1. Background
Genital diseases are prevalent and can be painful and distressing. They are associated with psychosocial stigma and disrupt self-image (1). In developing countries, reproductive tract infections (RTIs) and sexually transmitted infections (STIs) are major public health problems (2) and rank among the top 10 diseases in India for which adults seek care. According to the National AIDS Control Organization (NACO) report 2016–17, 6% of the adult population in India reports RTI/STIs every year (3).
Sexually transmitted infections/reproductive tract infections significantly impact the quality of life, causing morbidity and sometimes mortality. They might lead to infertility, cancers, and pregnancy complications, impact reproductive and child health, and promote the transmission of human immunodeficiency virus (HIV) (4). The increase in HIV-seropositive patients has led to an upsurge in genital and non-genital malignancies (5).
In 2019, there were an estimated 23.49 lakh people living with HIV (PLHIV) in India, with an adult (15 - 49 years) HIV prevalence of 0.22% and children accounting for 3.4% (6). Sexually transmitted infections, usually associated with genital manifestations, act as co-factors of HIV transmission. Genital lesions can have varied clinical presentations, and this knowledge can help in early diagnosis and better prognosis (7). Timely treatment of STIs has been shown to reduce the transmission rate of HIV infection by more than 40% (3).
Genital lesions are also often encountered in pediatric patients, an aspect that tends to be overlooked (8). The patterns of genital lesions might vary with factors such as age, gender, socioeconomic strata, and HIV status. Despite the huge impact of these lesions on individuals, families, and society at large, the importance of their public health remains an under-appreciated and neglected topic.
2. Objectives
The primary objective was to document the clinical profile and socio-demographic data of patients presenting with genital lesions and to identify common etiologies. Secondary objectives included analyzing the correlation of various parameters and determining the factors contributing to the development of genital lesions. Additionally, the present study sought to determine the proportions of pediatric and HIV seropositive patients.
3. Methods
This hospital-based cross-sectional observational study was conducted at a tertiary care hospital in Pune, Maharashtra State, India, over a two-month period within July to August 2022. All patients attending the outpatient and inpatient departments of Dermatology and Pediatrics during this period were screened. Those presenting with genital lesions were included in the study. Informed consent was obtained from patients or parents/legal guardians (for patients under 18 years of age) in the vernacular language (Marathi/Hindi) or English. Subjects aged under 12 years and between 13 and 18 years were included in pediatric and adolescent age groups, respectively. Patients without written informed consent were excluded. Convenience sampling was performed based on the census method. All patients or their relatives were assured of strict confidentiality. Institutional Ethics Committee approval was obtained.
The patients underwent a detailed history-taking process using a predesigned proforma. The information gathered included chief complaints, site of onset of lesion, progression, presence of lesions elsewhere on the body, ameliorating/exacerbating factors, history of chronic illness or prior similar complaints, and personal, sexual, family, or drug history.
Clinical examinations were conducted, followed by relevant microbiological, serological, and histopathological investigations, and the final diagnoses of genital lesions were made by one of the investigators (second author, associate professor in the Department of Dermatology). Medical records were scrutinized to document patient demographics (e.g., registration number, age, gender, address, education, occupation, family income, religion, and socioeconomic status using the Modified Kuppuswamy Scale) and laboratory investigations and reports (including HIV status and CD4 count).
The etiology of genital lesions was classified into infectious or non-infectious and STIs or non-STIs. Infectious lesions were subdivided into five categories: Viral, bacterial, fungal, parasitic, and treponemal. Non-infectious lesions were classified into three categories: Inflammatory, benign, and malignant lesions. The presence of risk factors was assessed. Proportions of pediatric and HIV-seropositive patients were calculated.
The data were compiled and entered on MS Excel sheets and analyzed using SPSS software version 23. Qualitative data were expressed as frequency and percentages; quantitative data were expressed as mean and standard deviation. The Chi-square test and student t-test were applied to find any association between study variables, and a p-value of < 0.05 at a 95% confidence interval was considered significant.
