1. Background
Keloids are fibroproliferative disorders seen only in human following trauma, inflammation, and surgery as well as spontaneous conditions, due to collagen accumulation in dermis and hypodermis (1). Even ear piercing, abrasion, tattoos, and more importantly, burns could make keloids emerge (2). Radiotherapy, laser therapy, and administration of interferon, bleomycine, and triamcinolone are well-known preventive techniques (3-6). Among which triamcinolone acetonide, the most suitable corticosteroid, is widely used as 10 - 40 mg/mL intralesional injections, which blocks inflammatory cell rush at the site. In addition, it stops fibroblast proliferation. Calcium channel blockers are known as compounds which stimulate procollagenase production, especially when injected into keloids and hypertrophic scars. This would result in actin filament depolarization and fibrosis inhibition in damaged tissues. High cost, low efficacy, and higher rates of recurrence as well as cancerogenic features have disregarded non-medical treatments including surgery, laser, radiotherapy, and gel sheeting for managing keloids and hypertrophic scars. Medical therapy has a likely low response (tacrolimus), high cost (bleomycine and/or interferon), high recurrence rate (5-flouracil) as well as unpleasant adverse effects (7, 8). Verapamil is reclaimed to inhibit the production of IL-6 and Vascular Endothelial Growth Factor (VEGF) in keloid fibroblast cell culture. A hypothesis has recently shaped expressing that high production of cytokines and growth factors play a prominent role in fibroblast proliferation, especially in a layered structure tissue secreting IL-6 and VEGF (9, 10). Decreased IL-6 and VEGF production was observed after 100 µmol verapamil administration on a fibroblast cell culture through 72 hours. This calcium antagonist compound can lessen cell proliferation by 29%, while increasing apoptosis rate by 8% of verapamil, a calcium channel blocker with almost acceptable adverse effects with or without cryotherapy, as an alternative medication for intralesional injection of triamcinolone acetonide with cryotherapy and cryotherapy alone (11).
2. Objectives
The aim of this study was to compare the efficacy and safety of “Intralesional triamcinolone with cryotherapy” and “Intralesional verapamil with cryotherapy” in the treatment of keloid.
3. Patients and Methods
Between March 2008 and August 2012, 105 patients with keloids referred to skin research center in Shahid Beheshti University of Medical Sciences, Tehran, Iran were recruited. Patients aged 10 - 50 years with keloids smaller than 10 cm2 in area who had received no treatments in the past six months were included. All pregnant or breast feeding patients as well as those with diabetes mellitus, cancers and cardiovascular diseases were excluded. Hypertrophic scars or post acne scar were also excluded.
Independent from the severity and chronicity of lesions, patients were randomly divided into four groups of intervention. Demographics in addition to symptoms and signs, clinical aspects of lesions and the size of scars were recorded using a questionnaire. In the case of multiple keloids, the most accessible one with a defined size preferred by the patient was considered for the treatment.
The Vancouver Score Scale (VSS), an international evaluation means to survey keloid scars, was used in the current performance. Thickness, pliability, vascularity and pigmentation are the four zones of checking in this scale. The Centimeter Scale was the other used means to report keloid size.
All participants underwent regular visits after therapy every three weeks to evaluate the treatment progress. The process was performed until the scar became flat unless having no response after six months, leading to treatment discontinuation and considering the patient as non-response case. The participants were followed up for a year to evaluate disease improvement and adverse effects or recurrence in any case. Clinical photography was performed at each session with a digital 14 mpc camera (Samsung, Korea).
3.1. Intervention Groups
At first, four groups of intervention were defined to randomly allocate participants to choose the selected drug and methods before comparing them. Group one: patients received cryotherapy with intralesional injection of triamcinolone acetonide. Group two: patients were treated with cryotherapy in addition to intralesional injection of verapamil. Group three: patients merely received intralesional verapamil (without cryotherapy). Group four: patients only underwent cryotherapy.
Cryotherapy was performed using nitrogen spray two times in 15 seconds interval 5 minutes before medication injection in group one and group two and without injection in group four. Spray covered the keloid with a 1 mm extra margin. In group 1, triamcinolone acetonide 40 mg/mL suspension (Kenacort A®) was diluted with lidocaine hydrochloride 2% to achieve a dose of 20 mg/mL. In groups 2 and 3, verapamil 5 mg/2 mL (Lekoptin®) was diluted in the same way to half of the concentration. Cryotherapy was performed five minutes before drug injection in groups 1 and 2 as previously described.
