1. Background
The nail is an opalescent window through to the vascular nail bed. It is held in place by the nail folds, origin at the matrix, and attachment to the nail bed (1). Nail disorders comprise approximately 10% of all dermatological conditions (2). Moreover, sometimes, nail changes can be presenting features before other signs of a systemic disease become clinically evident. Therefore, no dermatological evaluation is complete without a thorough nail examination. However, the nail remains an understudied, underutilized, yet quite accessible structure.
The nail as a unit is capable of projecting only a limited number of clinical manifestations. It is responsible for the more or less similar clinical presentation of numerous different nail disorders. Although various previous studies have focused on individual nail diseases, such as nail psoriasis, onychomycosis, and nail tumors, there are a limited number of published studies addressing nails as a whole system.
2. Objectives
Therefore, this study aimed to document various clinical patterns of nail changes, correlating them with different dermatological and systemic diseases. Additional objectives were to identify any predisposing or risk factors for nail disorders and analyze and correlate histopathology wherever required.
3. Methods
This cross-sectional observational study was conducted at a tertiary care hospital that included 200 patients (irrespective of age and gender) presenting with any kind of nail abnormality to a dermatology outpatient department (OPD). Mentally challenged individuals and those unwilling or unable to give informed consent were excluded. Institutional ethics committee permission was obtained before the commencement of the study. A case record form was designed to obtain basic information on demographics (i.e., age, gender, address, and occupation) and detailed history (i.e., Presenting complaints and other associated cutaneous/nail/hair/mucosal complaints related to toenails, and associated cutaneous/mucosal/hair). History was taken for any trauma, drug intake, and contact with chemicals. Clinical examination constituted a thorough cutaneous and orogenital examination. Nail examination was carried out in detail, including the number of nails involved and the type of abnormality (i.e., nail shape, attachment, surface, and color).
Routine investigations, such as a Haemogram test, biochemical evaluation, blood glucose, and human immunodeficiency virus (HIV) serostatus, were conducted in all patients. A skin biopsy was performed when it was required to confirm the clinical diagnosis. Special investigations, such as potassium hydroxide (KOH) (10%) mount and culture on Sabouraud’s dextrose agar media, dermatophyte test medium in suspected cases of onychomycosis, serum vitamin B12 level in all cases of melanonychia, and serum ferritin level in all cases of koilonychia and platynychia, were conducted. A nail unit biopsy (nail bed and matrix) was performed only on those cases presenting with isolated nail disease.
3.1. Statistical Analysis
The clinical and laboratory findings were recorded, and the data were analyzed using SPSS software (version 20.0). Qualitative data variables were expressed as frequency and percentage. The chi-square test/Fisher’s exact test was used to determine the association between the diagnoses with various qualitative data variables. A p-value of less than 0.05 was considered statistically significant.
4. Results
The mean age of the study population was 37.98 ± 16.79 years, and the majority (60%) of patients were within the age range of 21 - 50 years. The female to male ratio was 1:1.29. Although there were a higher number of females than males among onychomycosis cases, no significant association was observed between gender and disease. The most common occupation was housewife (n = 62; 31%) and manual laborers (n = 62; 31%). In addition, the occupation had a significant association with onychomycosis.
4.1. Chief Complaints
In this study, 45.5% of the patients had nail complaints as the presenting feature; however, in the remaining, nail changes were noted while evaluating for some dermatological or systemic disorders. The most common nail complaints were the physical or structural changes of nails in 49.5% of the patients, followed by pain and discoloration. Fingernails were more commonly affected (42%) than toenails (19.5%). All 20 nails were affected in 10.5% of the patients.
