1. Background
Cutaneous leishmaniasis (CL) is seen in two forms: the rural or wet (zoonotic) and the urban or dry (anthroponotic) forms. The main cause of urban leishmaniasis is Leishmania tropica (L. tropica) and the humankind is its main reservoir; however, dogs can also be infected with this parasite. The disease is transmitted by Phlebotomus sergenti, which is present in several cities of Iran such as Tehran, Kerman, Bam, Mashhad, Neishabour, and Sabzevar and recently in Rafsanjan and Khomeini-Shahr cities of Isfahan province (1-8). The incidence of leishmaniasis in Iran is estimated at 28 per 1000 population (9). Most of the cases were reported from Isfahan and Shiraz provinces, Iran and the lowest rate of infection was reported from Mazandaran province (10). Isfahan province is a CL endemic region, particularly the wet or rural type (zoonotic leishmaniasis or ZCL) (11, 12). Studies determined the type of leishmaniasis in Isfahan province as ZCL (13). Nadim and Seyedi Rashti showed that the main endemic regions of CL were the north, northeast and east of the Isfahan province (12). A study in 1991 in Borkhar, a city in Isfahan province, revealed a CL prevalence of 61.9% in the hyperendemic areas in Isfahan province and in 1995, the Leishmania major (L. major) was isolated from Phlebotomus papatasi (P. papatasi) in that city (10, 13). According to Yaghoobi et al. (11) study in four villages of Borkhar in north of Isfahan province, new cases of the disease were mostly found among people younger than ten years of age; in older ones, a prevalence of 11.9% was estimated with regard to the scar of lesion from which L. tropica was isolated (11). In addition, CL was reported in some parts of Ardestan, Natanz, Isfahan, Kashan, and parts of western and southern foothills of Isfahan province (14, 15). Regarding its complicated epidemiology, in addition to the location and presence of sand flies as vectors and the rodents as reservoirs, there are many other factors that contribute to disease transmission. These factors including agricultural projects, migration of the nonimmune individuals to the endemic areas, rapid and unplanned urbanization, and environmental changes such as irrigation, dam construction, and desertification, which all increase the risk of the diseases and its transmission (16, 17).
2. Objectives
A large number of patients from areas around the Isfahan province are referred to the governmental centers such as Skin Diseases and Leishmaniasis Research Center, which have equipped laboratories to diagnose and treat the leishmaniasis. The assessment of these patients not only shows the origin of disease but also reveals the old and new regions with high incidence of CL. In addition, the demographic features of the disease are important for researchers. Moreover, this information can be used to control the CL in Isfahan province. This study aimed to investigate CL epidemiology and its prevalence in Isfahan province, Iran.
3. Patients and Methods
In this cross-sectional study, all the recorded information was collected from patients with CL referred to the province Health Center from 2001 to 2011. The patients were diagnosed by direct microscopic examination of the samples in Skin Diseases and Leishmaniasis Research Center and other health care centers. Personal information, number as well as location of the lesions, duration of disease, area of residence, workplace and the history of travel during the past two months, address, and telephone number were recorded. The epidemiological status of leishmaniasis in Isfahan province was determined through the assessment of the recorded information. Data were analyzed using SPSS version 16 (SPSS Inc, Chicago, Il, USA). Descriptive findings were shown in graphs and tables. The Chisquare and ANOVA tests were employed to analyze the data.