Two research-blinded dermatologists evaluated keloids to diagnose and measure response rate and adverse effects as well as to identify those who needed to be excluded. Keloids were classified as mild (0 - 4 scores), moderate (5 - 8 scores) and severe (9 - 13 scores) considering VSS and improvement was reported as cure, partial treatment and no response to treatment based on the same criteria Concerning outcome measures, lesions with > 8 VSS needed to achieve VSS score < 4 to be reported as complete cure.
3.2. Statistics
This trial benefited 95% confidence interval as well as type 1 error of 0.05. Chi-square test was performed to compare results between the groups. One way ANOVA was professionally used to find any differences between the techniques used in interventional groups.
3.3. Ethics
A written consent was taken after relevant explanation to participants about the aims and process of study. No extraordinary facilities or expenditures were directed to people based on accepting or declining to participate in the trial. In any part of the study, participants could request to leave the study without any limitation or prerequisite. Besides, all patients’ information were saved carefully to provide suitable privacy for recruited participants.
4. Results
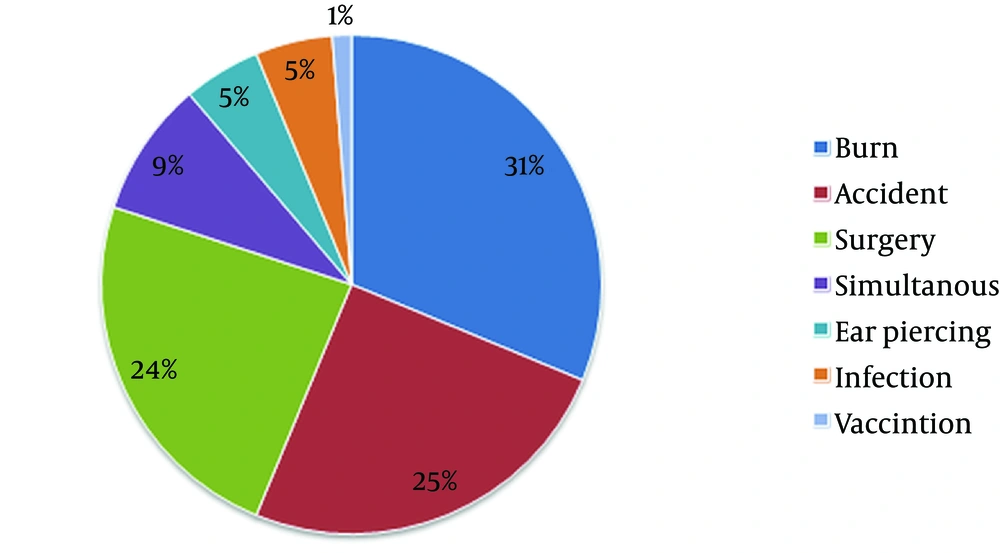
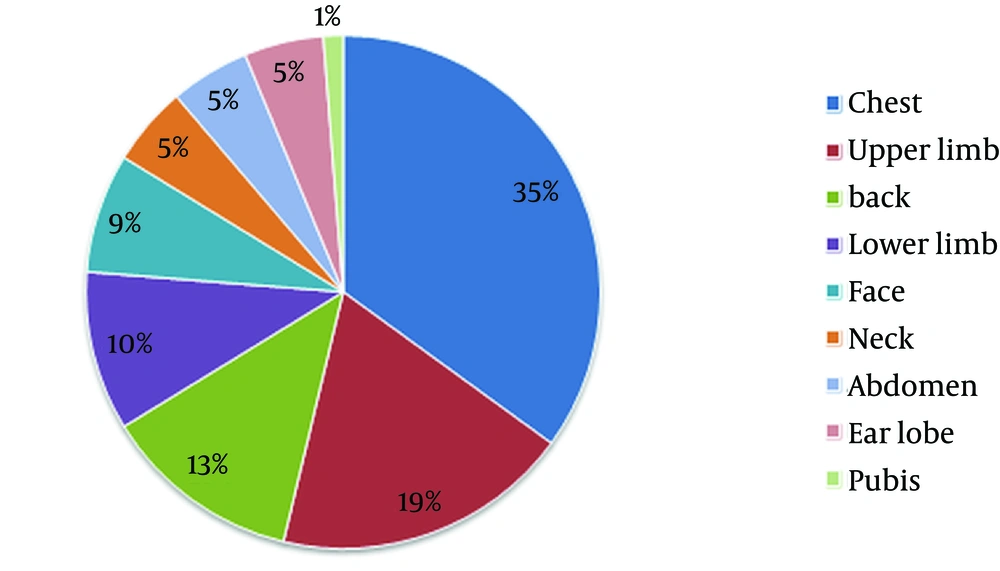
A total of 105 patients with keloid were recruited and randomly classified into four treatment groups. Based on the exclusion criteria, 25 patients were excluded and the remaining 80 patients, classified in groups of 20, were treated with one of the four therapeutic approaches. Overall, 38 (47.5%) and 42 (52.5%) of patients were male and female, respectively. The mean age of participants was 24.25 years containing three age groups as demonstrated in Table 1. With respect to skin type, two types of Fitzpatrick classes including III and IV were identified in 72 (90%) and 8 (10%) patients, respectively. A positive family history was observed in 12 (15%) of patients. Regarding Figures 1 and 2, the main cause of keloid and anatomical locations were evaluated and reported. As depicted in the first pie chart, burn was the most common causative factor with 31.25% rate followed by accident and surgery. The most prone part of the body to keloid formation was the chest (35%) with a significant difference (P value = 0.034). A prominent portion of participants reported itching (40%) followed by tenderness in 17.5%. In terms of size, the biggest diameter of lesions was 6 - 10 cm (mean = 5.27), while 5 - 15 mm for width (mean = 6.56). Of 80 patients, 60 patients (75%) had lesions with a diameter more than 2 mm (mean = 1.7). In average, participants had experienced keloid for 2.18 years among whom 50% had been involved for less than two years.