4.2. Etiology
Nail involvement secondary to dermatological disease was the most common overall cause of nail involvement (45%), followed by nail infections (36%); nevertheless, systemic-, traumatic-, genetic-, and drug-related causes contributed to the remaining 19% of nail diseases. Overall, onychomycosis (28.5%) was the most common cause, followed by nail psoriasis (19%) (Table 1).
| Nail Diseases | No. (%) |
|---|---|
| Onychomycosis | 57 (28.5) |
| Psoriasis | 38 (19.0) |
| Lichen planus | 15 (7.5) |
| Paronychia | 11 (5.5) |
| Vesiculobullous disease | 10 (5.0) |
| Connective tissue disorder | 8 (4.0) |
| Melanonychia (isolated) | 7 (3.5) |
| Eczema | 7 (3.5) |
| Leukonychia | 5 (2.5) |
| Epidermolysis bullosa | 4 (2.0) |
| Ichthyosis | 4 (2.0) |
| Ingrown nail | 4 (2.0) |
| Alopecia areata | 3 (1.5) |
| Habit tic deformity | 3 (1.5) |
| Koilonychia | 3 (1.5) |
| Subungual Wart | 3 (1.5) |
| Blue nail | 2 (1.0) |
| Darier’s disease | 2 (1.0) |
| Platynychia | 2 (1.0) |
| Pityriasis rubra pilaris | 2 (1.0) |
| Subungual hematoma | 2 (1.0) |
| Tuberous sclerosis | 2 (1.0) |
| Drug reaction | 1 (0.5) |
| Erythroderma | 1 (0.5) |
| Pyogenic granuloma | 1 (0.5) |
| Pincer nail | 1 (0.5) |
| Secondary syphilis | 1 (0.5) |
| Vitiligo | 1 (0.5) |
| Total | 200 (100.0) |
Observed Nail Diseases (n = 200)
4.3. Shape Abnormality
In this study, 26 patients showed nail shape abnormality comprising koilonychia in 8 (30.77%), anonychia (Figures 1A and B) in 7 (26.9%), platynychia in 5 (19.23%), clubbing in 3 (11.54%), racquet nails in 2 (7.69%), and pincer nails in 1 (3.85%) patient. Out of 7 cases with anonychia, 3 cases were secondary to epidermolysis bullosa, 2 cases due to pustular psoriasis, 1 case due to lichen planus, and 1 case due to paronychia. Two patients with racquet nails had collagen vascular disease (scleroderma). The cause could not be determined for pincer nails despite thorough history, examinations, and investigations.
4.4. Attachment Abnormality
Among attachment changes, the most common was onycholysis (n = 81; 40.5%) followed by subungual hyperkeratosis (n = 62; 31%), onychomadesis (n = 16; 8%; Figure 2), onychauxis (n = 15; 7.5%), and pterygium (n = 4; 2%). Onycholysis had a significant association with onychomycosis in comparison to other diseases.
4.5. Surface Abnormality
Observed nail surface changes were longitudinal ridging, Beau’s lines, pitting, trachyonychia, and onychoschizia. Out of the aforementioned changes, the most common were pitting and longitudinal ridging (n = 31; 15.5%), followed by Beau’s lines (n = 25; 12.5%) and trachyonychia (n = 24; 12%). Furthermore, pitting had a significant association with psoriasis (Table 2).
4.6. Discoloration
Nail discoloration was observed in 91 patients. The most common color change was yellow (n = 29; 31.87%) followed by black (n = 26; 28.57%), white (n = 23; 25.27%), green (n = 8; 8.79%), red (n = 3; 3.3%), and blue (n = 2; 2.20%). Nail discoloration was more common in onychomycosis as compared to all other causes of nail color changes (P = 0.03; Table 3)
| Onychomycosis | Psoriasis | Paronychia | LP (Lichen Planus) | Other | Total | Percentage (%) | |
|---|---|---|---|---|---|---|---|
| Yellow | 16 | 7 | 4 | 0 | 2 | 29 | 31.87 |
| White | 14 | 2 | 1 | 0 | 6 | 23 | 25.27 |
| Black | 6 | 2 | 0 | 3 | 15 | 26 | 28.57 |
| Green | 5 | 0 | 2 | 1 | 0 | 8 | 8.79 |
| Blue | 0 | 0 | 0 | 0 | 2 | 2 | 2.20 |
| Red | 0 | 0 | 0 | 0 | 21 | 3 | 3.30 |
| Total | 41 | 11 | 7 | 4 | 28 | 91 | 100.0 |
Correlation of Color Changes with Etiology of Nail Diseases (n = 91) a
4.7. Nail Psoriasis and Lichen Planus
In the analysis of individual diseases, the most common nail change in psoriasis was pitting (57.9%) followed by subungual hyperkeratosis (47.4%) and onycholysis (42.1%). The most common nail change in lichen planus was trachyonychia (46.7%) (Figure 3). Other less common findings were longitudinal ridging (36.8%), oil drop sign (21.1%), Beau’s lines (18.4%), onychauxis (18.4%), trachyonychia (15.8%), splinter hemorrhage (10.5%), fold changes (7.8%), and anonychia (5.3%). Anonychia was noted in two patients with pustular psoriasis.
