1. Context
Temporal skin arteriovenous malformations (AVMs), though less common than their cerebral counterparts, constitute a unique clinical entity in dermatological and vascular anomaly practice. Skin AVMs, including those in the temporal area, are part of a broader category of vascular malformations, with an approximate incidence of 1.5% in the general population. However, specific data on temporal skin AVMs are limited due to their rarity. Typically congenital, these lesions usually become clinically apparent during childhood or adolescence. They may remain stable in size or exhibit growth, often in response to hormonal changes such as puberty or pregnancy. Unlike cerebral AVMs, which present a significant risk of hemorrhage, temporal skin AVMs primarily pose cosmetic concerns (Figure 1) and, in some cases, can lead to pain, bleeding, or ulceration (1).
An AVM of the left temporal skin area causing serious cosmetic deficit in a patient who presented for evaluation and treatment at our outpatient clinic. A brain MRA showed arterial inflow from branches of the left external carotid artery – specifically the posterior auricular and the superficial temporal arteries (Courtesy of Dr. Konstantinos Roditis, vascular surgeon, Athens, Greece).
Recent epidemiological studies indicate a slight male predominance in cutaneous AVM occurrences. The specific prevalence of temporal skin AVMs within this demographic has not been thoroughly investigated. However, advancements in diagnostic imaging are likely contributing to an increased identification of these lesions (2).
Recent research has focused on uncovering genetic factors influencing AVM development, identifying mutations and pathways that may offer insights into targeted therapies. There is no conclusive evidence suggesting significant variance in AVM prevalence based on geography or ethnicity. The global incidence appears uniform, although differences in healthcare access and reporting standards across regions may influence this observation (3, 4).
Temporal skin AVMs, especially when noticeable, extend beyond physical symptoms and significantly affect psychological and social well-being, particularly in younger patients. This emphasizes the need for both medical and psychological support in their management (5). With this study, we aim to provide a comprehensive overview of the pathophysiology and clinical implications of temporal skin AVMs, assess the latest diagnostic modalities and treatment strategies, and explore the challenges in managing these lesions and future research directions.
2. Evidence Acquisition
To compile a comprehensive understanding of the recent advances in AVMs of the temporal skin area, a literature review was conducted. This review specifically targeted publications from the past decade to ensure the inclusion of the latest research and developments in this field.
2.1. Search Strategy
The literature search utilized PubMed, Scopus, and Google Scholar, chosen for their extensive collections of medical and scientific literature. Limited to the last decade, the search focused on recent data and developments. A combination of keywords such as "temporal skin arteriovenous malformations" and "cutaneous AVMs" was employed to broaden the scope. The aim was to include peer-reviewed articles, clinical trials, case reports, and comprehensive reviews relevant to the pathophysiology, diagnostics, and treatment of temporal skin AVMs. Thirteen publications were identified (3-15). Articles older than ten years, non-peer-reviewed articles, and studies not specifically addressing AVMs in the temporal skin area were excluded.
3. Results
3.1. Pathophysiology and Clinical Presentation
Sudduth et al. provided new insights into the genetic basis of cutaneous AVMs, highlighting the role of a specific gene mutation. They explored the role of the MAP2K1 mutation in arteriovenous malformation. Using droplet digital PCR and RNA sequencing, they analyzed the effects of this mutation in endothelial cells (ECs). The study revealed that the MAP2K1 mutation led to significant changes in gene expression related to cell migration, adhesion, matrix organization, tube morphogenesis, angiogenesis, and blood vessel development. This was evidenced by a marked upregulation of genes such as COL15A1, Itgb3, Piezo2, and Cd109, all of which play roles in vascular and angiogenic processes. This discovery has implications for understanding the pathophysiology of AVMs and potentially for targeted therapeutic approaches (6).
A recent nationwide cohort study in Korea investigated the incidence and mortality associated with various types of extracranial vascular malformations, including AVMs. The study revealed an annual incidence of 9.85 cases per 100,000 population for all extracranial vascular malformations, with a specific incidence rate of 0.24 cases per 100,000 population for AVMs. The study also noted a higher incidence rate among females compared to males for all subtypes of vascular malformations, with the most significant proportion observed in AVMs (7).
AVMs may become noticeable or worsen due to hormonal changes during puberty or pregnancy. Many vascular malformations are congenital and may only manifest later in life, possibly triggered by hormonal shifts. In a study published in the European Journal of Medical Research, researchers investigated hormone receptor expression in the vascular walls of various malformations, including AVMs. The focus was on the potential influence of hormones like estrogen and follicle-stimulating hormone (FSH) on angiogenesis. This research implies that hormonal changes, especially during puberty or pregnancy, might impact the growth and behavior of AVMs (8).
3.2. Diagnostic Techniques
Ongoing research in the field has yet to yield specific comparative studies exclusively focusing on the efficacy of magnetic resonance angiography (MRA), computed tomography angiography (CTA), and high-resolution ultrasound for diagnosing temporal skin AVMs. Current literature indicates that each imaging modality has its strengths, with suitability varying based on the clinical scenario. A study by Yip et al. demonstrated ultrasound's effectiveness in detecting vasculitic changes, showing comparable diagnostic accuracy to MRI. The study also suggested that ultrasound detected vasculitic changes more frequently in the supra-aortic arteries than magnetic resonance angiography (MRA), indicating potentially higher resolution in certain cases. Further research in this area is warranted (9). Other scientists have demonstrated that high-resolution MRA is capable of accurately detecting and measuring vascular morphological characteristics, such as the degree of stenosis, tortuosity, and aneurysmal dilatation, and is more sensitive than CTA in a sample of high-risk, symptomatic patients (10).
