1. Background
Psoriasis is a common chronic, relapse-remitting, and inflammatory skin disease associated with severe psychosocial impact among patients (1). It is characterized by bilaterally symmetrical, well-defined, dry, erythematous, scaly papules and plaques (2). Dermoscopy is the latest non-invasive, portable, in-office method which enables the diagnosis of many dermatoses. Psoriatic lesions on dermoscopy reveal regular red dots on a pinkish background with scales. At higher magnification, glomerular, globular, and dilated convoluted vessels are noted with other features, such as hemorrhagic dots, micro-ulcerations, and white areas (3)
Methotrexate (MTX) is a well-known effective drug in the treatment of psoriasis (4). Biological drugs have currently revolutionized the treatment of psoriasis. Apremilast (APL) is an oral phosphodiesterase-4 enzyme inhibitor and was approved by the United States Food and Drug Administration in 2014 in the treatment of moderate to severe plaque psoriasis and active psoriatic arthritis (5). Worsening of psoriasis is observed in 10.7% of coronavirus disease 2019 (COVID-19)-infected individuals. Psoriatic patients who were on anti-tumor necrosis factor biologicals required more treatment switching when affected by COVID-19 (6). According to recent studies, risankizumab, a fully human immunoglobulin G monoclonal antibody against interleukin-23, was recently approved for moderate-to-severe psoriasis treatment that resulted in the improvement of alopecia universalis (7).
The comparative efficacy of MTX and APL in the treatment of psoriasis is well documented. The APL has a higher discontinuation rate than MTX in the first year of treatment (1, 8). Although MTX is considered the first line of treatment for psoriasis, there is a lack of evidence to prove its superiority over APL (9). Regrettably, the most established parameter to measure the severity and evaluate the effectiveness of treatments, the Psoriasis Area and Severity Index (PASI) is not standardized. As a result, there is a continuous search for objective measures to predict the response to treatment. Therefore, the dermoscopic prediction of treatment in psoriasis treated with biologicals, narrow-band ultraviolet B (NB-UVB), and MTX was attempted (10-12). However, the comparative analysis of dermoscopic assessment in psoriasis treated with MTX and APL is not reported in the literature.
2. Objectives
The primary objective of this study was to evaluate dermoscopic prediction in psoriatic lesions for the treatment with MTX and APL by comparing the PASI.
3. Methods
This randomized interventional comparative control study was conducted in a tertiary care hospital in southern India within January 2020 to June 2021. Institutional ethical clearance was obtained. Diagnosis-confirmed patients of psoriasis were enrolled in the study after obtaining informed consent. The inclusion criteria were patients over 18 years and cases of moderate to severe psoriasis. The exclusion criteria were patients with liver and renal impairment, pregnancy or breastfeeding history, immunosuppressive drug therapy, palmoplantar psoriasis, and exclusive involvement of the nail and scalp. A washout period of 1 month was considered for patients who were on treatment. Demographic data in terms of age, gender, and illness duration were recorded. Hepatic or renal functions were assessed in addition to routine hematological investigations.
The patients were randomly allocated into two groups, including group A, receiving oral MTX, and group B, receiving oral APL. The allocated medicine was given by the investigator. The patients were blinded to the drug they received. The MTX was administered in a dose of 7.5 mg/week for 3 months, and APL was administered in a dose of 10 mg/day for 10 days, followed by 20 mg/day for 10 days and then 30 mg twice daily for 3 months. The lesions on the upper limb, trunk, and legs were selected as “target” lesions. Clinical (taking serial photographs captured by the medicam 1000s) and dermoscopic (using FotoFinder videodermoscope with a magnification of 20×) assessments of target lesions were carried out at the baseline, 4th, 8th, and 12th weeks. The PASI score was calculated during each visit.
The data were evaluated in Microsoft Excel sheets and analyzed using SPSS software (version 19). Qualitative data, represented in percentage and proportion, were compared. Other appropriate statistical tests of significance, such as the chi-square test and student’s t-test, were applied. A P-value less than 0.05 was considered statistically significant.
