1. Introduction
Bullous pemphigoid (BP) is the most common among subepidermal autoimmune vesiculobullous disorders (1). It usually affects elderly individuals above 70 years, with slight female predominance. While no studies are available regarding the incidence of BP in different ethnicities, particularly in India, it is the most frequently reported immunobullous disorder in Western Europe, with an incidence of 7 to 43 per million population (2). Bullous pemphigoid (BP) rarely affects young people, with an incidence of less than 0.5 cases per million population below 50 years of age (3). A somewhat lower mean age of 64 years at disease onset was reported from China (4). It is an autoimmune vesiculobullous disorder that occurs due to antibodies against transmembrane protein BP 180 and hemidesmosomal protein BP 230, along with complement activation, mainly C3, and chemotaxis of neutrophils and eosinophils. There are very few case reports of BP in young people. Here, we report two cases of BP in young males.
2. Case Presentation
2.1. Case 1
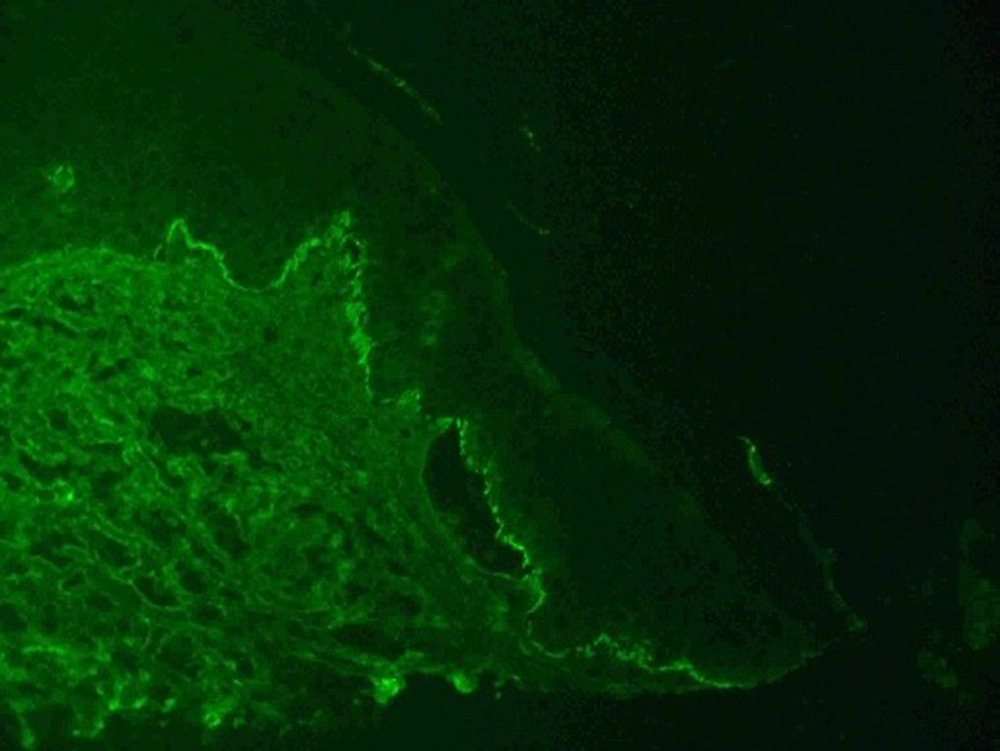
A 28-year-old male presented with painful fluid-filled lesions over his right forearm for three days. There was no involvement of the rest of the body or mucosa or history of other associated diseases. He gave a history of a single episode of similar lesions over the same site one year back, which resolved with some unknown topical treatment. There was no history of drug intake, radiation exposure, trauma, or any application of topical drugs prior to the onset of lesions. Dermatological examination showed multiple tense vesicles and bullae on the urticarial base with edema, tenderness, and local rise of temperature over the right forearm. Bulla spread sign was positive, while Nikolsky's sign was negative (Figure 1). The differentials considered were localized BP, cellulitis, linear IgA bullous dermatosis, irritant contact dermatitis, and fixed drug eruption. His blood (complete blood count, absolute eosinophilic count, liver function test, and kidney function test) investigations, including serum IgE level, were within the normal limit, and Arteriovenous Doppler of the left forearm was unremarkable. Blood and local pus culture did not grow any organisms. Histopathology from the lesion showed subepidermal clefts with eosinophilic and lymphocytic infiltrate. Direct immunofluorescence from perilesional skin showed linear IgG deposits at the dermo-epidermal junction in focal areas, with negative IgA, IgM, and C3, confirming the diagnosis of localized BP. The patient's treatment was started with prednisolone tablets 0.5 mg/kg in tapering doses, nicotinamide tablets 250 mg thrice daily, and doxycycline capsules 100 mg twice daily, along with other supportive treatment and local wound care. After two weeks of therapy, complete resolution was seen, and prednisolone was tapered off over the next month. Nicotinamide tablets 250 mg thrice daily and doxycycline capsules 100 mg twice daily were continued as maintenance therapy with no recurrence of lesions.
