1. Introduction
Palmoplantar keratodermas (PPK) constitute a clinically and genetically complex group of cornification disorders characterized by defective epidermal differentiation leading to marked palmoplantar hyperkeratosis (1). Classically, keratodermas have been categorized as hereditary and acquired forms. Inherited forms are classified as syndromic or non–syndromic PPK (2). Clinically, PPK presents in diffuse, focal, or punctate forms (2). These diseases can be distinguished from each other based on the pattern of inheritance, morphology, severity, histopathological findings, systemic and syndromic associations.
In this study, we report a case of 12-year-old boy with palmoplantar keratoderma with contractures of fingers, which on further investigation, was diagnosed as pityriasis rubra pilaris (PRP), which is an extremely rare presentation.
2. Case Presentation
A 12-year-old male, son of a farmer, and the first child of a non-consanguineous marriage presented to our dermatology outpatient department in a tertiary care center with diffuse thickening and yellowish discoloration of skin of palms and soles since early childhood. He also developed contractures of the fingers of both hands. The thickening of skin and contractures were progressive. The patient complained of functional impairment due to contractures like buttoning and unbuttoning of shirt, lifting the spoon, and holding a pen. He denied presence of lesions elsewhere on the body, joint pain, or any constitutional or systemic symptoms. There were no complaints pertaining to visual or hearing loss. No such history could be elicited in the family members.
Dermatological examination showed bilaterally symmetrical thick hyperkeratotic fissured scaly plaques involving surface of entire palm with sharp demarcation at volar aspect of wrist. Similar plaques with yellowish hue were present over the soles with superficial fissures (Figure 1). The skin thickening was limited to palms and soles without impinging over the non-glabrous skin. The sensations were intact. Tight flexion contractures leading to mobile claw hand were present. Examination of the rest of the body revealed multiple barely perceptible grouped and discrete skin-colored follicular papules over the trunk (Figure 1). The detailed examinations of wrist, knee, elbow, and ankle joints were unremarkable.
Peripheral nerve examination did not reveal any thickening or tenderness. There were no other abnormalities of scalp, hair, mucosa or teeth. All ten toe nails were dystrophic, while finger nails had linear longitudinal dark bands. General and systemic examination was within normal limits. The differential diagnosis of palmoplantar keratoderma (hereditary) and follicular psoriasis with palmoplantar involvement were considered. His complete blood count, urine analysis and blood chemistry, lipid profile, and radiological examination of hand were unremarkable. HIV-ELISA and VDRL were negative. Thyroid function tests and electrocardiography were within normal limits.
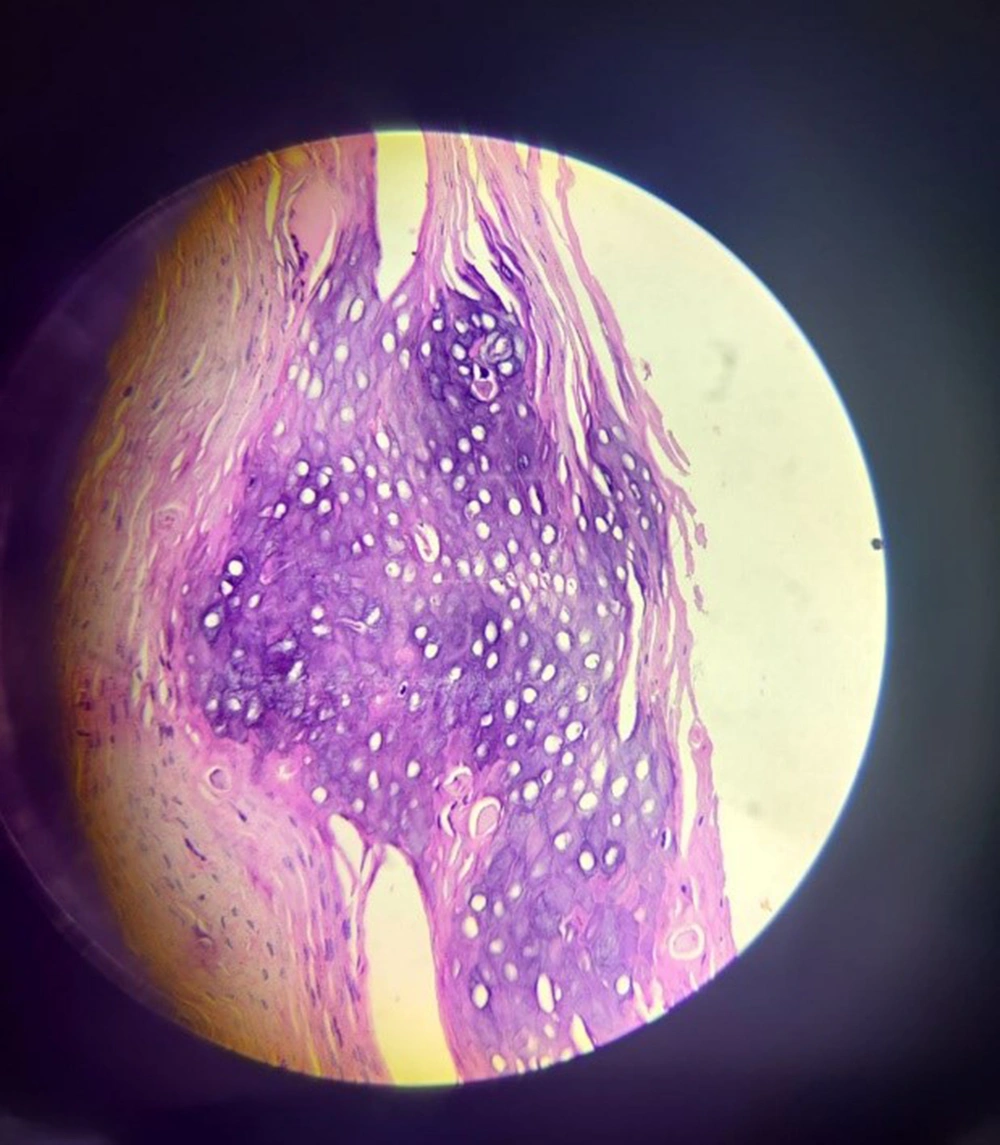
The histopathological examination of the skin biopsy specimen from the palm showed focal parakeratosis alternating with orthokeratosis in both horizontal and vertical directions (checkerboard pattern) with broadened rete ridges (Figure 2). The findings were consistent with PRP.