4. Results
4.1. Demographics and Risk Factors
Out of the total 83 patients enrolled, 80 were adults (77, 92.8%) and adolescents (3, 3.6%). Pediatric and HIV-seropositive patients comprised 3.6% and 18.07%, respectively. In this study, 44 patients were male (55%), and the rest were female (36, 45%). The adult male-to-female ratio was 1.2:1. All pediatric and adolescent patients were female. The mean age of adult patients was 37.01 ± 14.57 years. For HIV-seropositive, adolescent, and pediatric patients, the mean ages were 40.4 ± 13.29, 17.33 ± 2.1, and 5 ± 1.63 years (range: 3 - 7 years), respectively.
The majority of patients were residents of urban areas (96.3%) and educated up to middle school (25%). Moreover, 91.3% were Hindu by religion, and 67.5% belonged to upper lower (IV) socio-economic category.
Overall, 95% were heterosexual, and 5% were men who have sex with men (MSM) (bisexual orientation). Among the HIV-seropositive patients, 93.3% were heterosexuals, and 6.7% were MSM.
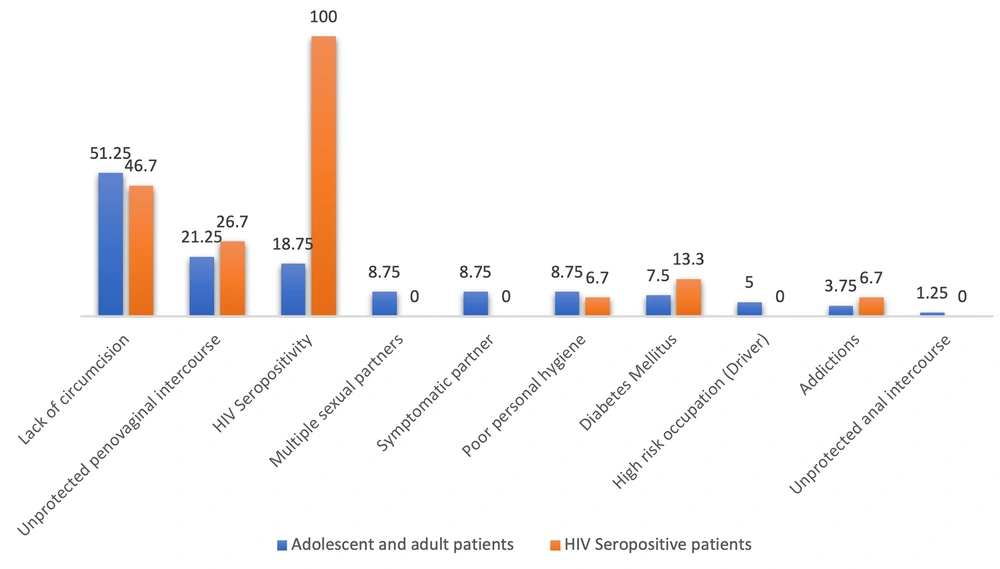
Figure 1 describes the distribution of risk factors among adult and HIV-seropositive patients. Table 1 shows the association between gender and various study parameters. There was a significant association between male gender and the presence of risk factors (P = 0.0001).
| Variables | Female | Male | Total | P-Value |
|---|---|---|---|---|
| Age, y | 35.64 ± 13.7 | 38.14 ± 15.2 | 0.449 | |
| Monthly income, INR (Indian rupee) | 9966.67 ± 5804.18 | 13511.36 ± 12308.3 | 0.116 | |
| Risk factors | 19 (30.6) | 43 (69.4) | 62 | 0.0001 |
| HIV seropositive patients | 9 (60) | 6 (40) | 15 | 0.195 |
| Diseases | ||||
| STI/non-STIs | - | |||
| STIs | 13 (37.1) | 22 (62.9) | 35 | |
| Non-STI | 21 (51.2) | 20 (48.8) | 41 | |
| Mixed | 2 (50) | 2 (50) | 4 | |
| Infectious/non-infectious | 0.333 | |||
| Infectious | 29 (42) | 40 (58) | 69 | |
| Non-infectious | 7 (63.6) | 4 (36.4) | 11 | |
Abbreviations: HIV, human immunodeficiency virus; SD, standard deviation; STI, sexually transmitted infection.
a Values are presented as No. (%) or mean ± SD.
