1. Introduction
Berardinelli-Seip congenital lipodystrophy (BSCL) syndrome is a rare autosomal-recessive disease characterized by generalized lipoatrophy, acanthosis nigricans (AN), diabetes mellitus, muscular hypertrophy, hepatomegaly and hypertriglyceridemia (1).
Three major criteria or two major plus two or more minor criteria make a diagnosis of BSCL likely. Major criteria include lipoatrophy affecting the trunk, limbs, and face, acromegaloid features, hepatomegaly, elevated serum triglycerides, and insulin resistance. Minor criteria include hypertrophic cardiomyopathy, psychomotor retardation, hirsuitism, precocious puberty in females, bone cysts, and phlebomegaly (2).
2. Case Presentation
In June 2015, an 18 year-old-boy born of consanguineous parents, presented to the dermatology OPD in SBMP medical college, hospital and research center, Vijayapur with dark rugosity of skin since early childhood. He had voracious appetite, polyuria and nocturia. He was a normal full-term baby delivered by normal spontaneous vaginal way, with no prenatal, perinatal, or postnatal complications. The first two children of the parents expired in infancy. There was no other particular birth history of the two babies except low birth weight following the full-term normal delivery.
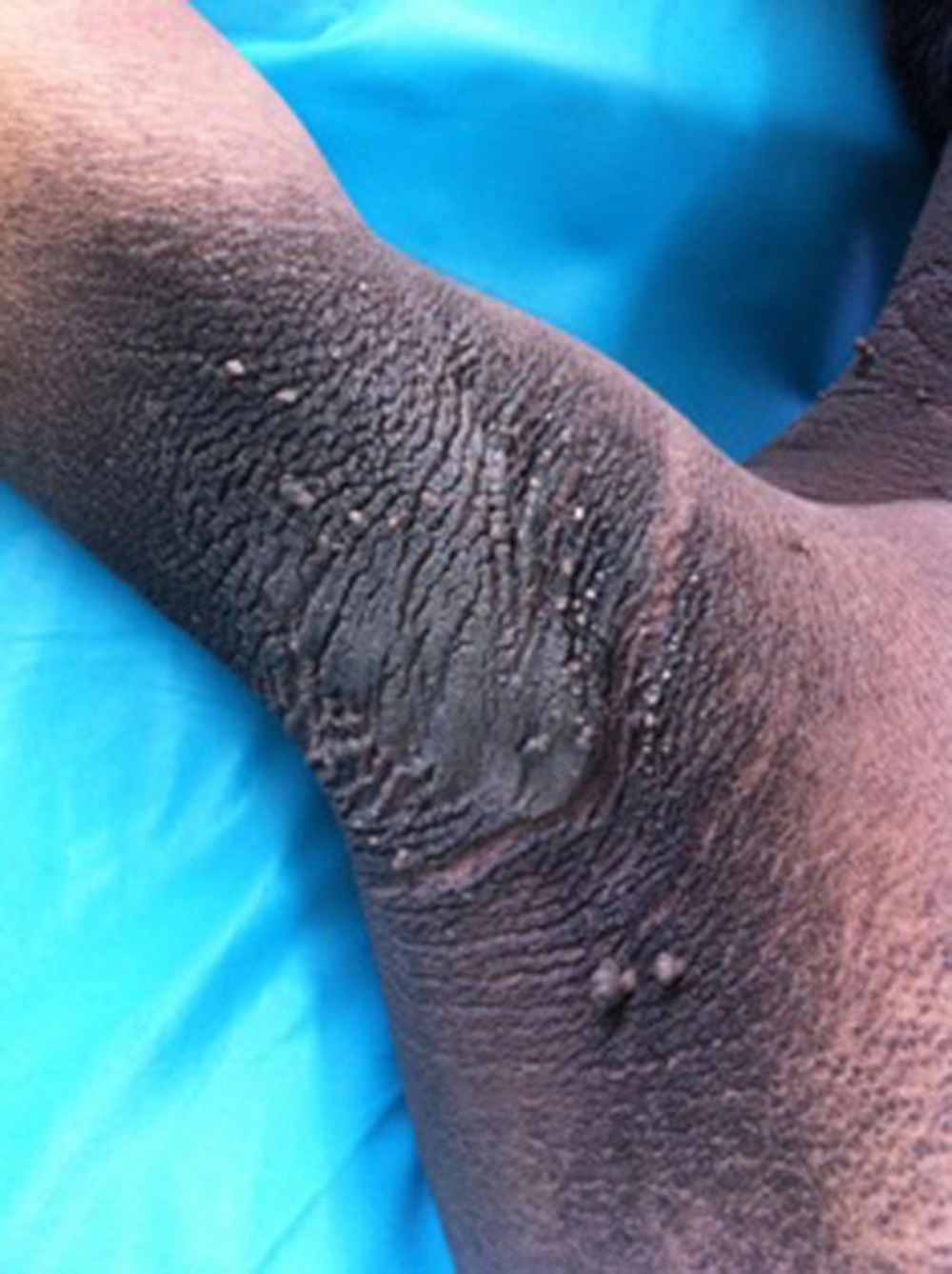
Physical examination revealed a height of 160 cm and weight of 45 kg. Clinical examination revealed acromegaloid facies (Figure 1) and generalized AN (velvety thickening and hyperpigmentation), which was more prominent around the neck and body folds including axillae (Figure 2), anticubital and popliteal fossae. He also had generalized loss of subcutaneous fat, hypertrophy