4. Results
A total of 98 patients were recruited in the study and divided randomly into MTX (n = 50) and APL (n = 48) groups. However, five and three patients were withdrawn from group A and group B due to side effects, respectively. The patients’ age range was 18 - 65 years. The male-to-female ratio was 3:1. The disease duration ranged from 1 month to 10 years. The most common sites involved were the scalp, upper limb, trunk, and lower limb. Clinically, there was a reduction in the PASI in both groups during each visit. Nevertheless, the reduction in the PASI was significant in group A as compared to group B in the 8th and 12th weeks. Group A achieved a faster reduction in the PASI than group B. A statistically significant reduction in the PASI was obtained in group A (83%) and group B (65%) in the 12th week.
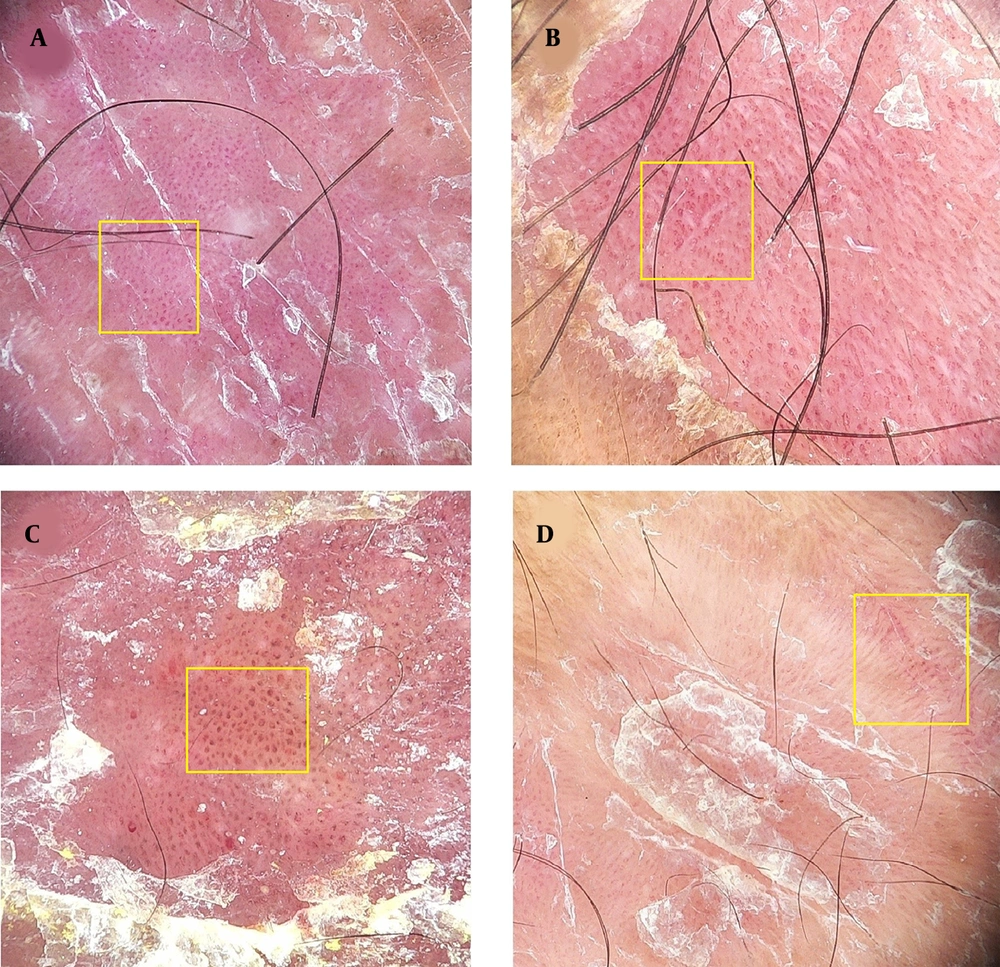
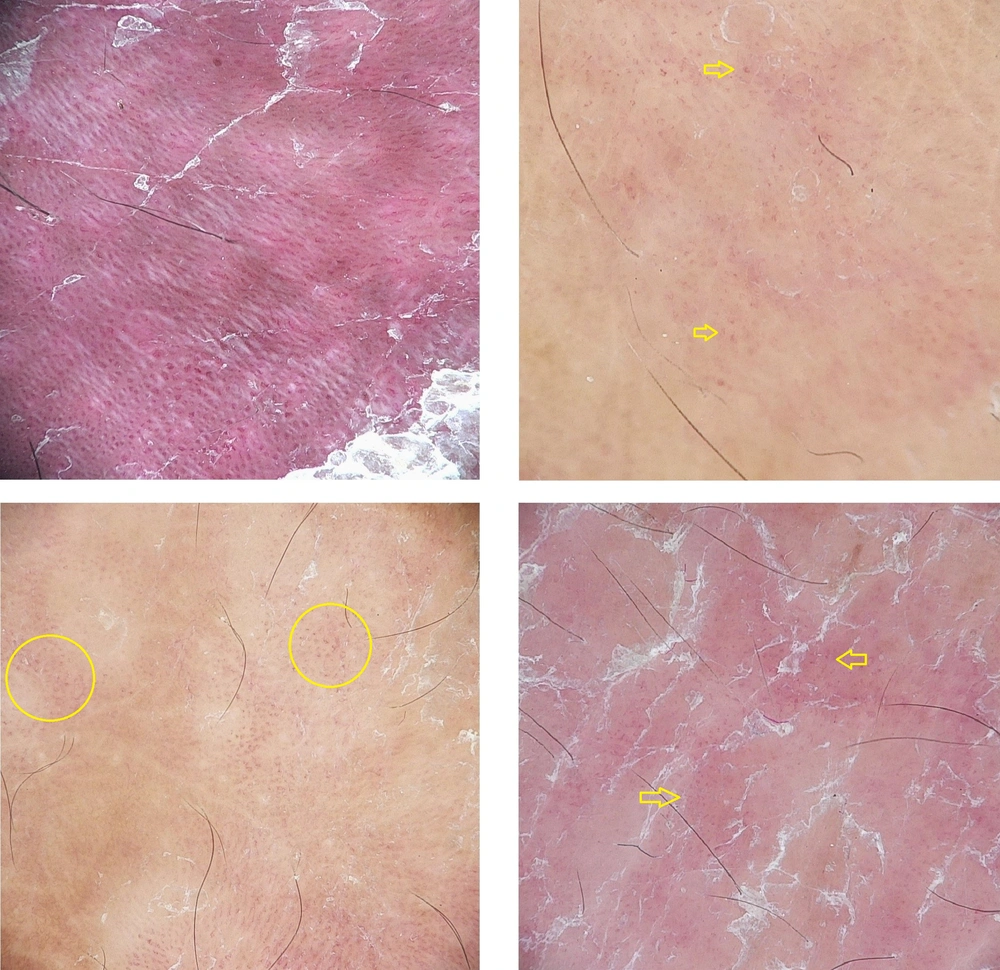
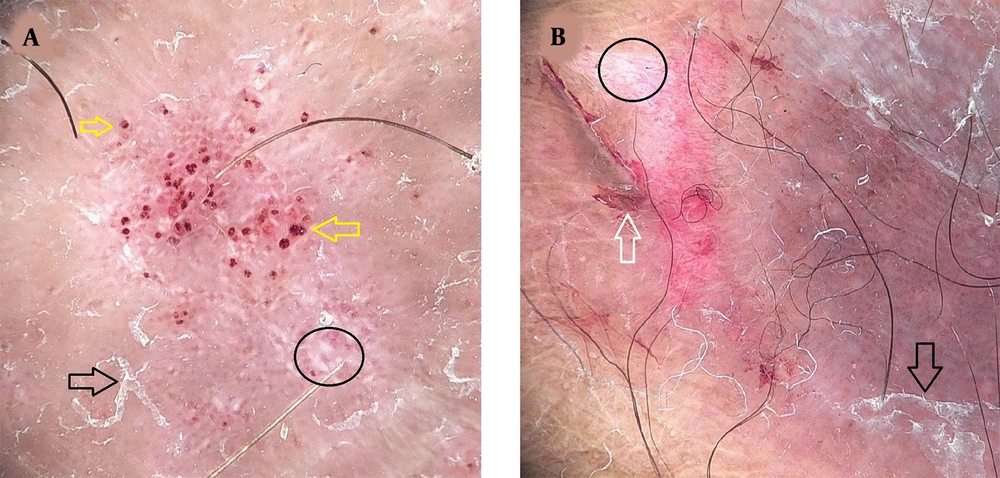
Dermoscopy showed regular red dots (Figure 1A), glomerular (Figure 1B), globular (Figure 1C), and linear convoluted (Figure 1D) vessels on a homogenous pinkish background. The arrangement of vessels was typified as regular (Figure 2A), scattered (Figure 2B), patchy (Figure 2C), and minimal (Figure 2D), in which uniform homogenous red dots, haphazard red dots, clusters of red dots, and homogenous but reduced red dots were observed, respectively (11, 13). Other vascular structures included hemorrhagic dots (Figure 3A) and micro-ulceration (Figure 3B). Apart from the vasculature, white areas, and bright white scales were also noted (Figure 3).