Treatment was started with systemic retinoids (Cap isotretinoin 10 mg at night), topical emollients (liquid paraffin after warm water soaks), and keratolytic agents (10% urea + 10% lactic acid combination in the morning and 20% urea application at night). After this treatment, the texture of the skin and mobility of fingers gradually improved. The patient was advised physiotherapy for further improvement of contractures and is currently under treatment with stringent periodic monitoring of lipid profile and liver function tests.
3. Discussion
PRP is an uncommon, inflammatory, and papulosquamous dermatoses of idiopathic origin. The disease usually begins as a pruritic generalised erythema with typical islands of sparing. The age distribution is bimodal, with onset commonly in the first and fifth decades (3).
Griffiths (4) proposed classifying PRP into five types considering age of onset, clinical presentation, and chronicity. A sixth category, which was associated with HIV (5), was added later.
Patients with Type 1 (classical adult onset) usually present with well-defined red scaly plaques, which may become widespread. Typically, intervening areas of normal skin are present, known as “islands of sparing” (6). The disease often starts over the scalp as a seborrhoeic dermatitis- like rash and spreads down the rest of the body; erythroderma frequently develops (7). There was no such history or clinical presentation in our patient.
Follicular hyperkeratosis may be present on elbows, wrists, and back of fingers. Palm and soles may become fissured and thickened. Nail changes can include distal yellow-brown discoloration and nail plate thickening. However, this type is self-resolving in an average of two to three years. Type 2 (atypical adult onset) is a chronic form, lasting longer than 10 years. Keratoderma and perifollicular papules do develop, but rapid spread with subsequent erythroderma develops rarely. Type 3 (classical juvenile onset) usually occurs between 5 and 10 years of age, considered to be the counterpart of type I PRP. This form usually undergoes spontaneous resolution within a year or two. Type 4 (circumscribed juvenile) usually occurs in children under 12 years of age. The commonest features are circumscribed plaques of erythema and follicular hyperkeratosis occurring on the elbows and knees. Scattered erythematous scaly macules may be present on the trunk and scalp along with Palmoplantar keratoderma. The prognosis of this type is uncertain. Type 5 (atypical juvenile) may be present at birth or start in early childhood with erythema and hyperkeratosis. Follicular hyperkeratosis is a prominent feature, and keratoderma is common. However, this type is commonly familial. Type 6 is encountered in HIV positive individuals (8). It is commonly resistant to retinoids and may respond to anti-retroviral treatment. Our case was HIV sero-negative. Type 3 PRP spontaneously resolves with one to two years, while our patient had progressive involvement. Types 4 and 5 have a chronic protracted course. Type 5 is commonly familial; however, our patient had no such family history. Type 4 presents with erythematous plaques and follicular hyperkeratosis of elbow and knees, not seen in our patient.
The description of clinical findings of our patient highlights a rare association of debilitating contractures with PRP. The classification of PRP by Griffith does not include any such entity. Despite a comprehensive literature search, we did not find any previously documented reports of non-paralytic claw hands due to PRP. Psoriasis shares many histologic features with PRP, but lesions of psoriasis have neutrophils in mounds of parakeratosis, thin and evenly elongated rete ridges, thinning of suprapapillary plates and broad dermal papillae, with mixed inflammatory cell infiltrates (9). The dilemma between follicular psoriasis and PRP was clinched by absence of Munro’s microabscesses in the histopathology. The classical pattern of alternating parakeratosis and hyperkeratosis found in our case has been characteristically described in PRP and is not seen in psoriasis or hereditary keratodermas. Another notable feature was the sparing of the joints.
Our patient was also thoroughly evaluated for the syndromic associations (10) related to palmoplantar keratoderma, while the histopathology results were awaited. Fortunately, no such association could be identified.
PRP is often recalcitrant and resistant to treatment. The most effective treatment, especially in children, is not yet standardized. Systemic retinoids are often considered the first choice of treatment for this hyperkeratotic entity, irrespective of age (11). There are some encouraging case reports of successful treatment with narrow-band ultraviolet B (NB-UVB) therapy, including the combination of acitretin and UVB light treatment (ReUVB) (12). Ustekinumab (13) may prove to be more effective than other agents when acitretin or methotrexate have failed or cannot be used (14). We prescribed isotretinoin (as the patient could not afford acitretin) along with adjuvant topical agents with slow but discernible functional improvement. Isotretinoin has been used previously with good response in a three-year-old male child with typical juvenile type of PRP (15). This is probably the first case report using isotretinoin in the management of juvenile PRP with debilitating flexion contractures of hands.
3.1. Conclusions
This report focusses on the recognition of unusual presentations of PRP and emphasises the importance of early diagnosis and timely treatment, which can avert the dreaded morbid and disabling complication of contractures. It also illustrates the promising utility of isotretinoin as a cost-effective alternative in resource-limited settings.