| Variables | Values |
|---|---|
| Age Categorization | |
| 11 - 20 | 24 (30) |
| 21 - 30 | 44 (55) |
| 31 - 40 | 12 (15) |
| Gender | |
| Male | 38 (47.5) |
| Female | 42 (52.5) |
| Fitzpatrick Skin Type | |
| III | 72 (90) |
| IV | 8 (10) |
| Family History | |
| Positive | 12 (15) |
| negative | 68 (85) |
a Data are presented as No.(%).
When VSS characteristics were concerned, the most pliability found was yielding (40%), while 49% showed redness and 46.25% had a complex of hypo and hyperpigmentation. VSS revealed that 57.5% of scars were moderately involved.
4.1. Treatment Outcomes in Interventional Groups
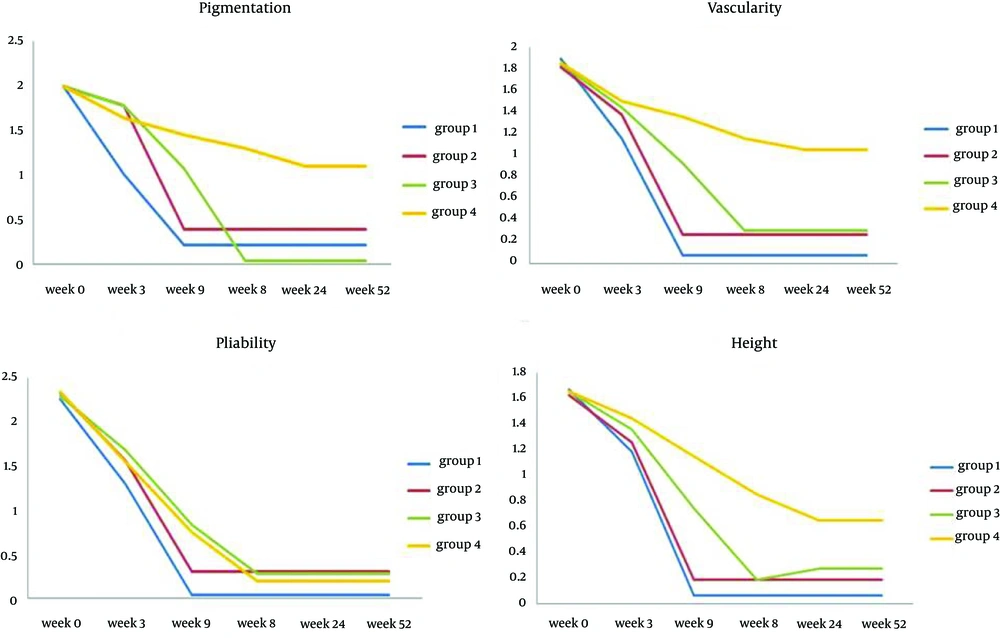
Figures 3 and 4 show treatment progress in four groups reporting the trend of VSS for each group.