3.3. Treatment Advances
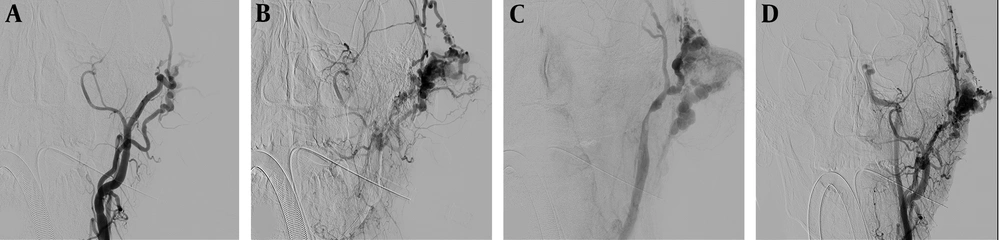
Advanced surgical techniques, combined with embolization and laser therapy, underscore the significance of a personalized treatment approach for scalp AVMs, taking into account lesion characteristics and patient preferences. A case series in Frontiers in Neurology detailed successful endovascular treatment of two scalp AVM cases through direct percutaneous catheterization. The study highlighted effective embolization, resulting in reduced mass size and the absence of pulsation post-treatment. Follow-up assessments, including cerebral angiography a year later, revealed no recurrence or evidence of skin necrosis (11). These outcomes suggest the effectiveness of the endovascular approach (Figure 2) in managing scalp AVMs, which could be analogous to temporal skin AVMs due to similarities in vascular structure and accessibility.
Selective diagnostic DSA of the left external carotid artery of the same 36-year-old patient, revealing the AVM originating from the posterior auricular and superficial temporal arteries (A, B) and communicating with the ipsilateral internal jugular vein (C). Post-embolization completion DSA of the same case, showing partial occlusion of the AVM (D). (Courtesy of Dr. Konstantinos Roditis, vascular surgeon, Athens, Greece).
Laser therapy, a minimally invasive option for arteriovenous malformations (AVMs), has demonstrated promising results in recent studies. A literature review on laser therapy for AVMs emphasized its effectiveness in reducing AVM size and enhancing cosmetic outcomes. It is crucial to recognize that while laser therapy is beneficial, it is not the primary treatment choice for AVMs; typically, it is reserved for smaller AVMs situated in cosmetically sensitive areas (12). Embolization followed by laser therapy in treating an AVM has demonstrated effectiveness in addressing the AVM with a favorable cosmetic outcome, indicating the potential utility of laser therapy in managing such conditions (13).
Notable studies and reviews explore intervention strategies for extracranial AVMs, with a focus on outcomes and complications. A comprehensive review in Operative Neurosurgery specifically addresses temporalis muscle arteriovenous malformations (TM-AVMs), a variant of scalp AVMs. Analyzing seven TM-AVM cases, the review covers clinical, epidemiological, radiological, and therapeutic aspects. Findings indicate that TM-AVMs typically manifest as large masses in the temporal region, presenting various symptoms like pain and cutaneous stigmas. Treatment involves complete surgical removal, often preceded by preoperative embolization. Importantly, the review highlights that TM-AVMs, distinct from common scalp AVMs, should be recognized as a separate pathological entity due to their unique features, emphasizing the importance of accurate diagnosis and tailored treatment planning (14).
A significant review focused on interventional therapy for extracranial AVMs in the head and neck analyzed articles on treatments such as sclerotherapy and embolization. Covering studies published between 2000 and 2020, the systematic review assessed interventions and their outcomes. Emphasizing the role of angiographic imaging in diagnosis, the review included studies utilizing MRA, CTA, DSA, or fluoroscopic angiography. It explored various aspects of AVM management, including sclerotherapy and embolization, with or without surgical interventions. The review underscored the importance of comprehensive reporting of symptoms, location, and complications resulting from treatments (15).
4. Conclusions
The evolving landscape of managing temporal skin AVMs necessitates a collaborative, multidisciplinary approach, encompassing both lesion eradication and cosmetic considerations. Recent studies have unraveled genetic nuances, spotlighting potential therapeutic avenues for mutations like MAP2K1 (6). Epidemiological data offer valuable insights into the occurrence and demographic trends of extracranial vascular malformations, including AVMs. The impact of hormonal changes on AVM progression underscores the dynamic nature of these lesions (7, 8).
Diagnostic techniques, including MRA, CTA, and ultrasound, continue to progress, with high-resolution ultrasound demonstrating its utility in the early detection of vasculitic changes for effective intervention planning (10, 11). Treatment advancements, such as promising outcomes from endovascular approaches and the emergence of laser therapy for smaller AVMs, strike a balance between efficacy and cosmetic preservation (11-13). Systematic reviews emphasize the necessity for tailored interventions based on individual lesion characteristics and patient preferences (15).
Our review echoes the call for sustained research in temporal skin AVMs, emphasizing genetic exploration, diagnostic refinement, and innovative treatments to improve patient outcomes. Multidisciplinary collaboration involving genetics, radiology, dermatology, and vascular surgery is pivotal in advancing our understanding and approach to these lesions. Moving forward, the focus is not merely on innovation but on translating it into actionable strategies for enhancing patient care and outcomes in clinical practice.