1. Introduction
Pediculosis capitis and tinea capitis primarily affect school-aged children. The causative dermatophyte species of tinea capitis varies across geographical regions (1). In contrast, Pediculus humanus capitis is responsible for pediculosis capitis worldwide. The coexistence of both infections in the same patient is rare (2).
The overall pediculosis capitis infestation rate amongst school-age children may reach more than 25% in some studies (3). Children with lice infestations may be completely asymptomatic; however, there is usually some pruritus. The itching can be severe, leading to excoriations, secondary impetiginization, and cervical lymphadenopathy. Identification of crawling adult lice and/or the nits, mainly in the occipital and retroauricular scalp, confirms the diagnosis (4).
Tinea capitis also mainly affects children worldwide, with a higher frequency in tropical and subtropical regions and an estimated occurrence rate of up to 45% in some studies (5). Tinea capitis can present with a multitude of clinical manifestations, including alopecic patches, scaly scalp that may be confused with nits, inflammatory changes in kerion with purulent discharge, and the possibility of cicatricial changes.
2. Case Presentation
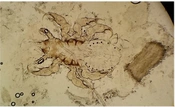
Herein, we present a 9-year-old girl presenting to our Mycology Clinic for an extensively scaly scalp with multiple focal areas of alopecia. The alopecic patches showed broken hairs, consistent with the clinical diagnosis of black dot tinea capitis. Hence, to confirm the diagnosis of tinea capitis, scrapings from the hair stumps were collected for potassium hydroxide (KOH) smears and fungal culture. Scrapings of hair stumps from the alopecic patches were examined with 10% KOH under light microscopy. At 200X magnification, to our surprise, a nymph of P. humanus capitis was seen attached by its claws to a healthy hair, with dystrophic hairs seen in the background (Figure 1). Clinically, pediculosis might have been obscured by the heavy scalp scaling. The dystrophic hairs on higher (400X) magnification showed endothrix fungal spores. The culture of the scrapings on Sabouraud dextrose agar (SDA) revealed, after 2 weeks, the growth of Trichophyton violaceum, which is endemic to our geographical region (1). The child was prescribed both systemic griseofulvin at a dose of 10 mg/kg for tinea capitis and topical 5% permethrin lotion for pediculosis.
Six-legged nymph (according to appearance, the third nymph) of Pediculus humanus capitis attached by its claws to a hair. Next to the nymph, there is a dystrophic hair parasitized by fungal spores (endothrix). The sections are visualized using 10% potassium hydroxide under light microscopy at 200X magnification
3. Discussion
The simultaneous acquisition of pediculosis capitis and tinea capitis is rarely reported. Also, the visualization of pediculi in scrapings is unusual and, hence, rather an interesting site.
The definitive diagnosis of pediculosis capitis can be made upon identifying crawling lice on the scalp hair. Nits alone are not diagnostic of active infestation unless they are very close to the scalp, are dark-colored, and contain larvae (6). In our case, the nymph was clearly demonstrated on a wet mount of scraped hairs.
Clinical diagnosis of tinea capitis is usually confirmed by KOH-prepared wet mount of plucked hairs or hair stumps collected by scraping or brushing. The location of the fungal spores in relation to the hair shaft (endothrix or ectothrix) can give a clue about the causative dermatophyte species, which should be confirmed by fungal cultures as SDA. Sabouraud dextrose agar contains dextrose, peptone, agar, and chloramphenicol to inhibit bacterial growth. Fungal growth is expected within 2 to 4 weeks. The gross appearance of the culture and stained culture mounts can accurately specify the causative dermatophyte subtype (7). The presence of endothrix suggests that the etiological agent belongs to the Trichophyton fungal genus. Waxy, glabrous, wrinkled, deep purple colonies (like the ones that were isolated from our case) are characteristic of T. violaceum (8).
Permethrin, a synthetic pyrethroid, interferes with sodium transport in the parasite, subsequently causing neural depolarization and, hence, respiratory paralysis. Permethrins are considered safe with low toxicity, and retreatment in 7 to 10 days is advised for the recently hatched nymphs (9). Although the 5% concentration is mainly used for scabies, it is currently used for pediculosis to overcome the resistance to the 1% preparations. Other lines of treatment for pediculosis include mechanical lice/nit removal using wet combing or other chemical preparations, such as lindane 1% and malathion 0.5% (6). Griseofulvin is FDA (Food and Drug Administration)-approved for treating tinea capitis. It is considered the drug of choice, especially in children, with high cost-effectiveness, cure rate, and easy accessibility. Griseofulvin is a microtubule assembly inhibitor that interferes with the formation of the mitotic spindle; hence, it inhibits mitosis in dermatophytes (10).
Body louse is a known vector for Bartonella organisms (B. quintana, B. recurrentis) (11), as well as for louse-borne relapsing fever, trench fever, and epidemic typhus, by transmitting different Rickettsia species (R. prowazekii, R. rickettsii) (12). However, whether head lice also serve as a vector is still inconclusive (13).
Studies found that head lice can pass infective Rickettsiae in their feces (14). Other studies showed that head lice could harbor a number of bacterial pathogens, such as the DNA of B. quintana (15), Coxiella burnetii (16), Borrelia recurrentis (17), and even Acinetobacter (16). However, the mere presence of a bacterial organism in an arthropod does not necessitate the ability to transmit it to humans and cause a disease in the infested individual (13).
The question remains whether the coexistence of tinea and pediculosis capitis is mainly attributable to overcrowding, poverty, and poor hygiene or whether the head lice might have a role in harboring and transmitting dermatophytes (2).