4.8. Infections
Infections accounted for 72 (36%) cases constituting onychomycosis (n = 57; 79.16%), paronychia (n = 11; 15.2%), periungual and subungual wart (n = 3; 4.10%), and secondary syphilis (n = 1; 1.38%). Nail changes in secondary syphilis were longitudinal melanonychia, pitting, and subungual hyperkeratosis. The Most common nail changes among onychomycosis were discoloration (n = 41; 71.92%) and onycholysis (n = 37; 64.9%), followed by subungual hyperkeratosis (n = 29; 50.9%)". The associations between color changes and onychomycosis (Table 4) and HIV seropositive status and onychomycosis were significant.
In the onychomycosis group, the most common clinical pattern was distal lateral subungual onychomycosis (DSLO) observed in 61.4% (n = 35) of the patients, followed by total dystrophic onychomycosis (TDO) in 15.80% (n = 9) of the patients, white superficial onychomycosis in 14.04% (n = 8) of the patients, and proximal subungual onychomycosis in 5.26% (n = 3) of the patients; nonetheless, the least observed pattern was mixed onychomycosis noticed in 3.5% (n = 2) of the patients.
Direct microscopy by KOH and fungal culture were positive in 71.9% and 52.6% respectively out of 57 cases with clinically suspected onychomycosis. Both KOH and culture positivity were observed in 31.5% of the subjects. The most common causative agent was dermatophyte Trichophyton rubrum (58.26%; Figure 4).
Among chronic paronychia patients, 5 (45%) patients had diabetes mellitus. Out of 26 patients with black discoloration of the nail, 15 subjects showed longitudinal melanonychia. The most common cause was drug induction, among which the most frequent was the antiretroviral drug group. The most common genetic disorder associated with nail involvement was epidermolysis bullosa (50%), followed by Darier’s disease (25%) and tuberous sclerosis (25%).
4.9. Nail Biopsy
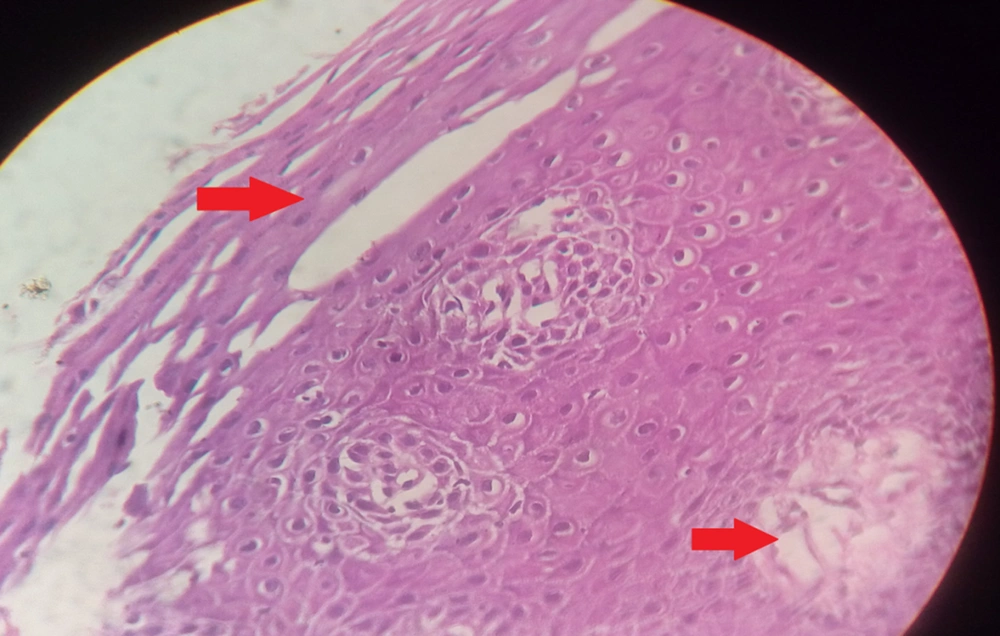
A nail matrix biopsy was performed on 15 patients presenting with isolated nail changes without any skin lesion. The results were conclusive in 12 (80%) patients, comprising psoriasis (n = 6), lichen planus (n = 3), and onychomycosis (n = 3). In three inconclusive cases, the diagnosis was made based on clinical features.