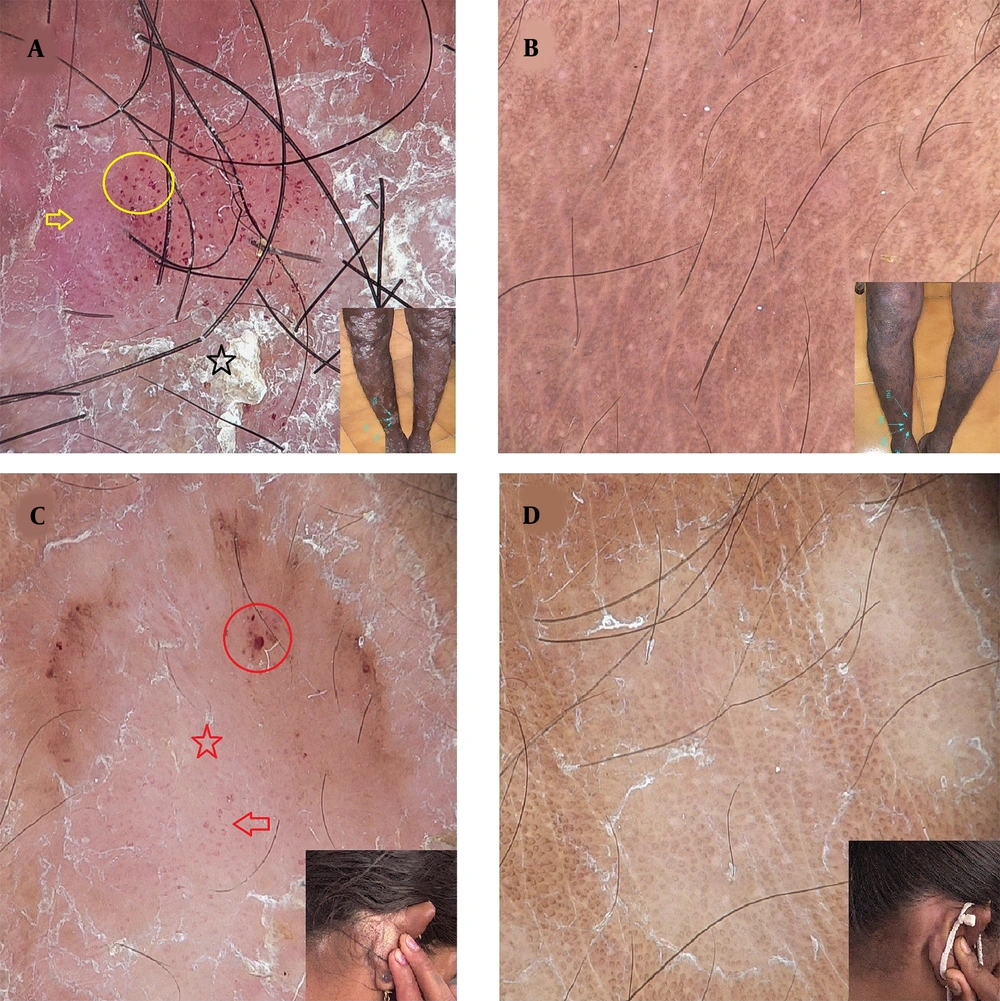
Before treatment, vascular structures and scales were well visualized in group A (Figure 4A and C) and group B (Figure 5A and C), which were reduced significantly in group A (Figure 4B and D) and group B (Figure 5B and D) in each visit during treatment.