2.2. Case 2
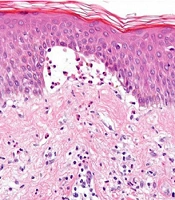
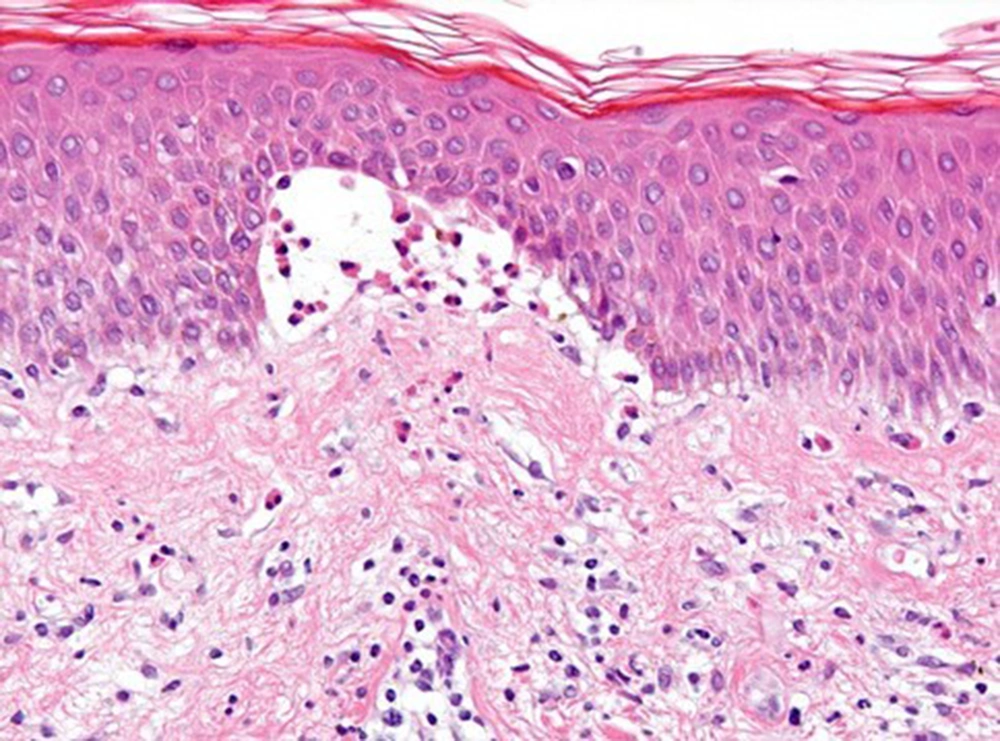
An 18-year-old male came with fluid-filled lesions over his face, hands, genitals, and feet for two months. He started developing tiny fluid-filled lesions over the scrotum, which gradually progressed to involve the face, palms, and feet. The lesions did not rupture spontaneously. There was a history of painful raw areas in the oral cavity with intolerance to spicy food. There was no history of similar illness in the patient or family members, itching or reddish lesions prior to the onset of lesions, systemic symptoms, or other associated diseases. He had been treated with varying doses of oral steroids and antiviral drugs from some private hospitals for the same, with slight improvement. On examination, multiple tense vesicles and bullae were present over the face, palms, inguinal folds, and legs, with positive bulla spread and negative Nikolsky's sign (Figure 2). Differentials kept were bullous pemphigoid, erythema multiforme, and pemphigus herpetiformis. His routine laboratory investigations were within normal limits. Histopathological examination showed a subepidermal blister with dense inflammatory infiltrates comprising neutrophils and eosinophils (Figure 3). Direct immunofluorescence revealed granular IgG along the epidermal basement membrane with negative IgM, IgA, and C3 (Figure 4). Thus, the final diagnosis of BP was made. The patient started prednisolone tablets 0.75 mg/kg in tapering doses, doxycycline 100 mg twice daily, nicotinamide 500 mg thrice daily, and supportive treatment. A complete resolution was seen after two weeks. Prednisolone was discontinued after two months. Currently, he is on regular follow-up with nicotinamide tablets 250 mg thrice daily and doxycycline capsules 100 mg twice daily as maintenance therapy without any recurrences.