4.2. Etiological Distribution and Clinical Profile
The majority of patients were 21 - 30 years old (37.5%), with the highest number of patients with infectious etiology belonging to this age group (40.6%). Moreover, 36.4% of patients with non-infectious etiology were between 31 - 40 years. The infectious-to-non-infectious ratio was the highest and lowest in the 21 - 30 (14: 1) and 51-60 (2.5: 1) years age groups, respectively.
There was an overlap of patients with STI and non-STI etiology, with four patients presenting with both types of lesions. The ratio of STI to non-STI lesions was 1: 1.15. Tables 2 and 3 show the etiology of STI and non-STI lesions, respectively. A case of genital mucormycosis (Figure 2), a rare non-STI, was encountered in this study.
| Etiology | Female (n = 15) | Male (n = 24) | Total (n = 40) |
|---|---|---|---|
| Fungal infection | 8 (80) | 2 (20) | 10 (25) |
| Candidial balanoposthitis | 0 | 2 (100) | 2 (20) |
| Vulvovaginal candidiasis | 8 (100) | 0 | 8 (80) |
| Viral infection | 4 (23.5) | 13 (76.5) | 17 (42.5) |
| Genital molluscum contagiosum | 0 | 2 (100) | 2 (11.8) |
| Herpes genitalis | 1 (11.1) | 8 (88.9) | 9 (52.9) |
| Genital warts | 3 (50) | 3 (50) | 6 (35.3) |
| Bacterial infection | 1 (25) | 3 (75) | 4 (10) |
| Gonorrhoea | 0 | 2 (100) | 2 (50) |
| Chancroid | 0 | 1 (100) | 1 (25) |
| Bacterial vaginosis | 1 (100) | 0 | 1 (25) |
| Treponemal infection (syphilis) | 3 (33.3) | 6 (66.7) | 9 (22.5) |
| Parasitic infection | 0 | 0 | 0 |
a Values are expressed in number (%) unless otherwise indicated.
| Etiology | Female (n = 23) | Male (n = 25) | Total (n = 48) |
|---|---|---|---|
| Fungal infection | 14 (53.8) | 12 (46.2) | 26 (54.2) |
| Tinea cruris | 11 (55) | 9 (45) | 20 (76.9) |
| Vulvovaginal candidiasis | 3 (100) | 0 | 3 (11.6) |
| Candidial balanoposthitis | 0 | 2 (100) | 2 (7.7) |
| Mucormycosis | 0 | 1 (100) | 1 (3.8) |
| Bacterial infection | 0 | 1 (100) | 1 (2.1) |
| Secondary infection to genital scabies | 0 | 1 (100) | 1 (100) |
| Parasitic infection (genital scabies) | 2 (28.6) | 5 (71.4) | 7 (14.6) |
| Inflammatory | 3 (42.9) | 4 (57.1) | 7 (14.6) |
| Lichen sclerosus et atrophicus | 1 (50) | 1 (50) | 2 (28.5) |
| Chronic plaque psoriasis | 0 | 1 (100) | 1 (14.3) |
| Eczema | 0 | 1 (100) | 1 (14.3) |
| Balanitis xerotica obliterans | 0 | 1 (100) | 1 (14.3) |
| Keloid | 1 (100) | 0 | 1 (14.3) |
| Behcet disease | 1 (100) | 0 | 1 (14.3) |
| Benign tumor | 2 (50) | 2 (50) | 4 (8.3) |
| Steatocystoma multiplex | 0 | 2 (100) | 2 (50) |
| Vulval syringoma | 1 (100) | 0 | 1 (25) |
| Bowen disease | 1 (100) | 0 | 1 (25) |
| Malignant tumor (SCC) | 2 (66.7) | 1 (33.3) | 3 (6.2) |
Abbreviation: SCC, squamous cell carcinoma.
a Values are expressed in number (%) unless otherwise indicated.