The histopathology of clinically suspected nail psoriasis (Figure 5) showed parakeratosis and hyperkeratosis in the nail plate as the most common feature (n = 6; 85.77%), followed by focal hypergranulosis (n = 4; 71.42%) and neutrophilic infiltrate in the nail bed (n = 2; 28.57%). The histopathology of lichen planus showed hypergranulosis (n = 3; 75%) as the most common feature (n = 6; 85.77%), followed by basal cell vacuolar degeneration (n = 2; 50%) and a band-like infiltrate (n = 2; 50%). A nail biopsy was diagnostic in three cases of suspected onychomycosis with fungal pseudohyphae detected in the nail plate and confirmed on Periodic acid-Schiff staining.
5. Discussion
The nail is an important part of various dermatological disorders. The clinical variants of nails are often observed in routine practice. In the era of the increasing trend of aesthetic consideration, even the slightest nail change might be a cause for concern. In the present study, the prevalence of nail diseases was noticed to be perceptibly higher in males than females. A German study (3) conducted in 2010 on 3531 patients with nail psoriasis showed that nail involvement was more prevalent in male individuals. The aforementioned results are consistent with the results of the present study. The high prevalence in males might be attributed to the greater degree of outdoor activity and the likelihood of reporting to the health care system, compared to that of females.
Additionally, the prevalence of most dermatologic and/or systemic diseases with nail involvement is probably higher in males. On the other hand, in this study, it was observed that females outnumbered males among the onychomycosis group. Similarly, the study of onychomycosis in 100 patients by Bokhari et al. (4) in 1999 reported a female predilection (female: 72% and male: 28%). This gender prejudice of onychomycosis might result from the greater participation of Indian females in household work and increased exposure to moisture, which might predispose them to fungal infections.
This study compared occupational risk among various nail diseases and showed a significant association between occupation and onychomycosis. The aforementioned results are in line with the results of a study conducted on 130 onychomycosis patients by Gupta et al. (5) in 2007 indicating a higher prevalence of nail diseases among farmers. The high prevalence among manual laborers and housewives observed by the present study could be explained by increased perspiration, a greater risk of occupation-related trauma, and exposure to soil saprophytes and water. Similar to the findings of the current study, another Indian study performed by Kaur et al. (6) reported that onychomycosis constituted 20 - 30% of all onychopathies.
Twenty nail dystrophy or trachyonychia is clinically characterized by thin, brittle, rough finger and toe nails with longitudinal ridging. 21 cases with trachyonychia were enrolled in the current study which constituted varied etiologies such as lichen planus (7, 33.33%), psoriasis (5, 23.80%), epidermolysis bullosa (3, 14.28%), icthyosis, erythroderma, eczema, PRP, pemphigus vulgaris, onychomycosis (1, 4.7% each). These causes are well-documented in the literature (7). The prevalence of nail psoriasis was lower in the present study (19%) in comparison to that reported by a German study (40.9%) (6). This is probably due to the overall lower prevalence of psoriasis in the Indian population, compared to that reported in Western literature.
After comparing the prevalence of nail pitting among various diseases, this study observed a significant association with psoriasis (coarse pits involving an average of four nails). A study on 1728 patients with nail psoriasis conducted by de Jong et al. (8) demonstrated pitting to be the most common nail manifestation; however, it was not possible to find any study reporting the proportion of nail pitting among individuals presenting with various nail changes.