Dermoscopy in methotrexate group: Hemorrhagic dots (yellow circle), red dots (yellow arrow), and white scales (black star) before treatment (A); disappearance of scales and vascular structures noted after treatment (B); white area (red star), hemorrhagic dots (red circle), and glomerular vessels (red arrow) observed before treatment (C); resolution of vascular structures and scales observed after treatment (D); inset: Clinical image
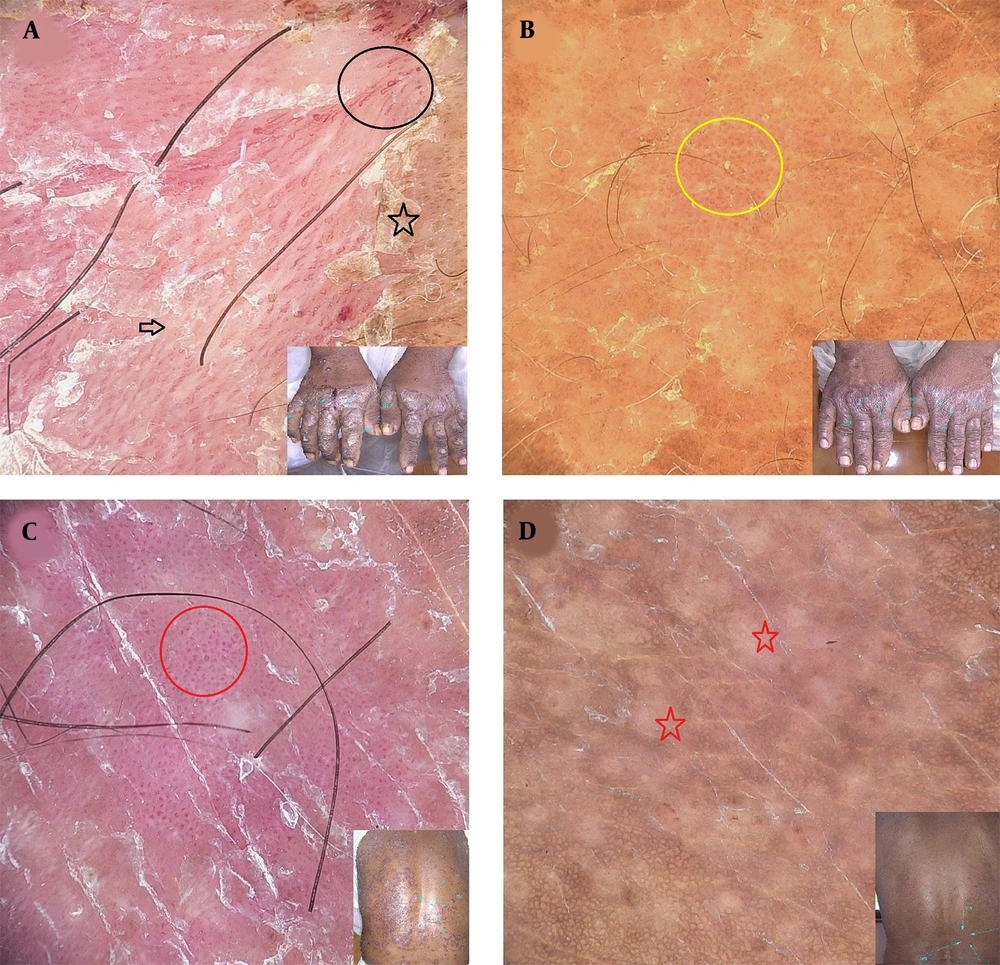
Dermoscopy in apremilast group: Linear convoluted vessels (black circle), white areas (black arrow), and white scales (black star) before treatment (A); disappearance of scales and vascular structures with few red dots (yellow circle) noted after treatment (B); glomerular vessels (red circle) observed before treatment (C); white areas (red stars) and resolution of vessels observed after treatment (D); inset: Clinical image
4.1. PASI According to Type of Vessels
The lesions with red dots showed PASI-100 (100% reduction in the PASI); however, in other types of vessels, the PASI reduction was average.