Among HIV-seropositive individuals, most had fungal (33.3%) and viral (26.7%) lesions. Herpes genitalis was the most common disease overall. Two patients had squamous cell carcinoma (SCC). Table 4 shows the etiological distribution of lesions in pediatric and adolescent patients.
| Variables | Value |
|---|---|
| Pediatric patients | |
| Etiology; total (n = 3) | |
| Inflammatory | 1 (33.3) |
| Lichen sclerosus et atrophicus | 1 (100) |
| Bacterial infection | 1 (33.3) |
| Ecthyma gangrenosum | 1 (100) |
| Fungal infection | 1 (33.3) |
| Vulvovaginal candidiasis | 1 (100) |
| Adolescent patients | |
| Etiology; total (n = 3) | |
| Fungal infection | 2 (66.7) |
| Tinea cruris | 1 (50) |
| Vulvovaginal candidiasis | 1 (50) |
| Viral infection | 1 (33.3) |
| Genital warts | 1 (100) |
a Values are expressed in number (%) unless otherwise indicated.
The most common presenting complaint among adult patients was pruritus (50%), and 16.25% had asymptomatic lesions. The predominant examination finding was genital ulcers (21.25%). A similar clinical profile was observed among HIV-seropositive patients (Table 5).
| Variables | Total |
|---|---|
| Age group (y) | |
| 12 - 20 | 5 (6.3) |
| 21 - 30 | 30 (37.5) |
| 31 - 40 | 18 (22.5) |
| 41 - 50 | 13 (16.3) |
| 51 - 60 | 7 (8.8) |
| > 60 | |
| Gender | 7 (8.8) |
| Male | 44 (55) |
| Female | |
| Risk factors | 36 (45) |
| Lack of circumcision | 41 (51.25) |
| Unprotected penovaginal intercourse | 17 (21.25) |
| HIV Seropositivity | 15 (18.75) |
| Multiple sexual partners | 7 (8.75) |
| Symptomatic partner | 7 (8.75) |
| Poor personal hygiene | 7 (8.75) |
| Diabetes mellitus | 6 (7.5) |
| High-risk occupation (driver) | 4 (5) |
| Addictions | 3 (3.75) |
| Unprotected anal intercourse | |
| Symptoms | 1 (1.25) |
| Pruritus | 40 (50) |
| Asymptomatic lesions | 13 (16.25) |
| Whitish vaginal discharge | 12 (15) |
| Pain | 9 (11.25) |
| Ulcer | 9 (11.25) |
| Dysuria | 7 (8.75) |
| Purulent urethral discharge | 4 (5) |
| Fluid-filled lesion | 4 (5) |
| Painful erection | 1 (1.25) |
| Bloody urethral discharge | 1 (1.25) |
| Bleeding on scratching | 1 (1.25) |
| Burning sensation | |
| Examination findings | 1 (1.25) |
| Ulcer | 17 (21.25) |
| Papules | 13 (16.25) |
| Annular hyperpigmented plaque with scaling | 12 (15) |
| Vaginal discharge | 9 (11.25) |
| Erythema | 8 (10) |
| Erosions | 6 (7.5) |
| Hyperpigmented plaque | 5 (6.25) |
| Tenderness | 5 (6.25) |
| Excoriations | 4 (5) |
| Nodules | 3 (3.75) |
| Verrucous growth | 3 (3.75) |
| Hypopigmentation | 2 (2.5) |
| Urethral discharge | 2 (2.5) |
| Phimosis | 2 (2.5) |
| Eczematization | 1 (1.25) |
| Keloid | 1 (1.25) |
| Vaginal stenosis | 1 (1.25) |
a Values are presented as No. (%).
