1. Introduction
Juvenile xanthogranuloma (JXG) is a non-Langerhans-cell histiocytic proliferative disorder that is seen throughout the first two decades of life (1, 2). It is a relatively rare benign fibrohistiocytic lesion. The mean age of manifestation is three years (median, one year old) with a predominant male involvement. It is characterized by one or more cutaneous nodules and is less often seen in deeper soft tissue or internal organs. The most common sites are the head, neck and trunk, but it can develop anywhere in the body including groin, scrotum, penis, clitoris, eyelids, toenails and lips (3). In the recent years, numerous clinical forms of JXG beyond this classic description have been reported. In such cases, making the diagnosis may be difficult without knowledge of the different clinical variants. The JXG can be easily recognized when it presents the common yellow cutaneous nodule, yet it may not be suspected in atypical variants. Correct diagnosis is essential and has the big advantage of avoiding unnecessary invasive procedures and treatments.
The eye, especially the iris, is a common site of extracutaneous involvement, yet it can also develop in bones (Erdheim-Chester disease), lungs and liver (4-6). Herein we reported on a 14-year-old boy who presented JXG localized on the left palm. We described a case of JXG with a rather unusual clinical presentation on an uncommon involvement site, and highlighted the importance of considering this entity in the differential diagnosis of benign soft tissue tumors of the palms.
2. Case presentation
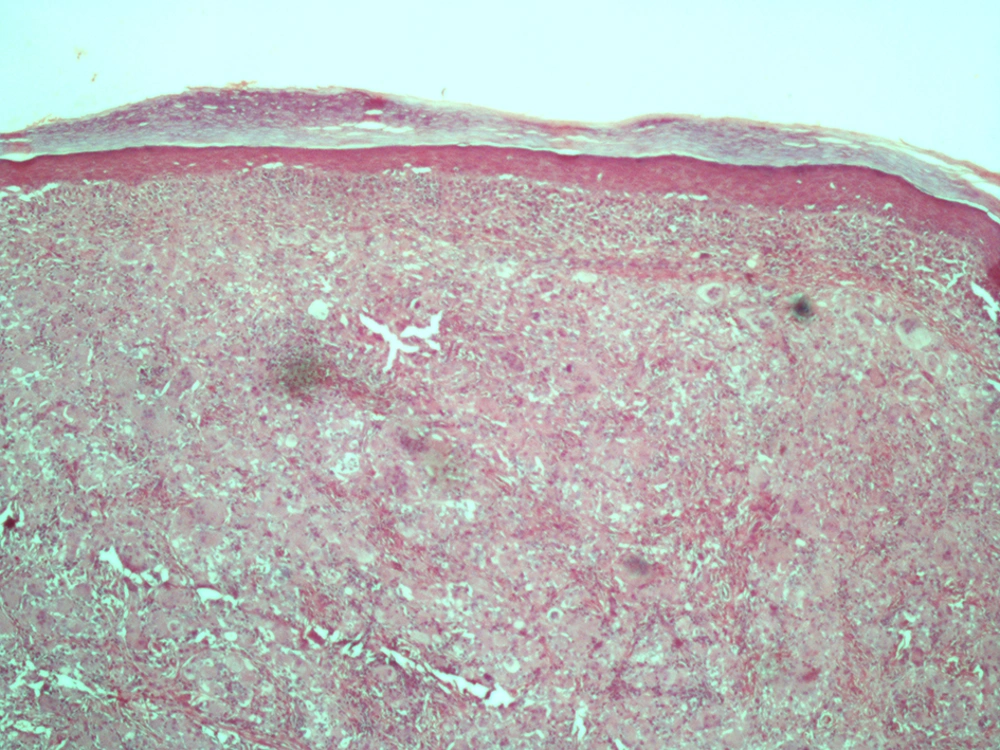
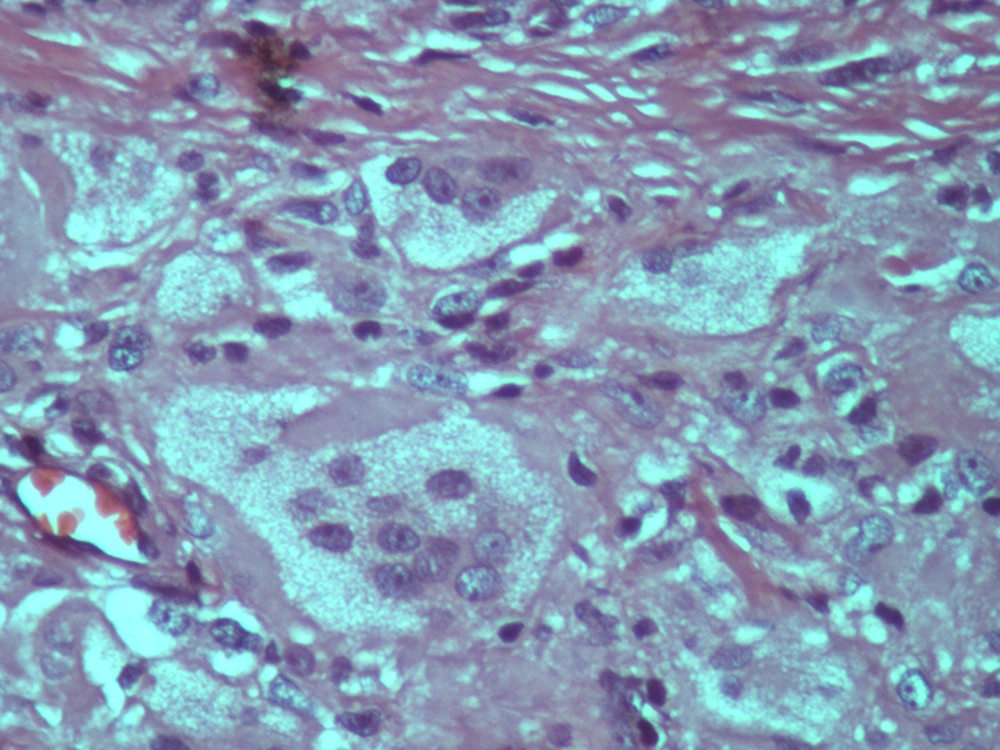
The case was a 14-year-old boy who presented a nodular lesion on the mid part of his left palm. The lesion had appeared two years ago, yet it had rapidly enlarged during the preceding two months. He had no history of any trauma or bleeding, but the nodule was painful. On physical examination, the lesion was circumscribed, firm, immobile, brown papule and 4-mm in diameter (Figure 1). It was shiny and on palpation, it was firm and without tenderness. Family history was insignificant. Findings of the radiographic and laboratory tests such as blood cell count and liver profile were normal. Excisional biopsy was performed to make the diagnosis. The patient underwent surgery under local anesthesia. The lesion was excised completely with the elliptical technique. Differential diagnosis included xanthoma, neurofibroma, spiradenoma, and leiomyoma. Histopathologic examination with hematoxylin and eosin staining was used to confirm diagnosis. The epidermis was normal. Histopathologic