1. Background
2. Objectives
This study determined the epidemiological and clinical characteristics of eyelid tumors seen in an Iranian population.
3. Methods
A retrospective chart review was conducted on patients who had undergone the excision of eyelid lesions from April 2022 to April 2023 in the Skin Clinic of Razi and Farabi university hospitals (Tehran, Iran). All the tumors were first fixed in formaldehyde and then embedded in paraffin. They were classified according to histopathology using hematoxylin and eosin (H&E) staining according to the classification criteria of the World Health Organization (WHO). The 5th edition of the classification of tumors of the eye and orbit by the WHO covers common malignant and benign eyelid tumors based on their site-specific characteristics. This chapter also mentions rare adnexal tumors with a predilection for the eyelid, e.g., sebaceous neoplasms and endocrine mucin-producing sweat gland carcinoma, as well as unique lesions of the eyelid, e.g., phakomatous choristoma and intratarsal keratinous cysts. This material is aligned with the 5th edition of the WHO classification of tumors of the skin, specifically concerning cutaneous melanocytic tumors (4). Specialists performed all the procedures, and a pathologist reported the histopathological types of the tumors. Information on sex, age, location of the tumor, and recurrences was also collected. Absolute numbers and percentages were used for binary and categorical variables, while means, standard deviations (SD), and 95% confidence intervals (CIs) (95% CI) were utilized for continuous variables. Chi-square and independent samples t tests were used for group collation.
4. Results
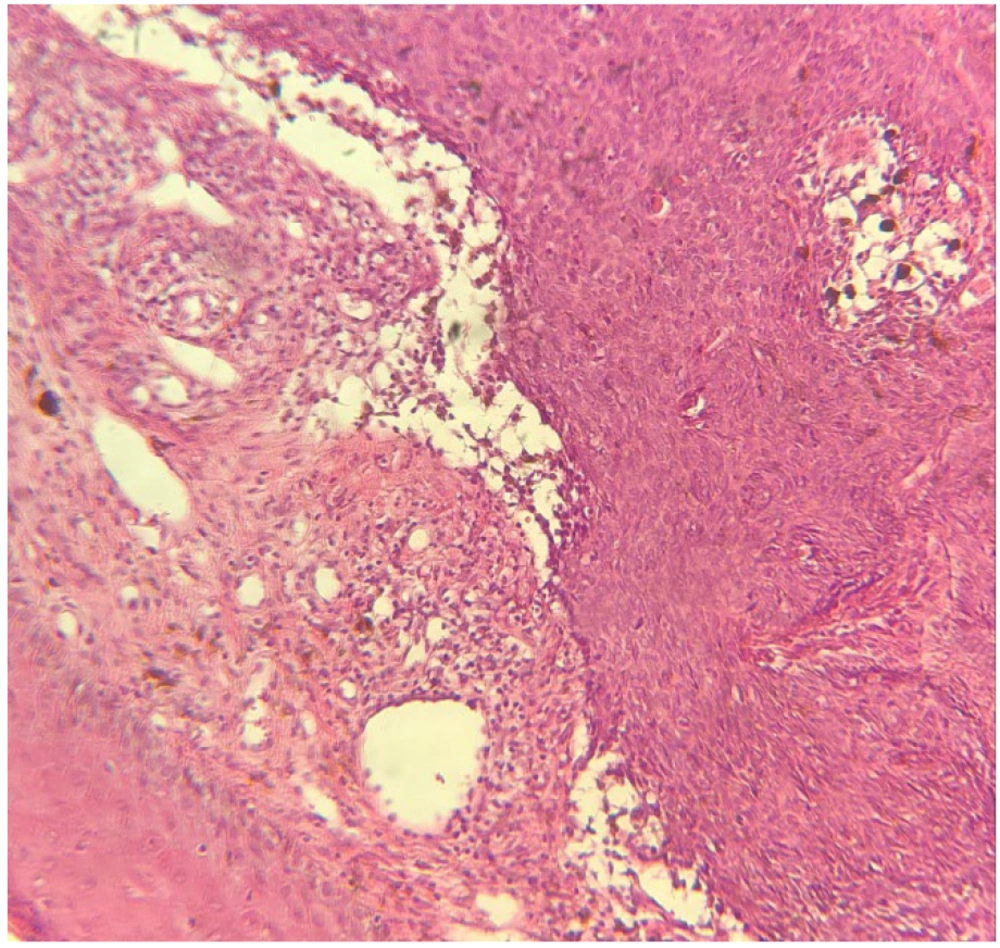
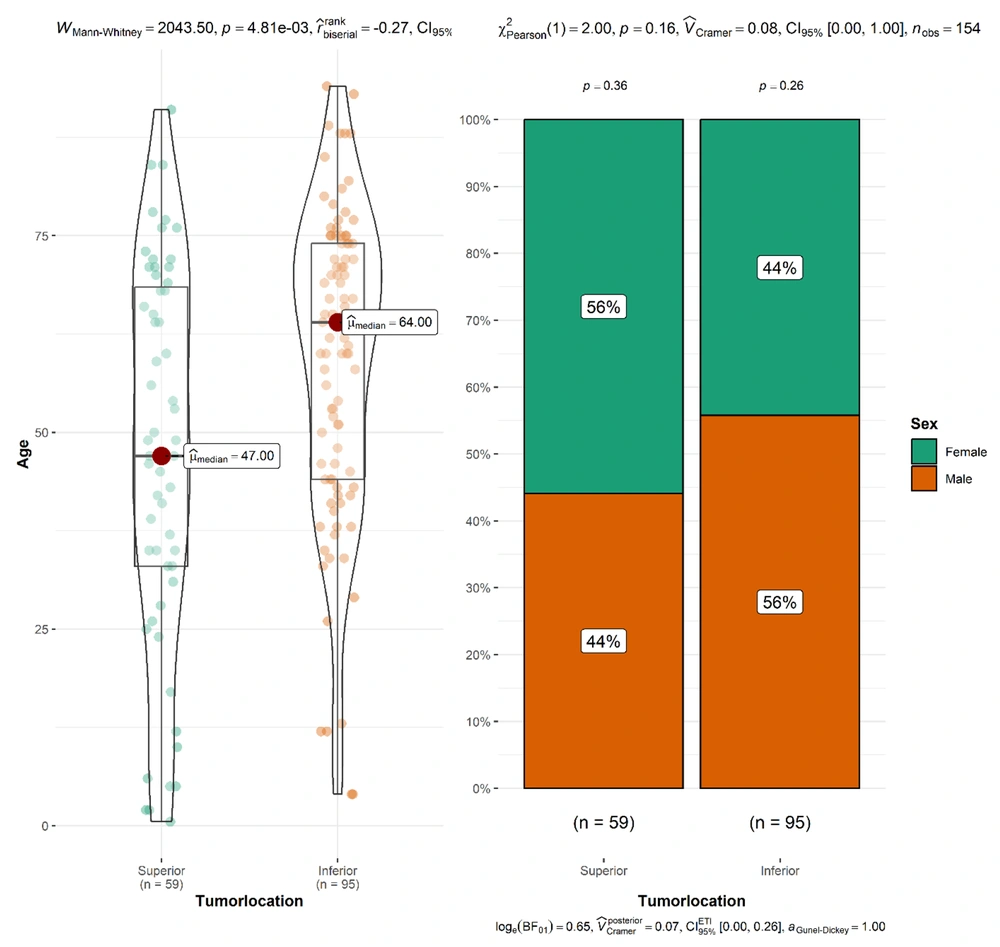
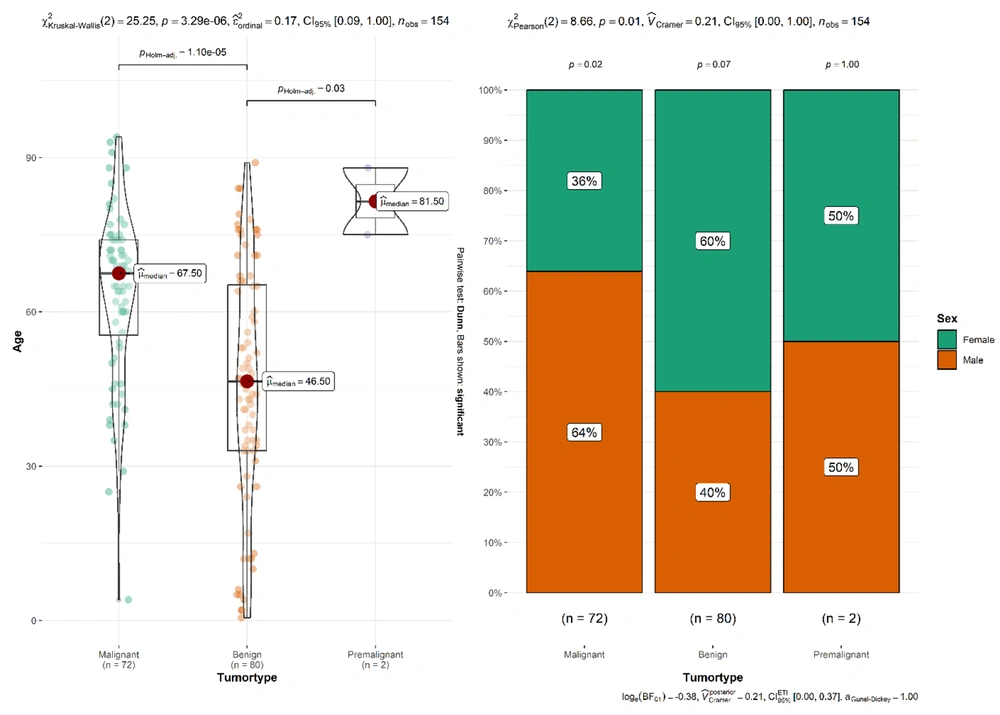
A total of 154 specimens (72 malignant, 80 benign, and 2 premalignant tumors) from 79 (51.3%) males and 75 females (48.7%) were retrieved and analyzed. The mean age was 45.8 ± 23.06 years for patients with benign lesions, 63.5 ± 16.7 years for patients with malignant lesions, and 81.5 ± 9.19 years for premalignant lesions (Table 1). For malignant tumors, there were 81.9% (59 cases) basal cell carcinomas (BCC) (Figure 1), 15.3% (11 cases) basosquamous cell carcinomas (BSC), and 1.4% (1 case) squamous cell carcinomas (SCCs).