4. Results
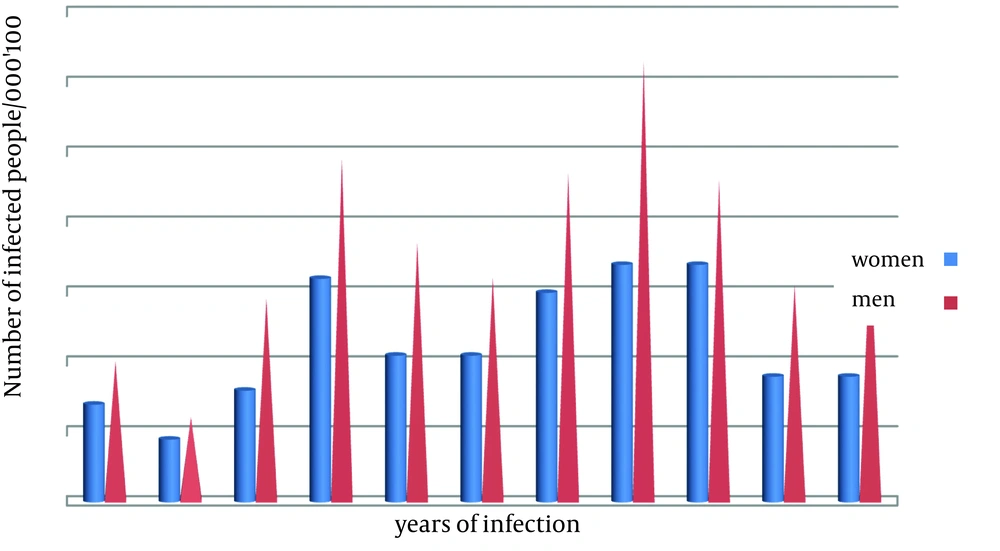
In the current study, the data of 28315 patients consisted of 10809 (38.2%) females and 17491 (6.8%) males with CL in Isfahan province from 2001 to 2011 were collected. The results showed a significant association between gender and leishmaniasis infection (P < 0.0001) (Figure 1). In addition, the mean age of patients was 22.40 ± 16.52 years (Table 1).
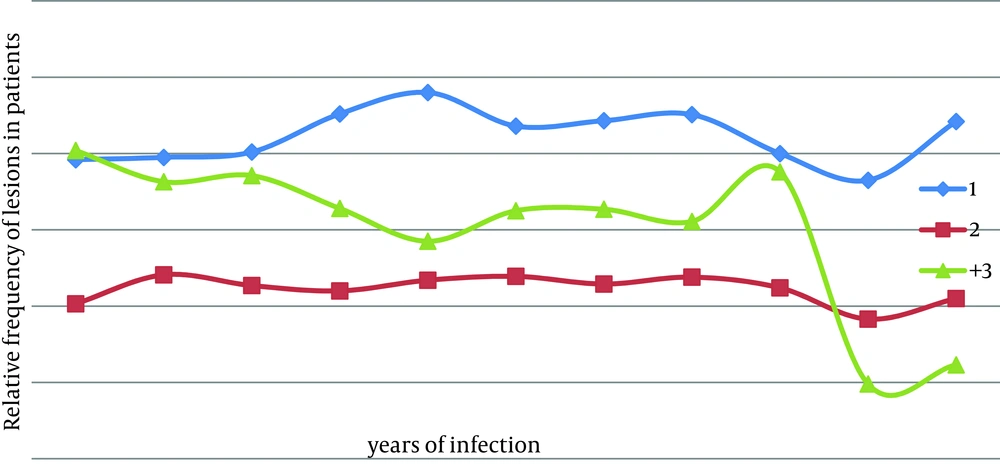
Based on the age groups, the highest prevalence rate was seen in the 10 to 20-year-old group (26.8%) and the lowest rate was observed among those older than 90 years of age. There was also a significant association between the prevalence of the disease and the age groups (P < 0.0001). The prevalence of disease among different age groups is shown in Table 1. As shown in Figure 1, hands (32.3%) had the highest rate of involvement and feet (11.5%) showed the lowest rate of involvement. There were one to three lesions on the patients’ trunk. In this study 12163 (43%) patients had one, 6330 (22.4%) had two, 503 (1.8%) patients had three, and 8008 (28.3%) patients had more than three lesions (Figure 2).
