1. Background
For most individuals, the first signs of aging are noted around the eyes. Due to the complexity of periorbital anatomy and the consequent aging process, which includes volume loss, skin laxity, and tissue descent, a variety of surgical and non-surgical methods can be combined to rejuvenate the periorbita (1). Surgical blepharoplasty has traditionally been used to rejuvenate the upper and lower eyelids by removing excess and lax soft tissue that has descended with aging (1). Overall, blepharoplasty has a low complication rate and is well tolerated by most patients; however, it does not address the issue of volume loss. It is important to find the best strategy to maximize the rejuvenation effect while minimizing complications. In-depth discussions with the patient to determine goals, risk factors, and alternatives are required to decide on the best combination of modalities.
A variety of modalities have been used with blepharoplasty to enhance the aesthetic rejuvenation of the periorbita. Botulinum toxin, hyaluronic acid fillers, and platelet-rich plasma (PRP) have all been used. Botulinum toxin can be costly and is required frequently. Hyaluronic acid fillers carry an increased risk of vessel occlusion, prolonged edema, scarring of the lymphatics of the periorbita, and discoloration around the eyes. PRP also requires more than one treatment and provides short-term results. In the last 10 years, advances in fat grafting have made autologous fat a very reasonable option to combine with surgical blepharoplasty (2). Recently, Marten and Elyassnia (2) reviewed the role of fat grafting in surgical procedures to rejuvenate the periorbital area by treating the problem of volume loss. Most agree that fat grafting provides a more youthful and natural aesthetic appearance than blepharoplasty alone. The shift from macrofat of the past to microfat has allowed for more preservation of the stem cell component, providing both a regenerative therapy and an aesthetic effect. Nanofat has transformed into "lipofilling" with very small fat particles and a high concentration of growth factors and stem cells, making the fat highly regenerative. This is relevant to understanding the potential impact of adipose tissue adjunct to an already well-standardized intervention. Nanofat addresses volume loss and revitalizes tissues of the periorbita affected by aging (3, 4). Fat grafting also has the advantage of providing longer-lasting results compared to other modalities. However, fat grafting does require an additional harvest site, thus an additional procedure, raising concerns about creating undue burden on the patient and the postoperative course.This retrospective study aimed to investigate the short-term postoperative effects of lipofilling in combination with blepharoplasty for patients undergoing periorbital rejuvenation by an experienced plastic surgeon in a private practice setting.
2. Objectives
This retrospective study was aimed to investigate the short term post operative effects of lipofilling in combination with blepharoplasty for patients undergoing periorbita rejuvenation by an experienced plastic surgeon in a private practice setting.
3. Methods
3.1. Study Design
This retrospective study analyzes the short-term postoperative period of patients undergoing surgical blepharoplasty alone (Group 1) or blepharoplasty combined with lipofilling (Group 2) from 2002 to 2021.
3.2. Participants
Patients for the study were recruited from a private practice setting. All patients signed written informed consent forms for the procedures and photography.
3.3. Procedures
All procedures were performed by a single plastic surgeon. Meticulous marking was done while the patient was standing to preserve landmarks once the patient was supine and local anesthesia was infiltrated. Intravenous sedation was administered using Midazolam (2 mg), Fentanyl (50 - 100 micrograms), and Propofol (in small boluses). Additional local anesthesia was provided using 2% Mepivacaine with epinephrine for eyelids and infraorbital nerve blocks. Oxygen flow was supplied during the procedure to assist with the patient's spontaneous breathing. Amoxicillin-clavulanic acid was used intraoperatively for prophylaxis and postoperatively.
