1. Introduction
Amputated stump is prone to various dermatoses and causes great morbidity. The dermatoses commonly found include stump edema, verrucous hyperplasia, allergic contact dermatitis, acroangiodermatitis, and even malignancies (1). Amputation greatly disturbs the normal pattern of blood and lymph flow, especially in the lower limb. This gets aggravated if the socket is improperly fitted, resulting in 'stump edema syndrome’ (2). During rehabilitation, it is mandatory to take care of the edema and manage the circulation of the stump. We describe a case of verrucous hyperplasia of the amputated lower limb, which got resolved with a change in prosthesis and pressure bandaging.
2. Case Presentation
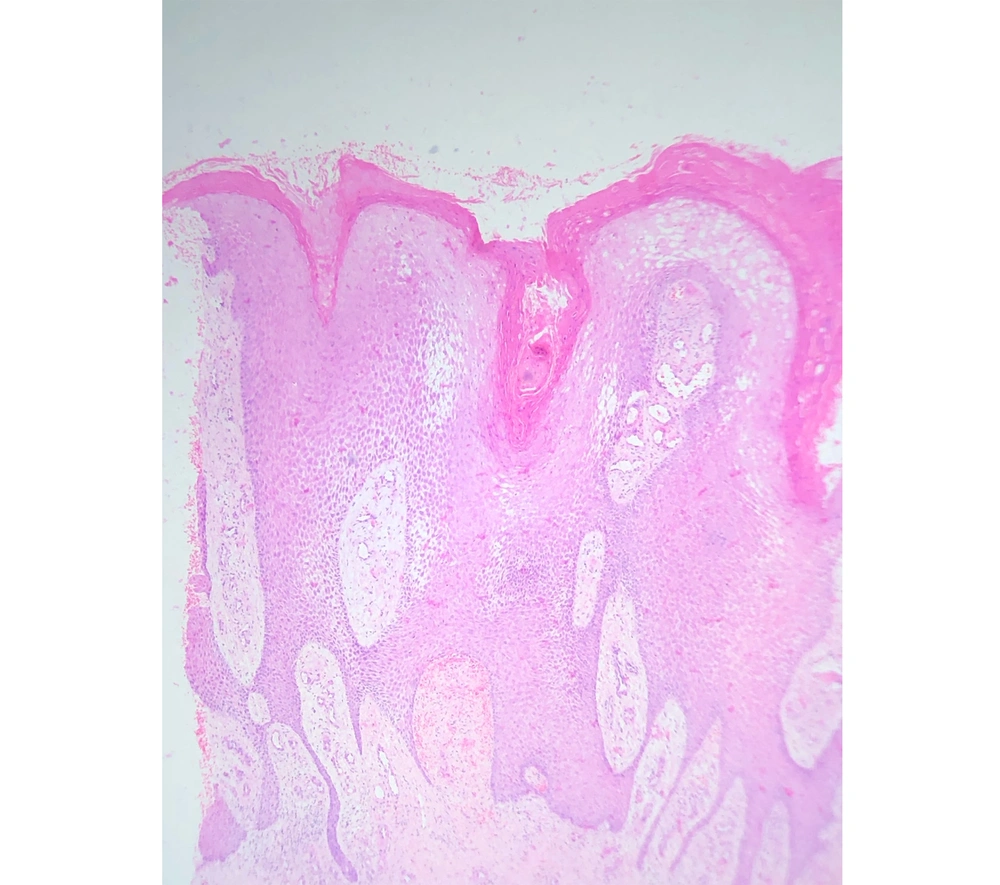
A 49-year-old male presented to us with a warty lesion on the amputated limb, which started as a small textural change at the tip of the amputated stump 12 years after his amputation. It was slowly growing, and he gave a history of repeated episodes of infection for which he had to take oral antibiotics. Clinical examination revealed a well-defined verrucous plaque at the tip of the amputated stump with surrounding erythema (Figure 1). His prosthesis was loose, and the amputated stump was loosely hanging inside the socket with no adequate padding. Histopathological examination showed hyperkeratosis, parakeratosis, and pseudoepitheliomatous hyperplasia with a mixed inflammatory infiltrate in the dermis. There were no koilocytes or malignant changes (Figure 2). A diagnosis of verrucous hyperplasia of the amputated stump was made. The patient was advised for a change of prosthesis and compression bandaging and the lesion resolved over three months.
3. Discussion
Verrucous hyperplasia is also known as papillomatosis cutis lymphostatica, lymphostatic congestion papillomatose (e.g., elephantiasis), or papillomatosis cutis verrucosa (e.g., mossy foot) (3). There have been various factors implicated in the pathogenesis of verrucous hyperplasia including poor-fitting prosthesis, suction socket prosthesis, venous stasis, and friction, and superimposed bacterial infections (4). These factors lead to impaired lymphatic outflow, which causes chronic lymphedema and subsequently, verrucous hyperplasia of the amputated stump. When the amputated stump lacks support distally, and when there is proximal compression, the limb edema gets aggravated. The limb swelling can be partially prevented by the gradual compression of the stump and the use of a properly fitted prosthesis. A correct socket of the prosthesis limb with distal padding helps in even the distribution of the pressure. This can be accompanied by compression using socks or bandaging. Early recognition and management of this condition can ameliorate much distress to the patient and improve their ability to effectively function within their community. It is also important to train the patient regarding the importance of prosthesis fit even if it is uncomfortable, edema management, and residual limb/socket hygiene.