of all limb muscles, prominent veins, enlarged hands and feet and multiple acrochordons around the neck and axillae (Figure 3). He had normal IQ. His vital signs and systemic examination were normal. Based on these clinical features, differential diagnosis of BSCL, leprechaunism and Rabson-Mendenhall syndromes (RMS) were considered.
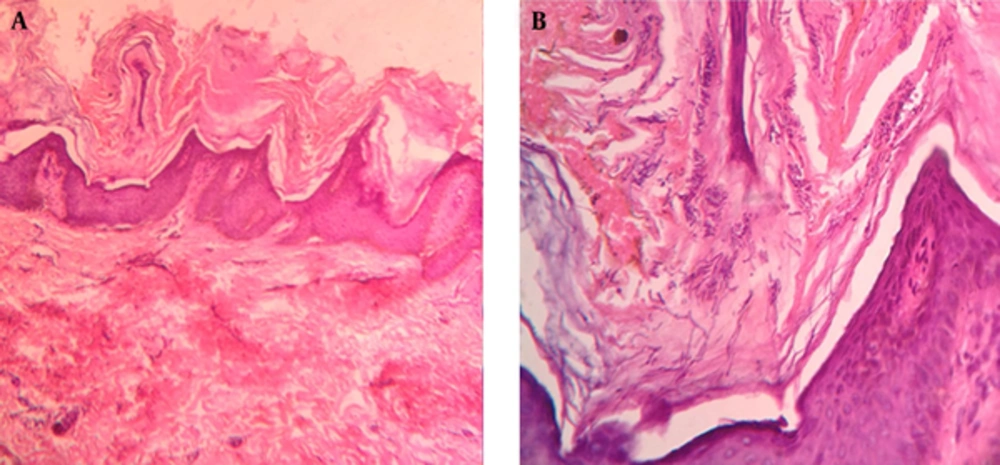
Laboratory investigation such as complete hemogram was within normal limits. Blood glucose study revealed hyperglycemia (RBS-321 mg/dL). The glycosylated hemoglobin (HbA1C) level of the affected individual was slightly higher than controlled diabetic range. Urinary ketone bodies were absent. Serum lipid profile showed hypertriglyceridemia (274 mg/dL) and low HDL-24 mg/dL. He had raised serum insulin levels-48.54 μIU/mL (N: 2.6 - 24.9 µU/mL). Histopathological examination of skin showed features of AN with fungal hyphae and spores suggestive of cutaneous candidiasis (Figure 4). Abdominal ultrasonography showed altered hepatic echogenicity, splenomegaly, and bilateral enlarged kidneys. Electrocardiogram and echocardiography were normal. Lack of resources prevented genetic analysis.
The Rabson-Mendenhall syndrome was ruled out by the presence of normal growth and absence of ketoacidosis and hypertriglyceridemia. Diagnosis of BSCL was made as our patient fulfilled four major criteria, lipoatrophy, acromegaloid features, hypertriglyceridemia and insulin resistance; although three major or two major plus two minor criteria would have been adequate. The patient was started on metformin 500 mg BD and given dietary advice, with significant improvement of AN and blood glucose level. He is currently under follow-up.