5. Discussion
The present study demonstrated that the number of males affected was slightly higher, with a male-to-female ratio of 1.2:1, in accordance with Pottipati et al.’s study (9), which reported a ratio of 1.24:1. This slender male preponderance might be attributed to associated stigma among females, along with consultation for genital complaints in other departments, such as gynecology, rather than dermatology.
Of the adult patients, 67.5% were legally married, and 54% of the unmarried individuals were involved in sexual activities. Among sexually active individuals, a ‘ping-pong effect’ might be observed, wherein sexual partners recurrently re-infect each other with the same STI if not treated concurrently. This emphasizes that notification, screening, and simultaneous treatment of the partner are imperative for STI control. In the current study, one in four MSM (bisexual) patients was HIV-seropositive (25%), highlighting the higher prevalence of STIs, including HIV, in this high-risk group (10). The MSM individuals should, therefore, be prioritized and counseled about safe sexual practices for risk reduction.
Tekam et al. (11) reported that over half of their participants presented with STIs. In the present study, the proportion of non-STI cases (53.75%) was marginally higher, with a higher number of males in the sexually active age group, potentially due to a greater propensity for high-risk sexual behavior. The presence of one or more risk factors was significantly higher in males (69.4%) than in females (30.6%).
The majority of non-STI cases had lesions of fungal etiology, with tinea cruris leading the list. Pottipati et al. (9) and Tekam et al. (11) reported vitiligo and candidial balanoposthitis as the most common non-STI lesions, respectively.
Similar to Marcos-Pinto et al.’s study (12), the present study showed that SCC was the most frequent malignant lesion. An interesting case involved a 26-year-old HIV-seropositive woman presenting with a fungating growth over labia majora, who was diagnosed as poorly differentiated SCC upon histopathology. Human papillomavirus (HPV)-DNA polymerase chain reaction (PCR) was positive for subtype 16. Human papillomavirus types 16 and 18 are classified as high-risk HPV (HR-HPV), and their association with genital warts is strongly linked to cervical dysplasia (13). Therefore, in the case of genital condyloma, HPV typing holds predictive value for the development of genital SCC, and its screening and timely management are imperative to avert genital malignancies.
Another notable case was a 49-year-old male diabetic who presented with ulcers over the penile shaft, with purulent bloody urethral discharge for one month. He had a history of a recent dorsal slit procedure performed in view of impending penile gangrene. Upon examination, multiple preputial ulcers and segmental gangrene on the glans penis were observed. The demonstration of characteristic fungal elements on potassium hydroxide mount and histopathology led to the diagnosis of mucormycosis, a potentially life-threatening opportunistic infection caused by Zygomycetes, typically affecting immunocompromised individuals. Uncontrolled diabetes likely predisposed him to this condition. Genital mucormycosis is extremely rare.
The majority of patients with STIs had lesions of viral etiology (42.5%), with herpes genitalis being the most common, consistent with Tekam et al.’s findings (11). Nevertheless, Wildsmith et al. (14) reported chlamydia as the foremost cause. The higher prevalence of herpes reflects the changing trends in STI patterns in India (15). This finding might be attributable to the syndromic approach (16) implemented for their management instead of the identification of specific etiology.
Tekam et al. (11) demonstrated that herpes genitalis and genital warts were the predominant STIs in males and females, respectively. In the present study, the most common STI in males was herpes; however, in females, it was vulvovaginal candidiasis, consistent with Elfaituri S’ findings (17).
In the present study, one or more identifiable risk factors were present in 77.5% of subjects, with the predominant ones being lack of circumcision (51.25%), unprotected intercourse (22.5%), HIV seropositivity (18.75%), and multiple sexual partners, symptomatic partner, and poor personal hygiene (8.75% each). Wildsmith et al. (14) reported that 64% of patients had one or more identifiable risk factors, including multiple sexual partners, symptomatic partners, and unprotected intercourse.