| Variables | Overall, N = 154 a | Malignant, N = 72 a | Benign, N = 80 a | Premalignant, N = 2 a | P-Value b |
|---|---|---|---|---|---|
| Age (y) | 54.5 (22.18) | 63.5 (16.70) | 45.8 (23.06) | 81.5 (9.19) | < 0.001 |
| Sex | 0.006 | ||||
| Male | 79 (51) | 46 (64) | 32 (40) | 1 (50) | |
| Female | 75 (49) | 26 (36) | 48 (60) | 1 (50) | |
| Tumor location | < 0.001 | ||||
| Superior | 59 (38) | 15 (21) | 44 (55) | 0 (0) | |
| Inferior | 95 (62) | 57 (79) | 36 (45) | 2 (100) | |
| Recurrence | 0.061 | ||||
| No | 149 (97) | 67 (93) | 80 (100) | 2 (100) | |
| Yes | 5 (3.2) | 5 (6.9) | 0 (0) | 0 (0) |
a Mean (SD); No. (%)
b Kruskal-Wallis rank-sum test; Fisher's exact test
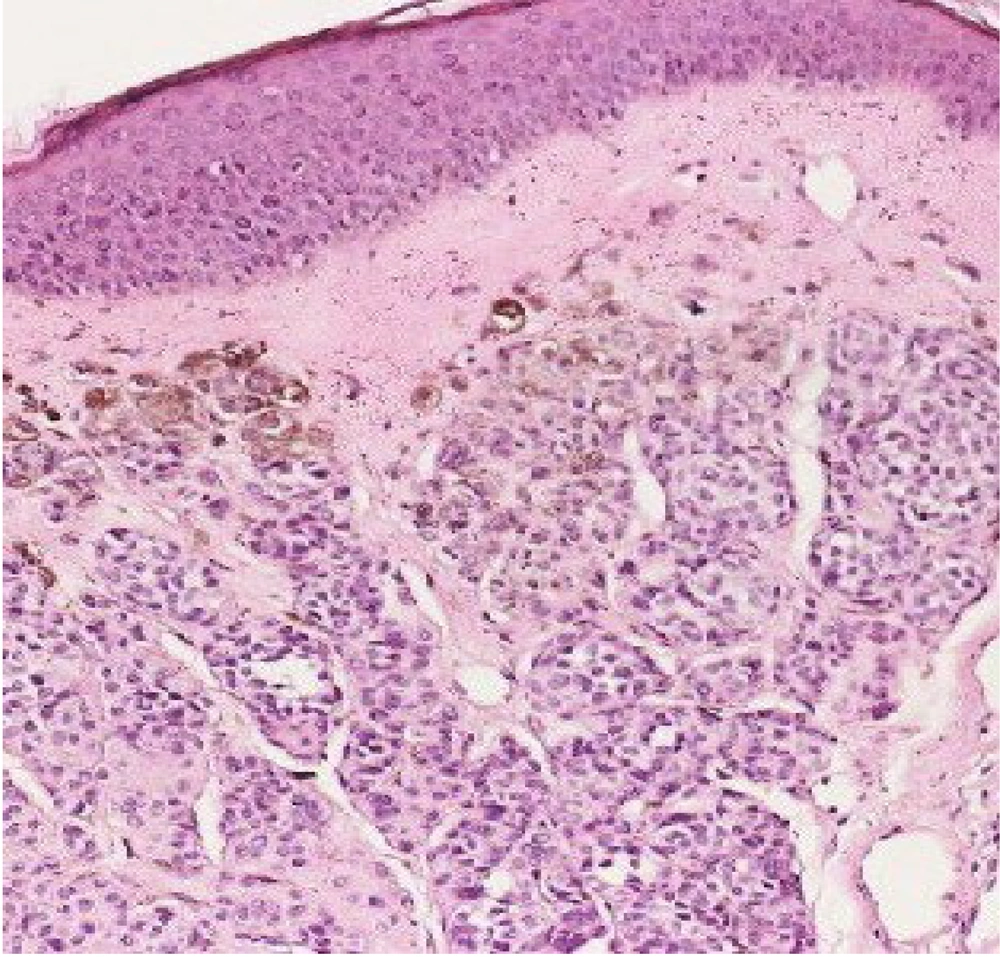
The benign eyelid lesions were comprised of 20% intradermal melanocytic nevus (Figure 2), 11.3% epidermal cyst, 7.6% dermoid cyst, 10% seborrheic keratosis, 6.3% xanthelasma, 2.5% wart, 3.8% compound nevus, 5% fibroconnective tissue, 3.8% squamous papilloma, 3.8% neurofibroma, 2.5% comedone, 2.5% apocrine hidrocystoma, 2.5% foreign body type granuloma, and 1.3% of others (arteriovenous hemangioma, cavernous hemangioma, cutaneous horn, eccrine hidrocystoma, epidermal nevus, inverted follicular keratosis, and osteoma pyogenic granuloma). The premalignant lesions were 2 cases of actinic keratosis. Malignant tumors were located on the lower eyelid in 79% of cases and on the upper eyelid in 21% of the cases (Table 2).
a Mean (SD); No. (%)
b U Mann-Whitney U test; Pearson's chi-squared test; Fisher's exact test
Benign lesions were seen in 55% of the cases in the upper lids and in 45% of the cases in the lower lids (Figure 3). All cases of premalignant lesions occurred in the lower eyelids. In our study, 63.6% (7) of the patients with BCC were male, and 36.4% (4 cases) were female (Figure 4).
