1. Background
The vulvar non-neoplastic epithelial disorders (NNEDV) is also a hyperplastic lesion of the vulvar skin with leather-like skin thickening, wrinkles or scales, eczema-like changes, darker red or pink vulvar skin, but sometimes with clear white patches. NNEDV is an ‘intractable disease’ featuring a chronic course with severe itchy symptoms, treatment resistance, and high recurrence rates. In 1987 the International Society for the Study of vulvar disease (ISSVD) defined the disease into two main pathological types: squamous hyperplasia (SH) (Figure 1A) and lichen sclerosus (LS) (1). The latter often presents with whitening and thinning of the vulvar skin (Figure 2A). It also shows dryness and chapped of the surface, loss of tissue elasticity, atrophy of the clitoris, thinning and shrinking of the skin, associated with the disappearance of the labia minora and constriction of the vaginal opening. Lichen sclerosus affects the quality of life of the sufferers, causing distress and anxiety, which are easy to diagnose (2). These alterations can negatively affect the quality of life and sexual function, causing relational couple discomfort and impaired psychological well-being (3). Between 4 to 5% of women with LS develop vulvar squamous carcinoma (4). The therapeutic options for LS, namely ultrapotent topical corticosteroids, require long-term or life-long regimens and are not curative (5, 6).
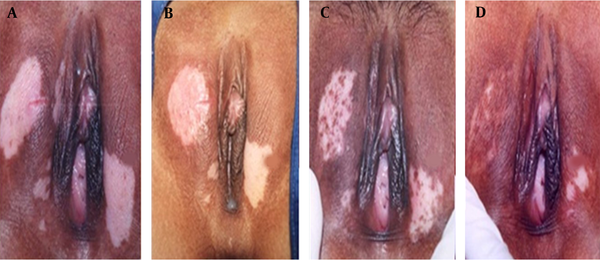
Vulvar NNED before and after focused ultrasound treatment. (A) before treatment, depigmentation on right labium majora and left labia minora and skin thickening. (B) At three months after treatment, the vulva is almost recovered. Vulvar lichen sclerosus (LS) before and after focused ultrasound treatment. (C) Clinical appearance before treatment. (D) The skin elasticity and pigmentation of the vulva were almost normal after 3 months of follow-up.
Vulvar leukoplakia before and after focused ultrasound treatment (A) Clinical appearance before focused ultrasound treatment. (B) Vulvar oedematous areas but with intact skin after focused ultrasound treatment. (C) Follow‐up at 1 month after focused ultrasound treatment showed an accumulation of skin pigments. (D) Two months after treatment, vulvar skin pigmentation returned to near normal.
Today FUS has been used to treat these irritating diseases noninvasively. Increasing studies in China revealed that FUS treatment for NNEDV is effective and safe. The current perspectives of advanced surgical treatment for lichen sclerosus involving high-intensity focused ultrasound surgery lead to improved patient outcomes (7). This paper describes the preoperative preparation, surgical technology, aftercare management, and results of focused ultrasound surgery to understand this non-invasive treatment.
2. Methods
2.1. Preparation of Focused Ultrasound Treatment for the Vulvar Non-neoplastic Epithelial Disorders
(1) A directed biopsy must be taken before the focused ultrasound treatment for suspicious lesions, and the histopathological diagnosis should be classified.
(2) The vulvar skin of the patient should be thoroughly evaluated, including tissue elasticity, skin thickness, and scars, etc., and the area for treatment estimated. For patients with a hard texture and marked thickening of the stratum corneum, 0.05% clobetasol ointment - a potent steroid ointment can be used 2 - 3 times per day for 3 - 4 weeks until the skin is soft before focused ultrasound treatment.
(3) The best treatment time is 3 to 7 days after menstruation. The timing of ultrasound therapy for pediatric or adolescent patients is after puberty.
(4) All pubic and vulvar hairs are shaved and removed to ensure good vulvar hygiene and condition.
2.2. Focused Ultrasound Treatment of Vulvar Non-neoplastic Epithelial Disease
Non-invasive focused ultrasound therapy was first applied to treat non-neoplastic epithelial diseases in 1999 when focused ultrasound energy beams are delivered to the deep-seated target tissue leading to coagulative necrosis of the subcutaneous tissue while the overlying skin and surrounding vulvar tissue are spared. The Model-CZF ultrasound therapeutic device we used for this treatment is a small machine manufactured from Chongqing Haifu Technology Co., Ltd., Chongqing, China (Figure 3). It comprises a power generator, a focused ultrasound transducer, a central console, and a circulating degassed water system. The 10‐mm diameter focused ultrasound transducer, operating at 8 - 12 MHz and pulses 100 - 3500 Hz, produces focused ultrasound energy with a focal length of 4 mm. The acoustic power was set at 3 - 5 Watt. A trained gynecologist can operate with the Model-CZF ultrasound therapeutic device without anesthesia and on an outpatient basis.
The FUS procedure involves a patient lying in a lithotomy position (the normal gynaecological examination position), with her vulva disinfected and completely exposed. Focused ultrasound treatment is performed under local anesthesia or general anesthesia. The Model-CZF system transforms the electrical power into an ultrasonic beam. A 12-mm diameter transducer probe is used for treatment with a frequency range from 8 to 12 MHz. The applicator is applied directly in contact with the vulvar lesions using water as the coupling medium. The operation is performed with a linear scanning mode at a speed of 3 - 5 mm/sec over the skin surface. Multiple linear scans move to cross the skin to cover the whole target lesion. The treatment area of each lesion included a margin of 5 mm of healthy skin. The treatment should last for about 15 to 30 minutes, depending on the lesion sizes.
