. She described regularly visiting a childhood friend’s family-owned shoe shop and using a fluoroscope to measure her feet in different shoes as a pastime. She disclosed prior topical fluorouracil 5% cream (5-FU) treatment of actinic keratoses (AKs) on her dorsal feet by a dermatologist 22 years prior. She reported being unable to tolerate the 5-FU due to the resulting pain. As a result, cryotherapy of AKs on her dorsal feet continued in place of 5-FU treatment.
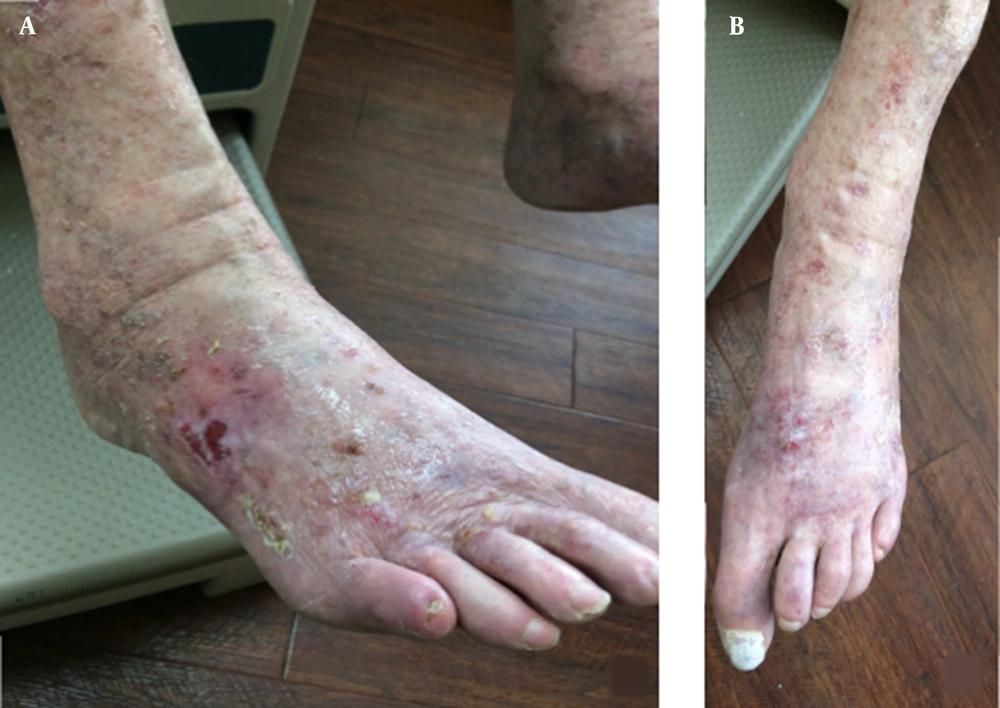
Examination of the patient’s dorsal feet showed thin, erythematous, scaled papules admixed with several painful ulcerations and patches of atrophic dyspigmentation extending to the ankle, with a sharp transition to normal appearing skin proximal to the ankle (Figure 2A and B). The scaled papules were consistent with AKs. The patient declined field treatment given her past intolerance to 5-FU, so these lesions were treated with cryotherapy. Ulcerated areas were concerning for SCC or chronic radiation dermatitis given the atrophy and dyspigmentation. The patient has previously had such lesions biopsied, with pathology demonstrating actinic keratoses, SCC in situ, and invasive SCC requiring a variety of surgical treatments. The patient denied having any skin cancers on other parts of the body, though two AKs were treated on her right dorsal hand in the past. The patient committed to close follow up with further biopsies and surgical interventions as appropriate.
3. Discussion
Ionizing radiation is a type of electromagnetic radiation of a sufficient energy to cause a change in the electrons of a molecule or atom, thus “ionizing” them. This ionization can be damaging to cellular DNA, resulting in the potential for carcinogenesis. IR includes gamma rays, X-rays, and higher frequency ultraviolet radiation. While ionizing radiation has been an accepted etiologic factor in the development of non-melanoma skin cancer (NMSC) and in cancer generally, there are surprisingly few reported cases of ionizing radiation-induced skin cancer. This may be in part due to the long delay between radiation exposure and the development of NMSC, in addition to the confounding exposure of ultraviolet radiation.