5. Discussion
In our study, about 47% of the tumors were malignant. It is important to increase the awareness of health care workers and the public regarding eyelid lesions in Iranian populations exposed to solar radiation. Also, 52% of the eyelid lesions were benign. This contrasts with data from Switzerland 1 (84% benign lesions), China 5 (86.2% benign lesions), and Greece (59% benign lesions) 1. Differences in the study populations, study methods, and the health care systems may justify the statistical differences. Patients with benign lesions were younger than patients with malignant lesions, in contrast to previous studies (1, 2, 5, 6).
Benign lesions have an almost equal frequency in the upper and lower eyelids; on the contrary, malignant tumors are found most often in the lower eyelid. This difference may be related to the increased solar exposure of the lower eyelid. Results of studies from other countries may show differences. In a study from Greece, the most common malignancy was BCC (86%); the second one was SCC (7%), the third one was basosquamous cell carcinoma (5%), and the last one was malignant melanoma (2%) (1). Another study from Switzerland showed that BCC was the most common eyelid malignancy (84%), followed by SCC (7%) and sebaceous carcinoma (3%) (2). A study which was done in Taiwan reported BCC (65.1%) as the most common malignant tumor, followed by SCC (12.6%) and sebaceous carcinoma (7.9%) (7). A study from Germany between 2009 and 2015 showed that BCC was the most common eyelid malignancy, followed by SCC and malignant melanoma (8). Another study from Pakistan showed that SCC was the most common malignancy of the eyelid (9). In one study from Sri Lanka, the most common malignant tumor of the eyelid was sebaceous carcinoma (10). Sebaceous carcinoma is the second most common malignancy of the eyelid in some studies, while SCC is the third (11). These differences in studies may be due to variations in population, disease awareness, and health care system (7). Basal cell carcinomas are usually local lesions and rarely lead to death (1). Basal cell carcinoma has an average age of 67 years, but a few patients younger than 40 years and a few pediatric patients with basal cell carcinoma were reported (3). Squamous cell carcinoma has the second place in most common eyelid malignant tumors in Western countries. The different ratios of SCC in different studies may be due to similar histologic features of SCC to other lesions (9). Malignant eyelid tumors other than BCC and SCC are rare and usually seen in elderly people (1). Malignant melanoma is a poor prognostic malignancy with a high mortality rate (3, 12). In our study, there is no case of malignant melanoma. In our study, there is no case of sebaceous carcinoma. This malignancy is very rare in contrast to BCCs but more common in some studies of the Asian population (6, 12-14). This malignancy may be underdiagnosed with similar histologic findings of sebaceous carcinomas from benign lesions (e.g., chalazion and blepharitis) and malignant lesions such as squamous cell carcinoma (11). In our study, malignant lesions included 81.9% basal cell carcinomas, 15.3% basosquamous cell carcinomas, and 1.4% squamous cell carcinoma. Finally, our study showed that benign eyelid lesions are generally seen in younger patients and have an equal frequency of upper and lower lids. On the contrary, malignant tumors were seen mostly in elderly persons and mostly in the lower eyelid.
5.1. Conclusions and Future Research
In the current study, benign eyelid lesions were seen predominantly in younger persons, and malignant tumors were seen mostly in elderly persons. Malignancy had an equal ratio of males and females. There were rare recurrence lesions after excision to the eyelid. In the future, research on the molecular genetics of eyelid tumors of the Iranian population and possible directions toward diagnosing and treating cutaneous tumors is recommended.