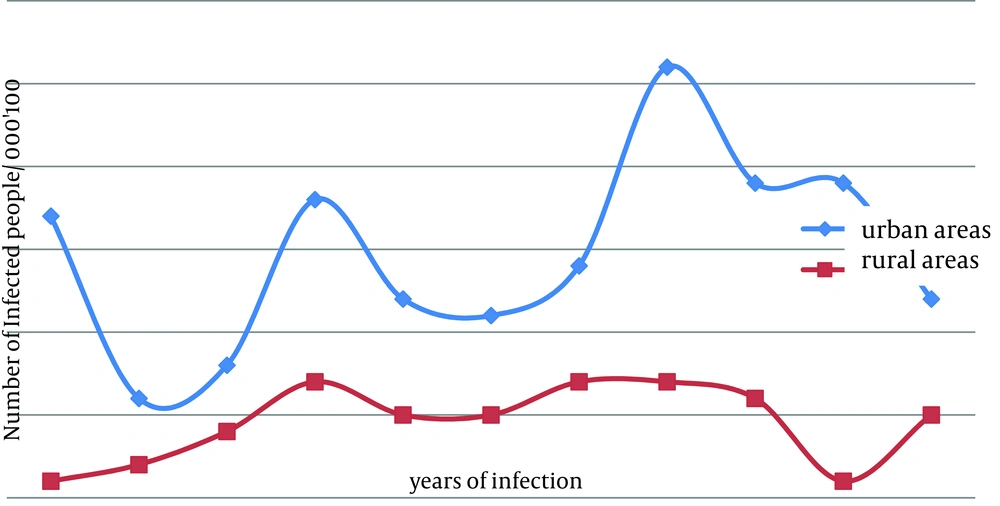
According to the results, urban areas had the highest rate of infection (63.2%) in comparison to the rural areas (29.1%). The prevalence of the disease in urban areas was two-times more than that of rural areas and a significant association was observed between the prevalence of the disease and residential area of the patients (P < 0.0001). Figure 3 illustrates the prevalence of CL in urban and rural population, in Isfahan province, Iran from 2001 to 2011. In the current study, the highest prevalence was seen in the patients who lived or had traveled to the endemic areas. In addition, 7.2% of patients with leishmaniasis came from nonendemic areas of the Isfahan province. The frequency of the disease among Iranian, Afghan, and patients from other nationalities was 92.5%, 7.4%, and 0.1%, respectively.
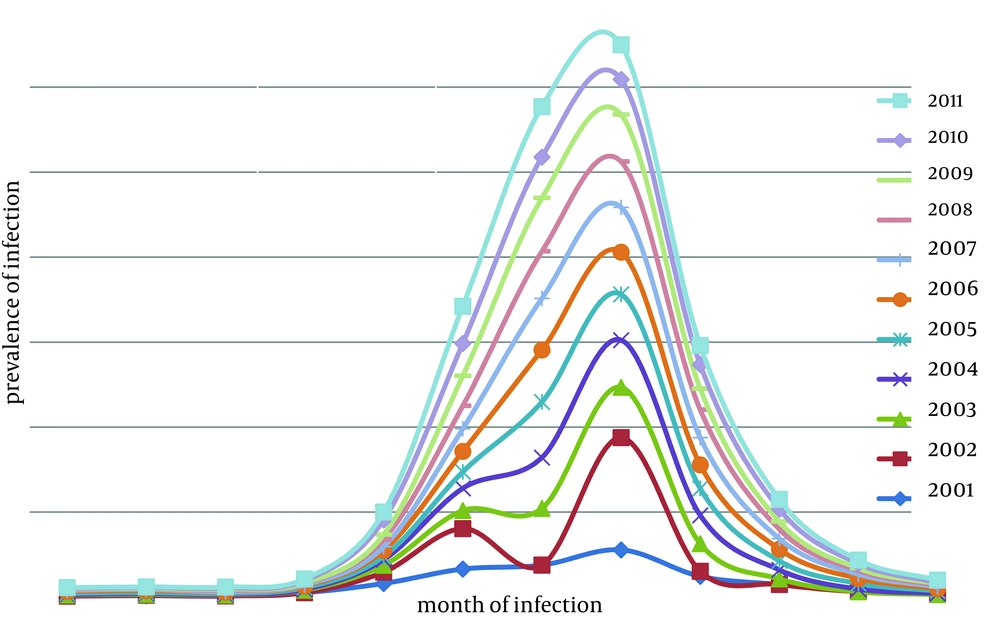
The results also indicated that the prevalence of the disease varied based on the months of the year. The prevalence of the disease was 28.3% in October and reached to its highest level of 28.3% in November, and then dropped to 4.1% in September. The highest prevalence was observed in Autumn since 70.1% of the infections occurred in this season.