Furthermore, of the few cases reported of NMSC induced by IR, the vast majority of them are related to BCC. Upon review of the literature, there were only two cases of BCC and no cases of SCC of the feet arising in relation to shoe-fitting fluoroscope devices (9). When evaluating older patients with a potential skin cancer in an uncommon location or with unusual presentation, it is important to consider the possibility of atypical causes, such as radiation therapies and equipment exposure now known to be unsafe. For example, before the dangers of radiation were well known, x-rays were used to treat relatively benign conditions such as tinea capitis, acne, warts, and eczema. Studies have shown an increased risk of non-melanoma skin cancers in these patients in the years following their initial irradiation (3, 4, 6).
The association between IR and risk of subsequent BCC is consistent and strong for a variety of populations, with some evidence for a dose-response relationship (5, 12, 13). However, the relationship between IR and SCC risk is less established. Shore et al. retrospectively reviewed records of children treated with X-rays for tinea capitis for up to 50 years past the initial treatment and found no significant association between IR exposure and SCC risk (3). Karagas et al. reported similar results for patients treated with IR for both benign and malignant indications (4), and van Vloten et al. found that a much lower percentage of patients irradiated for a variety of non-cancerous conditions (e.g. hemangiomas, hyperthyroidosis) developed SCC compared to BCC after a latency period of 40 years (12). Despite differences in the mode of IR exposure compared to literature focusing on X-rays, studies examining the rates of NMSC in Nagasaki and Hiroshima residents of various ages and distances from the explosions after the atomic blasts in 1945 failed to find a significant increased risk of SCC in the years following the event (5).
However, there are reports of a higher SCC risk among early radiologists and technicians (14, 15). For X-ray technicians in the early 1900’s, IR exposure was often chronic and at a high dose, given the lack of regulation regarding excessive radiation (14, 15). Ron et al. concluded that BCCs may occur following low-moderate IR doses while SCCs have a greater chance of developing after high doses (5). The study hypothesized that this discrepancy could be due to a higher percentage of proliferating stem cells in the basal layer of the epidermis compared to the suprabasal layer (5). Other studies have reported additional factors that may impact the radiation exposure-SCC risk relationship, although the underlying mechanisms are not well understood. For example, several studies highlighted a relationship between SCC incidence and IR exposure especially in the context of certain risk factors for sun sensitivity (e.g. light eye color, fair skin complexion), but this relationship was less strong than that of between BCC and IR (6, 16, 17). The anatomical location and age of IR exposure may also play a role in the rates of NMSC incidence. While SCCs are more typically found on the extremities, such as the feet, BCCs are more common on the head and neck, making it difficult to determine the degree to which exposure solely contributes to NMSC incidence (18). For both types of NMSC, a younger age of IR exposure and a longer latency was associated with higher risk of skin cancer (6, 17).
Here we report an older female patient with a multiple-year history of SCC of the dorsal feet in the background of chronic radiation dermatitis and a distant history of frequent shoe-fitting fluoroscopy use. Given this unique exposure, the abrupt demarcation of these skin changes to the ankle and foot, and the concurrence of skin changes consistent with chronic radiation dermatitis, it is reasonable to conclude that shoe-fitting fluoroscope’s IR contributed to the etiology of these malignancies and pre-malignancies. Additional contributing factors include her sun-sensitive skin type, frequent doses of IR, young age of exposure, and long latency period (50+ years).
There are a variety of treatment modalities for NMSC, including surgical excision, Mohs micrographic surgery, electrodessication and curettage, radiation, and topical agents (e.g. 5-FU, imiquimod) (19). Treatments depend on location, cancer type and subtype, and patient preference. It is important to have a high index of suspicion for NMSC in irradiated skin. While ulceration can result from chronic radiation dermatitis, it is prudent to biopsy these ulcers to ensure that they do not represent a poorly differentiated malignancy. However, chronic radiation dermatitis can also result in profound atrophy and poor vascular supply to the involved skin, which may complicate the wound healing of biopsies and excisions. Treatments of chronic radiation dermatitis includes topical corticosteroids, surgical skin reconstruction, and wound dressings (20). Our patient’s SCCs were treated with excision or electrodessication and curettage, and her AKs were treated with cryotherapy given her intolerance to field therapy in the past. We managed her chronic radiation dermatitis with triamcinolone 0.1% ointment applied to the feet twice per day and wraps with liberal amounts of petroleum jelly to mitigate foot ulceration and pain. Future treatments may include referral to a wound or pain specialist to assist with skin healing.
Dermatologists should inquire whether a patient has received radiation treatment in the past whether regulated and therapeutic (e.g. radiation therapy for childhood cancer) or unregulated and accidental (e.g. repeated use of a shoe-fitting fluoroscope), as both can lead to increased skin cancer risk (6, 14). Patients should be educated on the long-term effects of radiation exposure and monitored for skin issues that can occur as a result.