3. Discussion
Bullous pemphigoid in young individuals is an infrequent entity with less than 0.5 per million population (3). Genetic and environmental factors can contribute to triggering bullous pemphigoid. This subepidermal blistering disorder can also be induced by certain drugs such as antihypertensives (captopril, enalapril, losartan, and beta blockers), furosemide, spironolactone, and antibiotics like ampicillin, cephalexin, and ciprofloxacin. Patients with drug-induced BP have a younger age of onset (5, 6), but both our cases denied a history of drug intake. The pathomechanism includes autoantibodies against BP180 and BP230 antigens, which are components of the dermo-epidermal junction (7). Anti-BP180 autoantibodies of various immunoglobulin isotypes and IgG subclasses are present in bullous pemphigoid sera, with IgG being predominant, followed by IgE. Serum levels of anti-BP180-NC16A IgG and IgE correlate well with disease activity in bullous pemphigoid (8, 9). However, due to unavailability, indirect immunofluorescence studies were not done in our cases.
BP lesions mostly present over flexors and abdomen as tense blisters on the urticarial base, with negative Nikolsky's sign. Most patients experience prodromal symptoms of pruritus and urticarial lesions weeks or months before the eruption of blisters (2); nevertheless, it was not present in our cases. Mucous membranes are rarely affected. However, there are certain clinical variants: Classic, localized, pemphigoid vegetans, dyshidrosiform, pigmented, nodular, papular, erythrodermic, toxic epidermal necrolysis-like, etc. (10). The classic form of BP is characterized by large, tense blisters on normal skin or on an erythematous base with lesions most commonly on flexural surfaces, the lower abdomen, and thighs, although they may occur anywhere, as in our patients. In the second patient, vesicles and bullae were predominantly present over the face and extremities. Localized BP is an unusual variant with less than 20 cases reported in young people so far (11), with the most common site being lower limbs or over surgical/burn/trauma scar, radiation therapy, and phototherapy site (12), but in our case, it developed de novo over the right forearm. The bullae are typically filled with serous fluid but may be hemorrhagic with a positive bulla spread sign and negative Nikolsky's sign. Epidermolysis bullosa acquisita (EBA) was ruled out because of the patient's age and lesion site. EBA is another subepidermal immunobullous disorder, which predominantly presents in elderly males as tense bullae over the sites of friction and trauma. The investigations confirming the diagnosis of BP in our patients included biopsy from intact blister for histopathological examination and perilesional biopsy for direct immunofluorescence studies.
Histopathology findings in BP are subepidermal blisters, and inflammatory infiltrates consisting of neutrophils, eosinophils, and lymphocytes/macrophages (13). Direct immunofluorescence shows linear IgG and C3 deposition in the basement membrane (14), often with elevated IgE and peripheral eosinophilia (15). However, serum IgE level was normal in both cases, and peripheral eosinophilia was not seen. The salt split technique also differentiates BP, epidermolysis bullosa acquisita, and bullous lupus erythematosus. It is performed by incubating punch biopsy specimens in 5 mL NaCl (1 mol/L) at 4°C for 24 hours, followed by separating the epidermis from the dermis using fine forceps (16). Bullous pemphigoid (BP) demonstrates roof pattern (autoantibody deposition on the epidermal side of the cleavage as major target antigens located in the upper portion of lamina lucida), while floor pattern is observed in epidermolysis bullosa acquisita. The primary treatment modalities are topical steroids for mild disease and oral steroids along with other anti-inflammatory drugs (doxycycline, dapsone, and nicotinamide) for moderate to severe disease, in addition to supportive treatment like antihistaminics and antibiotics. Immunosuppressants, like azathioprine, mycophenolate mofetil, and methotrexate, and biologics, like rituximab and omalizumab, are usually reserved for severe or recalcitrant disease. Both patients in this study responded satisfactorily to a combination of oral prednisolone, doxycycline, and nicotinamide, along with local care. Few cases of bullous pemphigoid in young individuals have been documented in the literature. In a case series of three patients, a 43-year-old woman presented with intense itching, followed by extensive urticarial plaques and papulonodular lesions after the ingestion of captopril, while another 49-year-old female developed nasal, oral, and genital mucosal erosions with widespread vesiculobullous eruptions following the intake of losartan. All three cases had elevated serum IgE with peripheral eosinophilia and were treated successfully with a combination of dapsone and systemic corticosteroids, along with discontinuation of the culprit drugs.
3.1. Conclusions
This case report emphasizes the importance of considering bullous pemphigoid as one of the differentials in young individuals presenting with vesiculobullous lesions. Histopathological examination and direct immunofluorescence are mandatory to confirm and differentiate bullous pemphigoid from other subepidermal blistering disorders.