4.1.1. Group 1
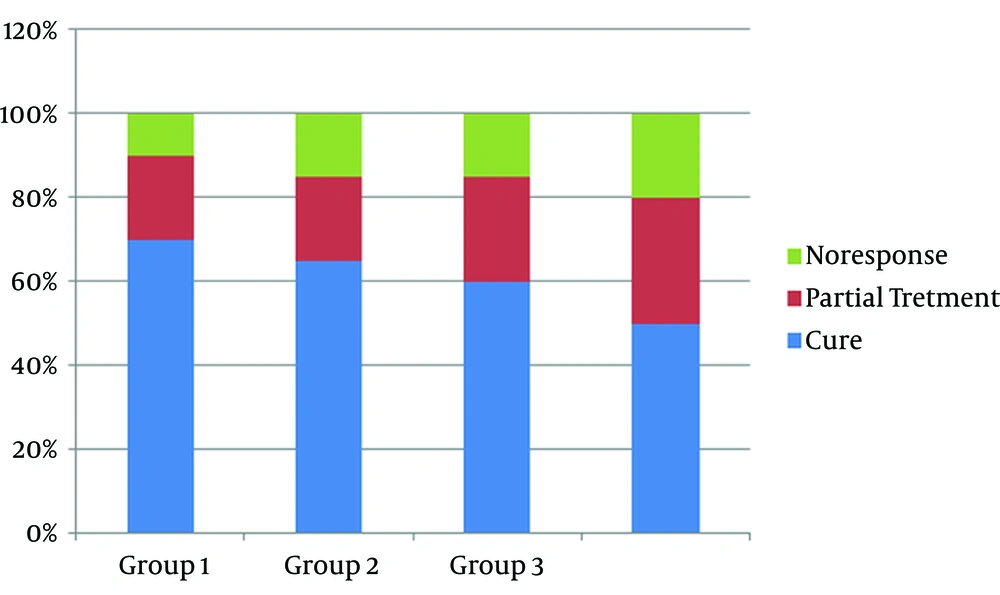
The mean time to treat keloids was 6 weeks among 20 patients who experienced cryotherapy plus intralesional triamcinolone acetonide. Total complete cure rate was 70%, while 2 (10%) had no improvement.
4.1.2. Group 2
Of 20 participants in this group (Intralesional verapamil plus cryotherapy), 13 patients (65%) showed completely flattened lesions, but 3 participants (15%) had no response to treatment. There was no significant difference compared to group one after a mean time of 9 weeks treatment. (P value = 0.13). Similar to group 1, this group showed significant improvement in all studied variables (P value < 0.001).
4.1.3. Group 3
This group did not receive cryotherapy as indicated in the method’s section (intralesional verapamil). The mean treatment period was 12 weeks. Overall, 60% (12 patients) complete cure rate was observed and 15% (3 patients) had no response to treatment. In treated patients, a significant improvement in all lesion characteristics was found as well (P < 0.001).
4.1.4. Group 4
During an average period of 24 weeks, 20% (4 patients) failed to be treated only with cryotherapy, although significant decreases in VSS and size were absolutely reported in responsive cases (P < 0.001).
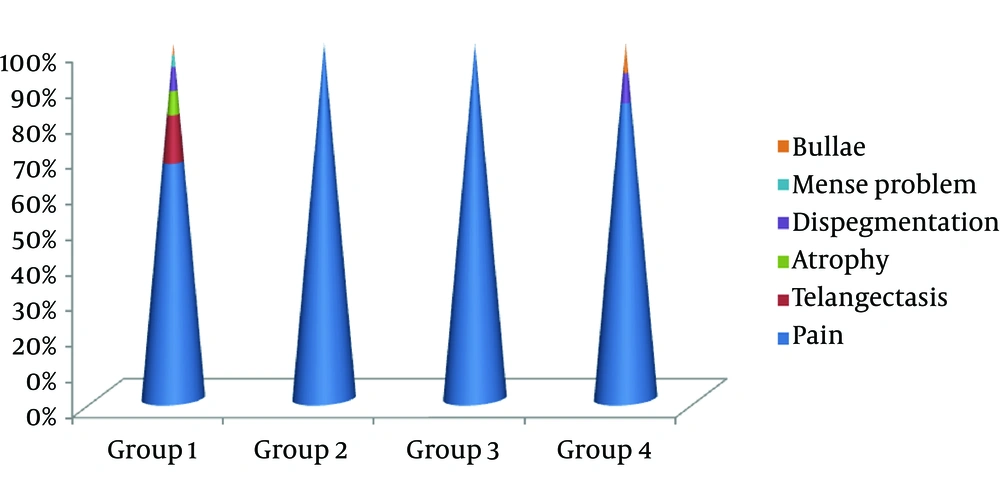
Comparing different therapeutic approaches, this trial found a real faster response in the first group; while groups 3 and 4 had the slowest responses to treatment. Rates of responsiveness seemed to have no significant difference between the groups, but adverse effects were significantly much frequent in the first group. Pain at injection and cryotherapy site was the most frequent complaint in all participants (100%) followed by telangiectasia (20%) in group 1. Other adverse effects are presented in Figure 5. In group 2, those who treated with intralesional verapamil and cryotherapy experienced significantly less adverse effects, regardless of pain, in an acceptable period of therapy (P = 0.046) compared to triamcinolone and cryotherapy receivers.