2.3. The Postoperative Care and the Management of Adverse Events
After treatment, the lesion area should show a mild degree of congestion, swelling, and heat. The wrinkled skin becomes flat and smooth immediately after HIFU treatment. Ice compress is applied on the treated skin intermittently for 6 - 12 hours to reduce the skin and subcutaneous tissue temperature and decrease the release of inflammatory mediators and tissue edema; When applying ice pack compression, care is taken to avoid prolonged application to prevent skin frostbite. Vulvar skin colour should be carefully observed. If the skin is pale, the ice pack application should be stopped immediately. Moist burn ointment may be used locally for a week after focused ultrasound treatment. Other minor side effects may occur, and they are managed as follow:
(1) The vulvar pain: Some patients have pain in the treated area after focused ultrasound treatment, and the pain can be relieved by an ice compress and oral analgesia.
(2) Vulvar congestion and edema: Because of the thermal effects of the ultrasound treatment, all patients after focused ultrasound treatment will have vulvar congestion and edema. The coupling gel or cream should be applied strictly under instructions.
(3) Bruises of the vulva: Due to the destructive effect of ultrasound on the skin capillaries, bruises may occur locally after treatment. A 1:5000 potassium permanganate bath can be applied on the second day after focused ultrasound treatment, followed by 50% magnesium sulphate two times a day until the colour of the vulvar skin becomes normal. Local application and massage of Hirudoid cream in the affected area three times a day to speed up the disappearance of the bruises.
(4) Vulvar skin scald: Mild scalds can form blisters, usually appearing immediately or the second day after treatment. A sterile needle can be used to puncture the large blisters to remove the liquid inside.
(5) Delayed skin ulcers may occur 7 to 14 days after skin burn. They can present as local skin ulceration, necrotic tissue, and purulent secretions (with infection). Oral or intravenous infusion of antibiotics should be prescribed for one week. Some ulcers may need surgical debridement, followed by spraying of epidermal growth factor on the ulcers, and then scald cream used for external application. Most ulcers will heal in 2 to 3 weeks.
(6) Sensitisation or hyperesthesia may occur during the recovery process after ultrasound treatment, manifesting as pruritus vulva or pain. Local application of steroid or neurotrophic drugs can effectively relieve these reactions.
3. Discussion
Patients with vulvar non-neoplastic epithelial disorders (NNEDV) often present with white skin lesions of the vulva. They often complain of intense vulvar itchiness, pruritus, and skin depigmentation. Local applications of hormone and steroid medication are commonly used (8) but often ineffective. Laser and simple skinning vulvectomy are effective, but the recurrence rate is very high (9).
Vulvar non-neoplastic epithelial disorders (NNEDV) can be effectively treated with a satisfactory result, as shown in Figures 1 and 2.
Focused ultrasound therapy is effective in treating vulvar non-neoplastic epithelial disorders (NNEDV). Li et al. 2004 (10) first reported their early study of 76 patients with squamous hyperplasia (45 cases) and lichen sclerosus (31 cases). After focused ultrasound treatment, they showed a response rate of 94.74%, with the clinical symptoms dramatically improved. The treated skin areas returned to normal appearance in 3-6 months. In the 2-year follow-up, 64% (49/76) of patients were cured, 30% (23/76) improved, and only 5% (4/76) persisted. There were no major complications that occurred. Later, in another study, Sun et al. (11) demonstrated that focused ultrasound treatment of NNEDV is effective, safe with efficacy. Their results showed a 99.74% effective rate. A similar result was shown by Jia et al. that focused ultrasound can successfully treat vulvar intraepithelial lesion (VIN) lesion with the efficacy of 94% and minimal side effects (12).
However, in a larger study, Ye et al. (13) in 2015 presented their study of 950 patients with NNEDV treated with focused ultrasound therapy. They found that focused ultrasound therapy could effectively improve the signs and symptoms of the vulvar lesions, but with a lower cure rate of 42.2%, an effective rate of 56.1%, and a recurrence rate of 9.4%. There were no severe complications during or after the treatment. They also showed that statistically, focused ultrasound therapy was less effective in older patients with lichen sclerosus and larger lesions than in younger patients with squamous hyperplasia and smaller lesions (P < 0.05).
Wu et al. 2017 (14) investigated the efficacy of focused ultrasound treatment to NNEDV. From 2011 to 2016, they studied a total of 136 patients with NNEDV undergoing focused ultrasound treatment. They reported a response rate of 93.38% (127/136) with 50% complete remission (CR). Only 9/136 (6.62%) showed ineffective treatment. However, the cure rates of patients in the different age groups were significantly different. During their 5-years follow-up of 36 patients out of the 136 patients after treatment, 31 patients developed degeneration of vulvar skin and itch in the vulva, ie, a 22.79% (31/136) recurrence rate in five years. Today, many centres in China are using this technique for treating this condition (10-14).
Focused ultrasound treatment for NNEDV is a new treatment modality. It has gradually received clinical attention globally. It had a higher efficacy, less morbidity, and safety compared with conventional treatment methods. Focused ultrasound can treat NNEDV effectively with minimal complications at an outpatient procedure under local anaesthesia. From accumulating experience, the long-term remission of FUS is probably related to the inherent pathology of the vulvar diseases and the patients’ age, which may be predictive factors. Although the initial cure rate or symptoms relief is high, long-term remission has not been studied. Therefore, larger multicentre randomized studies with other therapies should be performed to establish the clinical safety and effectiveness of this novel and innovative treatment for vulvar non-neoplastic epithelial diseases.