examination revealed a dermis expanded by predominantly multinucleated giant cells. Some of these cells contained foamy cytoplasm. An infiltrate of lymphocyte was also present throughout the lesion. A dense infiltrate of polygonal to spindle-shaped fibroblasts mixed with numerous foamy histiocytes within the dermis (Figure 2), and variable numbers of touton cells with vacuolated cytoplasm were present, which were characteristic of JXG (Figure 3).
In immunohistochemical analysis, the lesional cells were positive for CD68 and factor XIIIa, yet negative for S100, CD1a, and Langerin. These histopathologic and immunohistochemical findings confirmed the diagnosis of JXG. During the one-year follow-up, no recurrence or complication was seen.
3. Discussion
The JXG is a cutaneous fibrohistiocytic lesion, which was first reported by Adamson in 1905. It was defined as single or multiple cutaneous nodules. In 1912, McDonough proposed that this disorder might be derived from endothelial cells (7). Although the most common presentation is a solitary cutaneous lesion (1), it can manifest as a multisystem disease (6). It is usually seen in young children and the medium age of onset is two years; however, lesions may be present at birth. In our case, it presented on the second decade of life, which has been rarely reported by previous studies.
Another unusual finding in our case was the site of the lesion. Most lesions in JXG develop on the head and neck, while palms are not common sites for JXG. This disorder is more prevalent in males than females, especially in young infants. It can be seen in association with neurofibromatosis type 1 and juvenile chronic myelogenous leukemia (3). Ocular JXG mostly occurs in very young children without concomitant skin involvement (8). The JXG can be differentiated from other skin tumors such as poroma, molluscum contagiosum, neuroma and neurofibroma by history and histopathologic examination. Histopathologic examination is used to diagnose non-Langerhans histiocytosis, yet cannot help differentiate subtypes; therefore, immunohistochemical examination is essential and CD68 is its specific marker (9).
It is usually self-limited and often undergoes spontaneous regression (1, 5, 6). The pathogenesis is unknown, and initial triggers may be infections or physical factors such as trauma (10, 11). Despite the likelihood of spontaneous regression, it is best to excise the lesions for diagnostic reasons. Excision is enough and recurrence is uncommon (12).
It is recommended to excise any soft tissue masses for histochemical examination in children in whom a malignancy cannot be excluded by history.