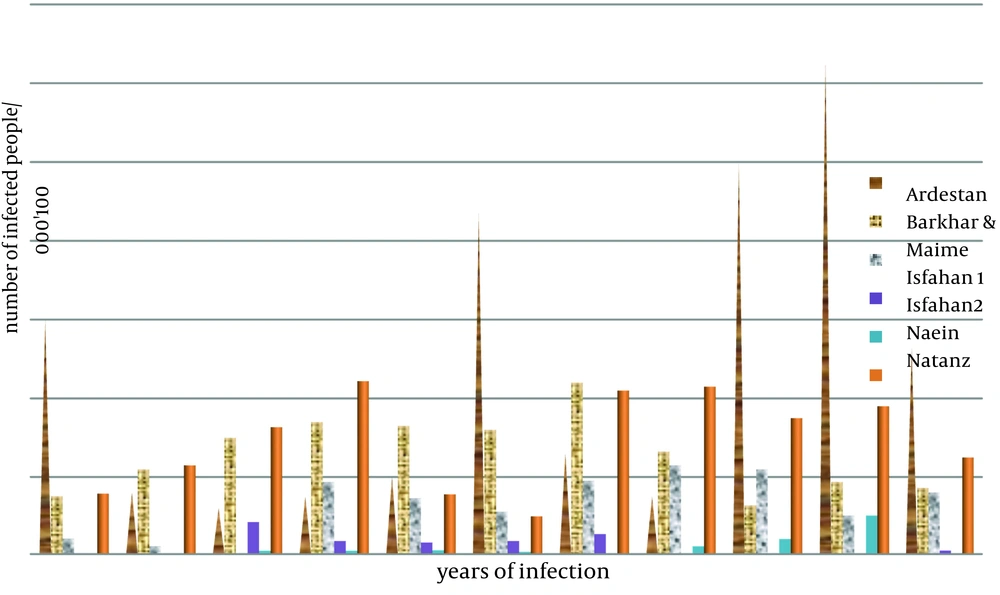
Statistical analysis showed a significant association between the prevalence of the disease and months of the year (P < 0.0001) (Figure 4). The highest rate of CL infections in Isfahan was in 2008, while the lowest rate was in 2002.
The prevalence of CL in endemic areas of Isfahan from 2001 to 2011 is presented in Figure 5. There was a reduction in the endemic areas in Isfahan in 2008 and 2011. The prevalence of CL in nonendemic areas of Isfahan province from 2001to 2011 is presented in Table 2. The results indicated that the prevalence of the disease in all nonendemic areas reached to 0.00 in 2007 (Table 3).
| Age Group, y | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-10 | 25.90 | 34.20 | 24.60 | 23.90 | 25.00 | 26.00 | 28.00 | 23.00 | 28.90 | 27.40 | 21.40 |
| 10-20 | 29.30 | 28.60 | 31.60 | 31.50 | 31.30 | 29.00 | 25.00 | 23.90 | 23.30 | 21.90 | 23.60 |
| 20-30 | 19.10 | 16.80 | 22.20 | 22.10 | 25.40 | 22.30 | 28.00 | 29.40 | 24.70 | 24.10 | 32.20 |
| 30-40 | 8.80 | 7.80 | 8.40 | 9.60 | 8.10 | 10.30 | 7.10 | 10.60 | 9.50 | 9.10 | 10.90 |
| 40-50 | 6.60 | 6.00 | 7.20 | 6.00 | 5.10 | 6.10 | 5.70 | 6.30 | 5.80 | 7.80 | 5.20 |
| 50-60 | 4.10 | 2.10 | 2.40 | 3.20 | 2.60 | 2.80 | 3.20 | 3.10 | 3.70 | 4.70 | 4.00 |
| 60-70 | 4.30 | 3.00 | 2.60 | 2.10 | 1.6 | 2.10 | 1.60 | 1.90 | 2.10 | 2.10 | 1.50 |
| 70-80 | 1.90 | 1.10 | 0.9 | 1.30 | 0.70 | 1 | 1.2 | 1.4 | 1.4 | 1.8 | 0.90 |
| 80-90 | - | 0.4 | 0.2 | 0.3 | 0.1 | 0.30 | 0.20 | 0.30 | 0.60 | 0.70 | 0.30 |
| 90-100 | - | - | - | 0 | 0 | 0 | - | 0.10 | 0.10 | 0 | - |
a Data are presented as No. (%).