5. Discussion
The current trial revealed faster treatment of keloid with more adverse effects in combined cryotherapy-intralesional triamcinolone acetonide therapy. Compared to Intralesional verapamil plus cryotherapy, patients only experienced pain at the injection site with only 3 weeks extra time required to get 5% less treatment rate, which might be acceptable. Groups 3 and 4 had the slowest responses to treatment, although pain was the only adverse effect observed in groups 3 and 4 which was similar to groups 1 and 2.
Verapamil is mainly concerned in three mechanisms for keloid treatment. This calcium antagonist, like triamcinolone, has an inhibitory effect on cell proliferation which is a known prevention pathway for fibrosis formation, but less effective than the former drug. In this regard, verapamil has similarities with interferon-alpha-2b (IFN-α-2b), which directs the prohibition by increased expression of TGF-β1 (12). The latter factor has no similar induced apoptosis effect which both triamcinolone and verapamil present as another pathway to prevent collagen accumulation as seen in keloid and hypertrophic scar. Another mechanism involved in verapamil action as a calcium channel blocker is due to strong stimulation of pro-collagenase synthesis in tissues, consequently making it a suitable alternative for triamcinolone (8). This makes verapamil and other calcium channel blockers effective blockers of the secretion of extracellular matrix molecules such as collagen, fibronectin and glycosaminoglycans (13, 14). Cellular secretion of the mentioned macromolecules is mainly a calcium-dependent process perfectly inhibited by calcium antagonists like verapamil and nifedipin (14).
Song et al. conducted an experimental study to compare fibroblast characteristics of normal and keloid tissues to indicate that keloid fibroblasts have real drug resistance when treated with vincristine and mitoxantrone compared to normal fibroblasts. Fibroblasts in keloid tissue revealed greater expression of membrane transporters as the main causes of increased resistance to chemotherapy agents and post therapy recurrence in keloids. Interestingly, researchers expressed that this resistance could be largely abrogated by verapamil treatment (15).
Globally approved evidence supports different methods from silicone sheeting to corticosteroid injections and pressure dressing as the first line treatment for keloids, while cryotherapy should be used in smaller lesions. Although fast to respond, surgery is mostly disregarded due to high postoperation recurrence rate unless combined with pulsed dye laser, radiation and imiquimod cream (16).
In line with the current trial, Xu et al. concluded similar benefits of intralesional injection of steroids, IFN-α2b and verapamil in keloid and hypertrophic scar; although the underlying mechanisms are different (12). Margaret Shanthi and colleagues introduced a study with two groups of intervention trying to compare intralesional injection of triamcinolone and verapamil in 54 patients with keloid. Similar to the present study, the two evaluation systems including the VSS and the Centimeter scale were used. Except scar pigmentation and length, clinical characteristics were absolutely improved using both drugs for three weeks and changes seemed to be faster with triamcinolone although higher drug reactions reported as well (8). In our study, despite using combined cryotherapy in the both groups, significant improvements in all VSS and centimeter items during 6 and 9 weeks of treatment with triamcinolone and verapamil, respectively were observed.
Through an 18-month follow-up, D’Andrea et al. compared the effects of intralesional verapamil hydrochloride in two groups after perilesional surgical excision of keloids and found 54% success rate in combined therapy with surgery, topical silicone and verapamil, but 18% in surgery in addition to topical silicone without verapamil (17). Recently, Ahuja et al. compared the effect of Triamcinolone (T) and verapamil injections for treatment of keloid. They reported that verapamil is the best choice for flattening the raised scars (7). Likewise, Lawrence showed that using intralesional verapamil hydrochloride after earlobe surgical keloid excision revealed a 52% cure rate in 35 African-American patients (18).
In conclusion, combination therapies in keloid lesions are better than single agent therapy preferably with intralesional injection of steroids or calcium antagonists as adjuvant treatments. In this regard, verapamil with lower drug reactions and adverse effects seems to be a suitable alternative for triamcinolone despite a slightly slower effect.
5.1. Study Limitations
The main challenge through the study was undisciplined follow-up visits, which was solved by explaining the importance of physician visits to participants.