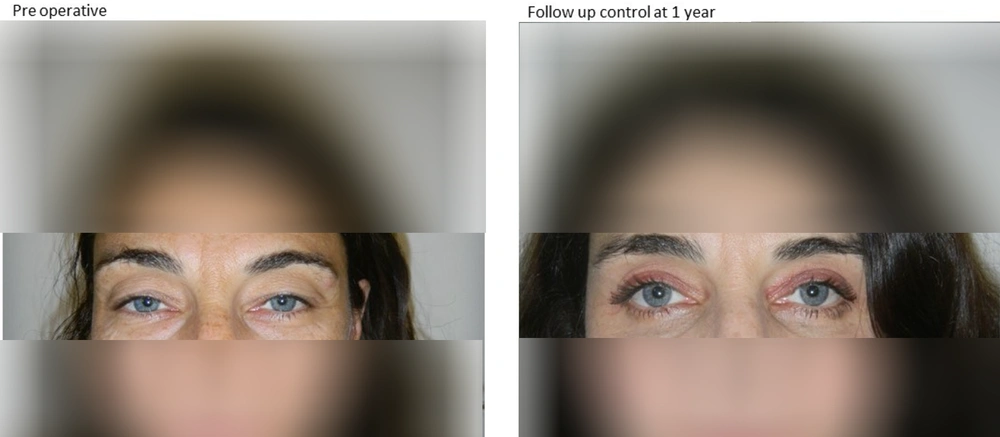
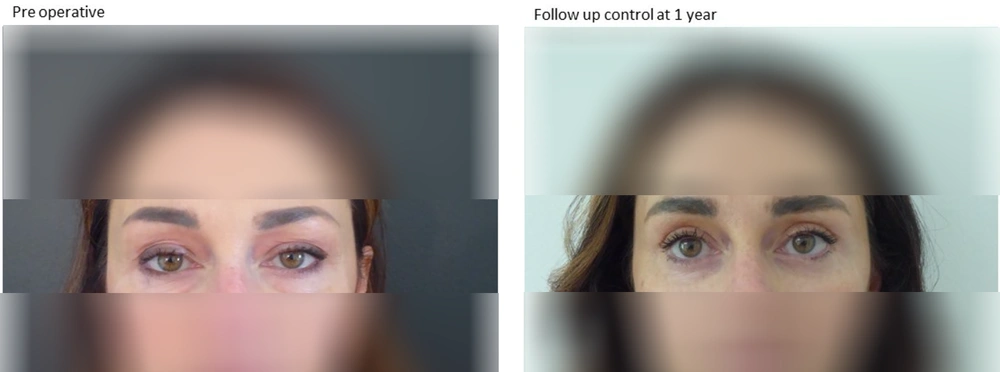
Ophthalmic Betadine was used to prep the periorbital area, while regular Betadine was used to prep the fat harvest site. For upper blepharoplasty, excess upper eyelid skin was sharply excised along with a small portion of the orbicularis muscle and the medial fat pad, if in excess. Lower blepharoplasty was performed with a subciliary incision, and a musculocutaneous flap was dissected up to the lower orbital edge. Excess adipose tissue was removed from the three fat pads, and a thin strip of skin and muscle was excised. Care was taken to ensure meticulous hemostasis in all phases of the surgery. The upper blepharoplasty incision was closed with a running intradermal Nylon 5 - 0 suture, while the lower blepharoplasty incision was closed with interrupted 4 - 0 Silk sutures. When performing lipofilling, 2% Mepivacaine with epinephrine was infiltrated at the harvesting cannula entrance site. Fat was harvested using a Tonnard Tulip cannula. The harvest sites were the inner knee for females and the flanks for males. A total of 20 - 40 mL of fat was harvested from each side (5). The choice of harvest sites was based on the increased stability and survivability of the fat in these regions, ensuring that if weight loss occurred postoperatively, there would not be a drastic change. Local anesthesia was avoided in the harvesting area to preserve the adipocytes as much as possible. The cannula entry site was closed with a 5 - 0 silk suture. Fat was processed according to the Coleman protocol, with centrifugation for 3 minutes at 3000 rpm to separate the nonviable components, which were then drained. Approximately 10 cc of the harvested fat was processed with the Tulip system as nanofat (6-8). Nanofat was produced by mechanical shuffling and filtration of microfat. Because the nanofat particles are extremely small, they do not provide notable volume effects. Studies indicate that nanofat contains abundant stromal cells and adipose-derived stem cells, which help reconstruct dermal support structures, such as collagen, and regenerate healthier, younger-appearing skin (9). In Italy, only mechanically treated stem cells are permitted, while enzymatic separation is prohibited. Microfat was injected using 25G cannulas for volume restoration, while nanofat was injected with 27 - 30G needles for fine rhytid filling and overall regenerative effects. Recently, a high-precision injection pen (Lipopen) has been used to provide greater uniformity of distribution; traditionally, injections were performed manually using syringes. Injections were performed slowly, with small boluses administered while withdrawing the cannula to avoid vascular occlusion and uniformly distribute fat. Microfat was placed with a microcannula in the tear trough and supraperiosteal in the lower eyelid. In other areas, such as the zygomatic region, microfat was placed subdermally into the subcutaneous tissue. A total of 4 - 15 mL was placed bilaterally to adequately restore volume. Nanofat was injected into the intradermal plane to form a wheal, which resorbed within a few days postoperatively.Surgical blepharoplasty typically took an average of 60 minutes to perform, and lipofilling added an average of 30 minutes to the procedure. Postoperatively, patients were observed for 30 minutes in recovery and then discharged home. Figures 1 and 2 illustrate two cases preoperatively and postoperatively.