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Face | 15.1 | 13.8 | 11.7 | 12.5 | 12 | 13.4 | 13 | 10.8 | 11.1 | 11.6 | 10.4 |
| Hands and feet | 1.9 | 1.3 | 1.1 | 1.4 | 1.3 | 1.6 | 1 | 1 | 1.7 | 0.9 | 1.6 |
| Hands and face | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.7 | 3.5 |
| Face, hands, and feet | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.4 | 1 |
| Feet | 22.9 | 23.6 | 27 | 25.1 | 24.7 | 23.2 | 24.6 | 24.4 | 22.6 | 19 | 27.2 |
| Hands | 30.6 | 30.6 | 35.1 | 32.4 | 34 | 33 | 31.7 | 34.7 | 32.2 | 25.9 | 31.2 |
| Hands and face | 5.7 | 5.8 | 4.1 | 4.4 | 4.2 | 4.9 | 4.1 | 4 | 5.5 | 4.3 | 0.1 |
| Hands, face, and feet | 0.5 | 3 | 1.2 | 1.5 | 1.5 | 1.5 | 2.1 | 1 | 1.9 | 0 | 0 |
| Hands and feet | 12.2 | 14.9 | 11.3 | 10.8 | 9.9 | 11.6 | 11.3 | 11 | 12.5 | 8.6 | 9.6 |
| Body | 11.1 | 7.2 | 8.5 | 11.8 | 12.2 | 10.7 | 12.2 | 13.1 | 12.4 | 7.9 | 14 |
a Data are presented as No. (%).
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tiran & Karvand | 8.8 | 11 | 17 | 22 | 11 | 0.58 | 0 | 23 | 22 | 5.8 | 20 |
| Khomeini-Shahr | 5.3 | 0.99 | 5.9 | 5.3 | 5.9 | 1.3 | 0 | 11 | 4.9 | 3.9 | 0 |
| Semirom | 0 | 0 | 0 | 0 | 0 | 4.2 | 0 | 0 | 5.6 | 2.8 | 4.2 |
| Falavarjan | 0 | 0 | 1.3 | 7 | 0 | 0.848 | 0 | 21.4 | 12 | 7.1 | 9.8 |
| Fereidan | 5.3 | 0.89 | 3.5 | 0.53 | 7.1 | 9.46 | 0 | 0 | 8.2 | 15 | 3.5 |
| Fereydon-shahr | 1.1 | 0 | 0 | 4.7 | 8.2 | 0 | 0 | 0 | 0 | 34 | 9.9 |
| Mobarake | 4.9 | 0 | 4.5 | 9.9 | 4.9 | 3.7 | 0 | 15 | 6 | 9.1 | 1.5 |
| Najaf abad | 1.74 | 4.5 | 0.33 | 8.3 | 7.5 | 4.3 | 0 | 11 | 7 | 6.3 | 3.6 |
| Shahreza | 5.6 | 0.99 | 0.49 | 0.33 | 5.9 | 1 | 0 | 29 | 24 | 12 | 19 |
| Golpayegan | 8.5 | 2.1 | 0 | 13 | 5.7 | 0 | 0 | 0 | 0 | 4.9 | 7.4 |
| Dahaghan | 0 | 0 | 0 | 0 | 0 | 11.1 | 0 | 11 | 0 | 13 | 16 |
| Chadegan | 0 | 0 | 0 | 2.7 | 2.7 | 0 | 0 | 2.8 | 11 | 5.6 | 0 |
| Lenjan | 6.6 | 1.6 | 3.7 | 5.6 | 2.8 | 12.8 | 0 | 21.5 | 10 | 5.8 | 10 |
| Shahin shahr | 0 | 0 | 0 | 9.5 | 0 | 0 | 0 | 0 | 0 | 25 | 15 |
| Khansar | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 3 |
a Data shows the prevalence of infection in 100000 people in each region.