3. Discussion
Berardinelli-Seip congenital lipodystrophy is a very rare heterogenous disorder, first described by Berardinelli in 1954 and subsequently by Seip in 1959 (3). It has a prevalence of < 1 case per 10 million individuals and affects all ethnic groups (4).
Congenital generalized lipodsytrophy are caused by mutations in the AGPAT2, seipin (also known as BSCL2), LMNA, caveolin-1, and rarely the PTRF gene. At least three loci were identified. AGPAT2 has been mapped to chromosome 9q34 and encodes the enzyme responsible for the acylation of lysophosphatidic acid into phosphatidic acid, a key intermediate in the biosynthesis of triacylglyceride and glycerophospholipids (5). It causes BSC1; BSCL1 is less severe phenotype than BSCL2 (6). Individuals with type 2 BSCL seem to present more severe and premature symptoms than those who have mutations in type 1 with a higher incidence of intellectual deficiency in type 2 BSCL. This is because of the variability in expression of seipin in several tissues such as liver, skeletal muscle, kidney, pancreas, testicles and a high expression in the central nervous system and AGTPA2, tissue-restricted enzyme, occurring at high levels in adipose tissue, liver and cardiac tissue, but almost undetectable in the brain (7).
Berardinelli-Seip congenital lipodystrophy is characterized by the near complete absence of subcutaneous adipose tissue, severe diabetes mellitus, no ketosis/ketonuria and insulin resistance; the latter usually develops in the second decade of life (8). Acanthosis nigricans, a manifestation of insulin resistance starts in childhood, becoming more severe through adolescence. It is commonly seen in flexures, sides of the neck, back and the umbilicus as grey-brown or black pigmentation with thickened skin covered by small papillomatous elevations, giving it a velvety texture. All the above three feature are seen in our patient. Similar features have been described in many other reported cases (1, 5). Generalized lipoatrophy and insulin resistance are two of the major criteria for diagnosing BSCL (2).
Acromegaloid features including prognathism, salient orbital ridges, enlarged hands and feet, macrogenitosomia, gigantism, muscular hypertrophy and advanced bone age, hepatomegaly and elevated serum concentration of triglycerides form the other three major criteria for diagnosing BSCL (9). In all individuals with BSCL, the liver is affected, ranging from an abnormal liver functions to hepatic steatosis, hepatomegaly and cirrhosis. Minor criteria include hypertrophic cardiomyopathy, psychomotor retardation, hirsuitism, precocious puberty in females, bone cysts, and phlebomegaly (2).
Other features include curly and frizzy hair, hyperhidrosis, xanthomas, hypertrichosis and different forms of nephropathy. In BSCL, apart from liver, heart and muscle, excessive fat deposition in orbit, tongue, palms, soles, breast and vulva have been documented (10).
Cardiac abnormalities of the condition include hypertrophic cardiomyopathy, hypertension, cardiomegaly, congestive heart failure and ventricular dysfunction. Our patient showed no evidence of cardiac involvement.
Other features of this condition include empty cheeks, umbilical hernia, polycystic ovaries and pancreatic disease (loss of B cells or amyloidosis). Kher et al. has described the association of immunodeficiency in these patients (11).
Enlarged genitalia (hypertrophy of labia majora, clitoris), signs of virilisation, precocious puberty and polycystic ovary syndrome are common and secondary to hyperandrogenism related to insulin resistance (12).
Metabolic abnormalities in BSCL develop as the disease progress and may prove fatal necessitating optimal therapeutic and preventive measures. The prognosis of the disease is very poor, and patients often die in the third decade of life. There is no curative treatment and the current treatment options are based only on symptomatic control of the complications. Patients are advised low fat diet (< 15% of calories from fat) with enhanced physical activities. Other treatments include metformin, fibric acid derivatives, n-3 polyunsaturated fatty acids, and fish oil and leptin replacement for correction of metabolic complications (13). Recent studies have proposed replacement therapy with leptin, a protein produced by the adipose tissue that plays an important role in glycemic control and decreasing triglyceride levels thus yielding promising results in controlling lipid and carbohydrate metabolic disorders that are characteristics of this syndrome (14, 15). We report this case of BSCL in view of its rarity.