Other disorders associated with nail pits in the present study were alopecia areata, lichen planus (superficial pits involving less than 3 three nails), secondary syphilis, contact dermatitis and pemphigus vulgaris. The secondary syphilis patient was also HIV seropositive and showed longitudinal melanonychia in addition to large deep pits (elkonyxis).
While comparing onycholysis among different disease groups, a significant association was observed with onychomycosis. Consequently, onycholysis can be considered a reliable marker of onychomycosis, particularly in the presence of yellowish (candidal), greenish, or blackish (dermatophytic/saprophytic) nail discoloration.
The current study analyzed color changes in onychopathies. Erythronychia was observed in 2 patients of Darier’s and 1 patient of Systemic lupus erythematosus (SLE). Out of 8 patients with greenish discoloration, Pseudomonas aeruginosa was cultured from 1 sample. The yellow color was secondary to onychomycosis in the majority of cases, followed by psoriasis.
The prevalence of nail psoriasis in the present study was 19%, which was slightly higher than a study by Samman PD. (12%) (9). Kaur et al. (10) in their study conducted on 167 psoriasis patients and Ghosal et al. (11) observed pitting to be the predominant nail change, followed by onycholysis and subungual hyperkeratosis. These observations were similar to those reported by the present study.
The study carried out by Tosti et al. (12) showed longitudinal ridging (10/15) as the most common nail finding, followed by trachyonychia (2/15) in lichen planus. Kanwar and De (13) observed longitudinal ridging as the most common finding in 17% of patients, followed by pitting in 15% and thinning of the nail plate in 9% of patients. The aforementioned findings are consistent with the findings of the current study.
The patients with paronychia in the present study belonged to the age group of 30-50 years. Additionally, 8 out of 11 patients were female, and the most frequently affected populations were housewives and manual laborers (probably due to recurrent and prolonged occupational exposure to moisture or harsh chemicals, such as solvents).
Guha and Panja (14), in a study performed on 100 chronic paronychia patients, showed that 76% of the patients were within the age range of 21- to 50 years with female preponderance. Please delete the sentence “The aforementioned study also echoed the female preponderance (90%) noted by Leon, on 201 paronychia patients. In the current study, 5 out of 11 (45.5%) patients had associated diabetes mellitus. According to Guha and Panja (14), 9.5% of diabetic female patients above the age of 20 years suffered from chronic paronychia, compared to 3.4% in the control group. Therefore, female gender, middle age, wet work, and diabetes are a few common risk factors mentioned in the literature, which were also observed to be associated with chronic paronychia in the present study.
In the current study, 5 out of 11 paronychia cases showed positive culture; Candida and Staphylococcus aureus species were isolated in 3 and 1 cases, respectively. One HIV seropositive patient with the greenish discoloration of the nail showed P. aeruginosa growth on culture. Guha and Panja (14) demonstrated that out of 25 paronychia investigated cases, 16 (64%) cases showed Candida albicans species on culture.
In the onychomycosis group, the most common clinical pattern was DSLO observed in more than half of the patients, followed by TDO in 15.80% of the patients. The results of the current study are consistent with the findings of Gupta et al. (5) in a study conducted on 130 patients with onychomycosis. Similarly, another Indian study (15) indicated that DLSO accounted for half of the onychomycosis cases. A significant association of nail discoloration was observed with onychomycosis. Therefore, it is recommended that all cases of nail dyschromia be screened for onychomycosis, particularly in tropical settings.
Weinberg et al (16) reported the sensitivity of KOH and culture as 80% and 59%, respectively; however, the specificity of KOH and culture were 72% and 82%, respectively. This finding justifies the low yield of culture positivity in the present study and emphasizes that although microbiological confirmation is desirable in all cases of onychomycosis, the diagnosis is most often clinical.
Dermatophytes (i.e., T. rubrum, tonsurans, and mentagrophytes) were observed to be the most commonly isolated causative organisms in onychomycosis, followed by yeasts (i.e., C. albicans and non-albicans Candida) and non-dermatophyte molds (e.g., Aspergillus). This result is consistent with the results of studies carried out on 90 cases of onychomycosis by Garg et al. (17) and Banerjee et al. (18), which also showed that dermatophytes were the most common isolates.