5. Discussion
The results of the current study showed that the incidence of infection in men was two times higher than that of women (61.8% in men and 38.2% in women) that may be due to the large number of men who work as seasonal migrant workers, work in open areas, wear less dresses than women do, have more passing through abandoned and dessert areas, and hence, have more contact with sandflies. Therefore, it is better to prevent contact with sandflies, avoid sleeping outdoors, and inform people who want to travel or migrate seasonally to the endemic areas about the potential risk of leishmaniasis and its consequences (18-20). In the current study, all the patients with leishmaniasis had a history of travelling to one of the endemic areas in Isfahan province or other leishmaniasis foci of Iran (drivers, seasonal workers, armed forces, and passengers). In the previous studies, the phenomenon of migration to the endemic areas has been mentioned as one of the factors leading to an increase of infection prevalence (21-23).
The results of the current study showed that there was an infection rate of 26.8% among those aged ten to twenty years from who the highest rate belonged to the people who lived in the endemic areas; moreover, most of them were physically active and had rarely left the area. The reason of high rate of infection with Leishmania species is the lack of knowledge about the ways of transmission to the patients. Generally, the prevalence of leishmaniasis in endemic areas increases in those younger than 15 years old thereafter, decreases probably as the result of acquired immunity. Based on the relevant studies, the highest rate of leishmaniasis prevalence was reported in those younger than 14 years of age, which is compatible with the results of the current study that introduced Isfahan province as an endemic region (22, 24). According to the results of the current study, the lesions were most frequently located on hands (32.3%) and feet (24.1%) of the patients, which are similar to those reported by Nazari (23). Considering the shortness of mouth appendages of sandflies and their inability to suck blood from the covered parts of the human body, the possibility of biting uncovered regions by sandflies was higher than the covered ones hence, the leishmaniasis lesions mostly occur in uncovered regions. Moreover, chemical and fragrance attractions such as the concentration of carbon dioxide, which usually occur in hands and feet more than the other parts, help sandflies to find their proper host. Studies conducted in Ardakan, south of Lorestan province, Damghan, and Mirjaveh, Iran, and the studies in Saudi Arabia confirmed the maximum occurrence of lesions in uncovered regions of the body (22-31). The results of the current study showed that the number of lesions in patients with leishmaniasis is varying between one and three (28.3%) which are not similar to those of the previous studies. The results of Rafati et al., Athari and Jalallu, Babaei, Mesgarian et al., Doroudgar et al., Hamzavi et al. and Dehghani et al. were also in agreement with the current study (20, 22-24, 28, 31).
The results of the current study showed that the highest prevalence of the leishmanias is occurred in the urban areas (63.2%), which indicated that people have travelled from urban areas to the endemic areas and people in rural areas were infected during childhood and would have acquired immunity in their adolescence. In the current study, the highest and lowest rates of leishmaniasis were reported in autumn and spring, respectively, which were similar to the reports of the previous studies. The results of a previous study showed that the highest incidence rate of seasonal leishmaniasis in Ahvaz, Iran, was in autumn in (49.2%) and the lowest rate was in spring (9%) (32). A study in Saudi Arabia reported a seasonal variation of infection with Leishmania species with the highest incidence during June to November (30). In a study performed in Ardestan, Iran, the highest rate of infection was reported during April to October (31). In another research in Moltan, Pakistan, all cases were reported during winter (33).
Considering the data provided by health care centers of the endemic provinces and regions of Iran from 2001 to 2011, four operational phases for controlling and fighting leishmaniasis were performed. Killing the rodents were done in all endemic areas (including Isfahan 1, Isfahan 2, Ardestan, Natanz, Bourkhar, Shahin-shahr, and Maimeh) through decoying with zinc phosphate, chlorate poisons or phostoxin tablets, nest destruction, and foul-up; these interventions resulted to an decreased leishmaniasis incidence in these areas in 2008. In addition, evaluation of nonendemic areas of Isfahan in 2007 showed that the prevalence of this infection reached zero that was probably due to the mentioned policies; in the endemic areas of the province, this disease has been eliminated too. Leishmaniasis, which is one of the main diseases transmitted by sandflies, is highly important because of its vast distribution in different regions of the country and should be eliminated anywhere detected, especially in Isfahan province with the high prevalence. Garbage should be collected precisely and animal reservoirs should be identified and properly eliminated through appropriate methods. Residential areas of sandflies should be identified and sprayed with insecticides. The ways of transmission and also leishmaniasis prevention methods should be trained.