1. Introduction
2. Case Presentation
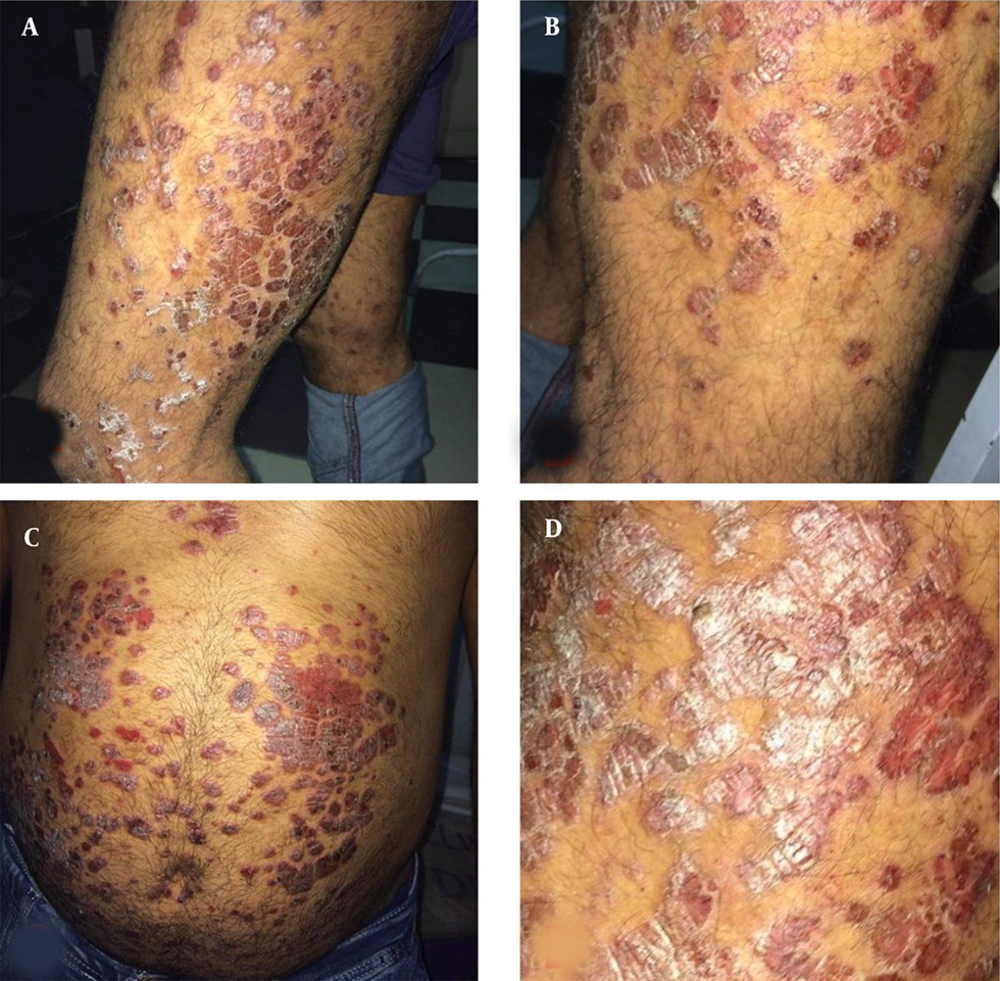
A 34-year-old male worker, a heavy cigarette smoker, was treated 10 years ago for mild controlled psoriasis vulgaris with topical medications (corticosteroids and emollients). He presented with severe itchy extensive psoriatic lesions involving most of his body in the past three months, not responding to previous lines of treatment and interfering with his daily activities. There was no family history of psoriasis and no history suggestive of systemic diseases. The patient used tramadol three months ago to treat premature ejaculation by self-description and gradually increased the dose to gain the maximum response. Since then, psoriasis became gradually extensive with marked itching and resistance to usual lines of treatment. Surprisingly, the withdrawal of tramadol improved itching and stopped the progress of psoriasis lesions. Diagnosis of psoriasis was confirmed clinically and dermoscopically. Clinical cutaneous examination revealed severe excoriated disseminated psoriasis plaques. General examinations of the patient were normal (Figure 1).
3. Discussion
The etiology of psoriasis is multifactorial. A complex interplay between genetic and environmental factors leads to the onset of psoriasis. In addition, several exacerbating factors could trigger psoriasis, such as infection, physical trauma, and emotional stress (3, 4).
There are numerous drugs eliciting psoriasis in several ways. First, the drug can aggravate the preexisting psoriatic skin lesions (drug-aggravated psoriasis). Second, the drug can initiate new psoriasis lesions in patients with a personal history of psoriasis. Third, the drug can provoke psoriasis de novo in patients without personal or family history of psoriasis. Several drugs have been linked strongly to psoriasis, such as beta-blockers, antimalarial drugs, lithium, imiquimod, interferons, and terbinafine (5). Rapid withdrawal of systemic corticosteroids or potent topical corticosteroids may cause a psoriasis flare (6).
Diagnosis of drug-related exacerbation and initiation of psoriasis can be difficult in daily clinical practice for several reasons. First, the association between drugs and psoriasis onset and/or exacerbation is usually not well-evaluated, resulting in a low level of evidence strength. Second, the lag time between the start of medication and psoriasis onset varies and can be pretty lengthy. Third, the psoriasis flare can persist in some patients, even after the implicated drug is withdrawn. Therefore, the clinical diagnosis of drug-related psoriasis may be challenging, and recognizing potential drugs involved in psoriasis is of clinical importance to allow optimal management (1).
To the best of our knowledge, we reported the first case of psoriasis vulgaris in which the lesions became extensive with marked itching and resistance to traditional lines of treatment after the use of tramadol. Thus, tramadol may be a new drug exacerbating psoriasis vulgaris that should be avoided. Tramadol increases the severity of psoriasis vulgaris and induces marked itching in this patient.