4.2. PASI According to Distribution of Vessels
The PASI-100 was obtained in patchy and minimal patterns. However, the regular pattern was resistant to therapy. Therefore, the PASI reduction was statistically significant (P < 0.001 by Pearson coefficient) based on the type and distribution of vessels.
Table 1 shows the frequency of dermoscopic patterns and the correlation of the PASI reduction regarding vessel morphology and distribution. Five patients from group A and three patients from group B were withdrawn from the study due to side effects, such as hepatotoxicity and intolerable diarrhea.
| Follow-ups | ||||||||
|---|---|---|---|---|---|---|---|---|
| Group A (n = 45) | Group B (n = 45) | |||||||
| Baseline | 1st Visit | 2nd Visit | 3rd Visit | Baseline | 1st Visit | 2nd Visit | 3rd Visit | |
| A) Dermoscopic features | ||||||||
| Regular | 19 | 15 | 12 | 13 | 15 | 10 | 10 | 12 |
| Scattered | 10 | 15 | 18 | 10 | 14 | 16 | 18 | 8 |
| Patchy | 12 | 12 | 14 | 17 | 13 | 15 | 16 | 20 |
| Minimal | 4 | 8 | 8 | 18 | 3 | 4 | 6 | 15 |
| Red dots | 20 | 10 | 7 | 1 | 11 | 8 | 5 | 3 |
| Glomerular/bushy vessels | 17 | 12 | 10 | 5 | 16 | 12 | 8 | 6 |
| Globular vessels | 15 | 8 | 4 | 2 | 10 | 12 | 5 | 3 |
| Radial vessels | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Micro-ulceration | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hemorrhagic dots | 18 | 13 | 5 | 0 | 14 | 10 | 8 | 6 |
| White areas | 16 | 9 | 4 | 4 | 12 | 10 | 7 | 3 |
| Red Dots, No. (%) | Glomerular, No. (%) | Globular, No. (%) | Radial, No. (%) | |||||
| B) PASI reduction | ||||||||
| PASI-50 | 0 (0) | 4 (30.7) | 8 (61.5) | 1 (7.7) | ||||
| PASI-75 | 0 (0) | 10 (37) | 17 (62.9) | 0 (0) | ||||
| PASI-90 | 19 (51.3) | 18 (48.6) | 0 (0) | 0 (0) | ||||
| PASI-100 | 12 (92.3) | 1 (7.7) | 0 (0) | 0 (0) | ||||
| Regular, No. (%) | Scattered, No. (%) | Patchy, No. (%) | Minimal, No. (%) | |||||
| C) PASI reduction | ||||||||
| PASI-50 | 10 (76.9) | 2 (15.6) | 1 (7.6) | 0 (0) | ||||
| PASI-75 | 19 (70.4) | 5 (18.5) | 2 (7.4) | 1 (3.7) | ||||
| PASI-90 | 5 (13.5) | 15 (40.5) | 14 (37.8) | 3 (8.1) | ||||
| PASI-100 | 0 (0) | 2 (15.4) | 8 (61.5) | 3 (23) | ||||
Abbreviation: PASI, psoriasis area and severity index.
5. Discussion
Dermoscopy, a non-invasive method, has gained popularity as an adjunctive in accurate diagnosis. Psoriasis specifically shows uniform and homogenous dotted vessels with bright white scales on a pinkish background (14). It should be noted that the term “red globules” is also used to describe red dots in the context of psoriasis, although their size has some differences (15). The other types of vascular structure are extremely rare in psoriasis. The arrangement of red globules in a circle or ring is also described in the literature (16). Under higher magnification, red dots appear dilated, convoluted, and elongated (17). In this study, the magnification of the dermoscope was 20×; therefore, glomerular and globular vessels were also noted. Linear convoluted vessels were noted in lesions with thick plaques. Hemorrhagic dots, which represent the extravasation of erythrocytes, are also described in psoriasis. They differ from red dots in being bright red in color due to the extravasation of erythrocytes (11).
Recently, dermoscopy has been utilized in the prediction of treatment outcomes in a given psoriatic lesion (11-13). Omar and Hassan studied the therapeutic response in psoriasis lesions treated by MTX and NB-UVB and observed a significant decrease in the hemorrhagic dots at the end of 4th month. Furthermore, the regular distribution of red dots was negatively correlated with disease response (13). In a report by Errichetti et al., the prediction of treatment outcome was assessed in psoriatic lesions treated by NB-UVB. Moreover, they showed that globular and dotted vessels were associated with poor/no response and good response, respectively. It is proposed that psoriatic plaques localized to legs and the lesions showing globular vessels predict poor response by NB-UVB (11).