The nail has been deservedly termed as the mirror of internal diseases. Nail changes due to systemic involvement were observed in 25 patients constituting koilonychia in 8 (32%), platynychia in 5 (20%), leukonychia in 5 (20%), clubbing in 3 (12%), blue nail in 2 (8%), and melanonychia in 2 (8%) patients. Among leukonychia, two Terry nails secondary to hepatic cirrhosis and malnutrition and one-half and half nail secondary to chronic renal failure were encountered. The remaining 3 patients were diagnosed with idiopathic punctate leukonychia as the etiology could not be identified.
Koilonychia and platynychia were incidental findings in 8 patients who visited OPD for other dermatological complaints. On investigation, iron deficiency anemia was detected, which has been historically established as the most common cause of koilonychia.
Both patients with blue discoloration of the nail had concomitant peripheral vascular disease. Out of 3 patients with clubbing, 2 patients were attributed to lung involvement secondary to collagen vascular disease; nevertheless, 1 case with clubbing had congenital heart disease. A significant association of clubbing with chronic lung disease has been mentioned by Samman PD (9).
Out of 26 patients with the black discoloration of the nail, 15 patients showed longitudinal melanonychia. The most common cause was drug induction (46.68%), among which 4 cases were attributable to cyclophosphamide and 3 cases to zidovudine. Of the exhaustive list of drugs that can potentially cause melanonychia, cyclophosphamide is commonly prescribed in dermatologic practice; however, zidovudine is a part of the first-line highly active antiretroviral therapy regimens. Other observed causes were dermatological diseases (e.g., dermatitis, connective tissue disease, and lichen planus) and a single case of secondary syphilis. Further investigation in 2 patients with melanonychia led to the diagnosis of vitamin B12 deficiency. Consequently, the nail can be an early marker of undiagnosed systemic disease.
Nails are often subjected to trauma and exposure to environmental factors due to their anatomic location and protective function. In the present study, traumatic nail disorders constituted 5.5% of all nail diseases, of which 4 (36.4%) patients had onychocryptosis (i.e., ingrown toenails); nonetheless, the remaining constituted habit-tic deformity, subungual hematoma, pincer nail, and periungual pyogenic granuloma.
Khunger and Kandhari (19) elaborated upon some risk factors for ingrown toenails, namely ill-fitting shoes, improperly trimmed toenails, excessive sweating, nail infections, nail apparatus abnormalities, and diabetes. In the current study, all 4 patients with ingrown toenails wore occlusive footwear and were pre-obese (body mass index > 25); nevertheless, 3 patients had uncontrolled diabetes.
A nail unit biopsy (nail matrix, nail bed, and nail plate) was performed on 15 patients. Of 7 cases of clinically suspected psoriasis with isolated nail involvement (onychauxis in 1 and nail pitting in 6 patients), a nail matrix biopsy was diagnostic in 6 patients according to Hanno et al. criteria (20). The foremost histopathologic feature was parakeratosis followed by focal hypergranulosis and neutrophil infiltrate. Grover et al. (21) performed a nail biopsy on 22 psoriasis patients and observed hyperkeratosis with parakeratosis to be the most common (91%) and hypergranulosis as the least common (36%) histological findings.
5.1. Strengths and Limitations
Although there have been studies carried out on isolated nail diseases, the present study was a comprehensive compilation of all nail disorders encountered at a tertiary care center and attempted to augment the existing Indian data on this important but often neglected skin appendage. Multiple parameters were analyzed to determine predisposing factors; however, it was not possible to perform nail a unit biopsy for all the patients.
5.2. Conclusions
This study reiterates the importance of the nail as an integral component of the complete dermatological evaluation. A thorough history and meticulous examination of nails, supported by simple investigations, facilitate the early diagnosis of hitherto undetected cutaneous/systemic disease. The identification of risk factors for common disorders, such as onychomycosis and paronychia, can help holistic management strategies. Therefore, the nail unit deserves greater attention for better understanding and utilization as a diagnostic tool.