3.4. Postsurgical Care
A dressing was applied over the incisions, ensuring the eyes could open and vision was not obstructed. An NSAID was administered postoperatively for 3 days to address pain, and antibiotics were also given. Immediately after surgery, a Pulsed Short Wave Therapy (PSWT) device (RecoveryRX, BioElectroninc, Frederick, MD, USA) was placed on each side to help reduce pain and inflammation. These devices were activated and checked to ensure proper functioning before placement. The device was secured to the head and face for 6 days until suture removal.Botox, 50 units, was injected one month postoperatively to decrease periorbital rhytids and enhance the aesthetic result. Botox therapy also helped reduce tension on the scar.
3.5. Outcome Measures
The outcome measures considered for comparison between the two groups were postoperative complications, patient-reported satisfaction levels, and postoperative pain on days 1 - 4 using a Numeric Rating Scale (NRS) (10, 11).
3.6. Data Analysis
Descriptive statistics were performed with proportions for categorical variables and means and standard deviations for normally distributed continuous variables. After assessing normal distribution, parametric tests (t-test, ANOVA) for repeated measures were applied to compare the differences between the two groups and analyze whether the type of procedure affected pain over time.
4. Results
This retrospective analysis included 109 patients with a mean age of 54.2 (SD ± 10.1). Of the 109 patients, 45 were in Group 1 (blepharoplasty alone) and 64 were in Group 2 (combined blepharoplasty-lipofilling). The average age was 53 years for both groups. In Group 1, 86% were female, and in Group 2, 89% were female. Demographic details are reported in Table 1. Pain control was rated as good to optimal in the majority of the sample in both groups. Satisfaction was rated as good in both groups, but dissatisfaction was reported by only two patients, with no statistically significant differences between the groups.
| Variables | Group 1 | Group 2 | P-Value | Chi2 |
|---|---|---|---|---|
| Blepharoplasty (N = 45) | Blepharoplasty + lipofilling (N = 64) | |||
| Age (y) | 54.3 | 54.1 | ||
| Gender | 0.65 | 0.21 | ||
| Females | 40 (89) | 55 (86) | ||
| Pain control: How would you judge it? | 3.04 | 0.22 | ||
| Insufficient | 0 (0) | 0 (0) | ||
| Sufficient | 0 (0) | 3 (5) | ||
| Good | 9 (20) | 17 (26) | ||
| Optimal | 36 (80) | 44 (69) | ||
| Satisfaction: Would you recommend it? | 1.74 | 0.42 | ||
| No | 0 (0) | 2 (3) | ||
| Yes | 42 (93) | 56 (88) | ||
| Maybe | 3 (7) | 6 (9) |
a Statistically Significant Difference, Alpha level of significant set below 0.05.
b Values are presented as mean SD or No (%).
The decision to add lipofilling to blepharoplasty was made by the patient during the preoperative consultation. Both groups were comprised of similar patients, with no significant differences in age, and females were predominant. The two groups showed similar characteristics at baseline, with no differences in age and an equal distribution of females (chi2 0.21, P = 0.65): 86% in the blepharoplasty alone group and 89% in the blepharoplasty plus lipofilling group.
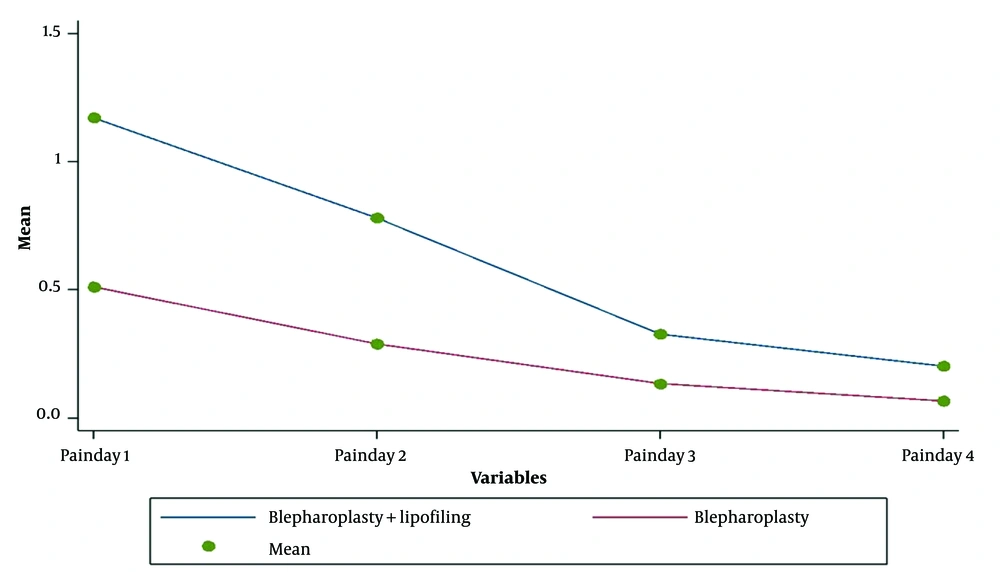
As reported in Table 2, pain scores were low for both groups. Higher scores were reported in the first two days in the blepharoplasty plus lipofilling group, but by days 3 and 4, the difference was no longer statistically significant (Figure 3). Postoperative complications reported by patients are shown in Table 3. Overall, 20% of patients (9 out of 45) undergoing blepharoplasty alone and 12% of patients (8 out of 64) undergoing blepharoplasty with lipofilling reported mild and transient problems.