In this study, treatment response varied depending on the type and distribution of vessels. Red dots at the baseline showed better response with PASI-100 at the end of 12th weeks in the majority. Inversely, globular and glomerular vessels demonstrated a poor response to treatment, and PASI-100 was observed in a very small number. This is probably due to variations in the degree of tortuosity and dilatation of capillaries in the dermis. A more pronounced inflammatory process produces globular and glomerular vessels; nevertheless, red dots are due to mild inflammation. In terms of the distribution of vessels, PASI-100 was noted in patchy distribution at the end of the 12th week. Conversely, none of the lesions with regular distribution achieved PASI-100. The patchy and regular distributions suggested the presence of minimal and profound capillary dilatation, respectively, thereby demonstrating a good response in the former and a poor response in the latter. Similar findings were observed in both groups. Therefore, MTX and APL had similar therapeutic efficacy when compared dermoscopically. However, PASI-100 was obtained faster in group A than in group B. It is proposed that the presence of red dots and patchy distribution would predict a better response to both MTX and APL. Although glomerular, globular vessels and regular pattern would show a poor therapeutic response to both MTX and APL. Nevertheless, the therapeutic response was not analyzed based on the location of lesions.
In another study on therapeutic response to biologicals in psoriasis, Lallas et al. showed that regular and patchy distribution had no and good responses to treatment, respectively. The absence of vessels at baseline demonstrated a complete response. Lallas et al. also noted that the persistence or reappearance of red dots during treatment had a high recurrence rate; nevertheless, hemorrhagic dots demonstrated a favorable response to biologicals (10). The observations of the present study are in line with the aforementioned findings. The lesions with scattered and minimal distribution showed a good response (PASI-100 in 61.5% and 23%, respectively); however, the regular pattern showed the least improvement (PASI-50 in 76.9%). This disparity could be based on inflammation and, in turn, on the amount of vasodilatation. Hemorrhagic dots showed a good response. This could be due to minimal vasodilatation with the extravasation of erythrocytes. Therefore, the lesions with scattered and minimal distribution and hemorrhagic dots would predict a good response to both MTX and APL. However, in this study, it was not possible to follow up on the lesions after 12 weeks for the recurrence of the lesion. Micro-ulceration (due to excoriations) and white areas (representative of psoriasiform hyperplasia due to the chronicity of the lesion) were reduced significantly (P < 0.05) in both groups after the treatment. The faster achievement of PASI-100 in patients on MTX is based on the potent antiangiogenic in comparison to APL. Therefore, vascular structures in psoriatic lesions responded well to MTX, compared to APL (18).
To summarize, the current study’s results suggest that dermoscopy is a useful diagnostic tool in evaluating the response in psoriatic lesions treated with MTX and APL. Vascular structures were the predominant feature in providing the early indication of treatment response in psoriasis. Therefore, vascular structures not only play a significant role in the dermoscopic diagnosis of psoriasis but also predict treatment outcomes in the lesions treated with MTX and APL. The dermoscopic assessment of psoriatic lesions in successive follow-up visits would bring benefit in predicting the therapeutic outcomes of MTX and APL. Concerning cost and dosage, MTX is economical and has better compliance than APL. The MTX has a faster PASI reduction than APL.
The limitations of the present study include the small sample size and a lack of follow-up analysis after 12 weeks. Variations in dermoscopic features based on the location and duration of lesions were not also assessed.
5.1. Conclusions
Dermoscopy, as a rapid assessment tool in clinical practice, is proven helpful in the prediction of the treatment response in psoriasis by demonstrating definitive vascular patterns which could be used for choosing a better treatment modality. It is repeatable each time with a great authentication of evidence-based documentation. The presence of red dots with patchy distribution and hemorrhagic dots would predict a good therapeutic response to both MTX and APL. Patients would be convinced about the prognosis of their psoriatic lesions, and treating physicians would benefit from the identification of which drug is good for a particular vascular pattern.