Among those with risk factors, the majority (87.1%) had a primary diagnosis of infectious etiology. Therefore, identifying and educating patients regarding modifiable risk factors might be instrumental in minimizing genital diseases.
Only 5.3% of patients in the STI category and 8.7% in the non-STI category were circumcised. Circumcision has been demonstrated to provide protection against STIs and penile cancer (18). Circumcision reduces the risk of oncogenic HPV by 32-35% and that of HR-HPV, bacterial vaginosis, and trichomoniasis in female partners by 28%, 40%, and 48%, respectively (19, 20).
The present study revealed that 86.25% of patients had a primary diagnosis of infectious etiology, emphasizing that infectious diseases still contribute considerably to the burden of genital diseases. The maximum number of cases belonged to the age group of 21 - 30 years (41%), suggesting a higher probability of indulgence in high-risk behavior within this age group.
Pruritus was the most common symptom, as also observed by Pottipati et al. (9). The second-highest number of patients were asymptomatic. The most frequent examination finding was ulcers, often an incidental feature on clinical examination rather than a presenting complaint. The lack of symptoms and their obscure location lead to genital lesions remaining unnoticed and neglected until these patients present at advanced stages with complications that could have been averted. This finding highlights the importance of meticulous clinical examination in the management of genital diseases.
Among HIV-seropositive patients, 63.3% had non-STIs, contrary to a previous study (11) in which 77% of HIV-seropositive patients had STIs. The human immunodeficiency virus is known to be associated with STIs (21); however, its relationship with non-STIs has still not been established and warrants further research.
All three adolescent females in the current study were post-pubertal, and two of them were married despite being younger than the legally permissible age of 18 years. This finding highlights the inherent risks of early-age sexual debut, particularly the acquisition of STIs, such as condyloma acuminata and candidiasis, as encountered in the studied adolescent subjects. It also supports the need for immunization of all young males and females with HPV vaccines.
All three pediatric subjects were females with non-STI dermatoses (ecthyma gangrenosum, vulvovaginal candidiasis, and lichen sclerosus et atrophicus). The presence of STIs in the pediatric population warrants thorough scrutiny for sexual abuse. However, no such history could be elicited in any of these children. Mekala et al. (22) reported that among pre-pubescent females, vulvovaginitis was the most common.
5.1. Strengths and Limitations
This study is novel, offering a comprehensive clinico-etiological and demographic compilation of all genital lesions (both venereal and non-venereal) across age and gender. It was impossible to find any similar studies documenting all the variables to compare to the findings of the current study. The limitation was the small sample size, owing to a brief period of data collection. This issue probably resulted in a small number of cases in each category; therefore, statistical analysis could not reflect the association between various parameters. In some cases, elaborate sexual history could not be elicited due to awkwardness and stigma, which might have led to recall bias and missing data.
5.2. Conclusions
This study emphasizes that although STIs remain a prominent cause of genital lesions, particularly in young sexually active individuals, non-STIs also contribute significantly and should be focused on. Therefore, measures for their prevention and control ought to be intensified. A detailed history is imperative to identify risk factors among these patients. Partner notification, screening, and treatment are necessary for the control and management of STIs. It is fundamental to perform an adequate anamnesis, beginning with particulars of sexual contacts (including abuse), fortified by meticulous clinical examination and relevant laboratory investigations for accurate diagnosis and management. Screening for HIV should be performed in all patients with genital lesions, especially with STI etiology. It is paramount to identify venereal dermatoses in children and adolescents since it might provide vital clues for sexual abuse. Genital lesions remain a major public concern and a source of embarrassment for patients, highlighting the unmet need for community sensitization to alleviate the stigma and counseling regarding safer sexual practices.