a Values are presented as mean SD.
bAlpha level of significant set below 0.05.
| Variables | Group 1 | Group 2 |
|---|---|---|
| Blepharoplasty (N = 45) 9/45 | Blepharoplasty + lipofilling (N = 64) 8/64 | |
| Itching | 3 | 2 |
| Nausea | 3 | 3 |
| Hypotension | 2 | 1 |
| Headache | 0 | 2 |
| Bleeding | 1 | 0 |
5. Discussion
Retrospective analysis revealed that the integration of lipofilling with blepharoplasty is very successful and well tolerated by patients. The combination of the two procedures does not increase complications and enhances the aesthetics of the periorbita. The focus of this study was on postoperative pain, patient complications, and patient satisfaction. Although pain was reportedly higher in the blepharoplasty-lipofilling group, it was brief and described as a “mild ache.” Despite being statistically significant, the differences in pain between the groups were not clinically significant. The fact that patients in both groups stated they would undergo the surgery again is evidence that they tolerated the procedures well (12).
The best candidates for lipofilling combined with blepharoplasty are those who have had no prior surgery of the periorbita and, as suggested by Cohen (3), those with more advanced aging requiring more than 5 syringes of fillers. It is important to note that both groups included in the analysis had an average age of 53 years, which is in line with previous studies on blepharoplasty (10). The numerical rating scale (NRS) has been utilized to evaluate pain levels in a variety of disorders. It is widely recognized and accepted in all fields of medicine that a pain level below 3 is considered acceptable. Therefore, the average pain level reported by the patients in both groups in the present study can be interpreted as mild pain, an ache by definition (11, 13).
All our patients showed good compliance with the dressing and use of the devices, with no nuisances reported in the provided sheets. Postoperative bruising and ecchymosis are expected in the early postoperative period and are usually minimized by the application of cold compresses for 48 hours (14). However, the PSWT device has replaced the use of cold application. Ice packs are difficult to manage in the postoperative period as they obstruct vision and cause cold-related headaches. The sensitivity of fat cells to low temperatures is also well known (15). In our experience, the PSWT device for postoperative management allowed excellent control of pain and edema and improved wound healing, confirming the initial experience reported by Nicolle (16) and further supported by additional publications (17). Clearly, the addition of fat and stem cells provides a benefit in healing, as evidenced by the literature and patient postoperative courses. Postoperative management was the same for both groups, and patients in this study demonstrated compliance. Previously, ice packs were used, but they were difficult for the patient to manage, so the PSWT device was used to decrease pain and inflammation. In this surgeon’s experience, the PSWT has allowed for excellent postoperative pain control, decreased edema, and improved healing (18, 19).The current results are in agreement with the scientific literature. A recently published review with meta-analysis reveals that overall patient satisfaction is relatively high, ranging from 86.4% to 94.0%. Most complications were minor and could be easily treated or may disappear spontaneously. There was no high rate of severe complications (20). The level of evidence exploring these surgical techniques is still too low to provide a better understanding of the pros and cons of different surgical choices. Observational cohort studies comparing pain and complications outcomes in larger cohorts and with longer follow-up would enrich the current body of knowledge (21).This study did not demonstrate a significant increase in pain or complications for the patient; however, it did increase overall satisfaction and aesthetics. The authors are planning a long-term follow-up for the included patients to provide more insights on lipofilling integrated with blepharoplasty in the long term. Because of these results, a paradigm shift occurred during the 2002-2021 period, integrating lipofilling with all blepharoplasty surgeries. It is important to inform patients that even though the rejuvenation effects of fat grafting or lipofilling persist for long periods, they are not permanent, and the aging process will continue. Therefore, patients should understand their options regarding future modalities for the correction of rhytids (22, 23). Fat banks in the future could allow subsequent correction as aging and volume loss continue.