1. Introduction
Rosacea, a centrofacial inflammatory dermatosis, is classified into overlapping clinical stages such as erythematotelangiectatic, papulopustular, phymatous, and ocular, according to the National Rosacea Society (1). The disease primarily begins in females aged 20 to 30 years. Typically, lesions are exacerbated by photo-exposure, heat, alcohol, smoking, consumption of spicy foods, and emotional stress. Phymatous rosacea (from the Greek "phyma," meaning skin tumor) is more common in white men over the age of 50 (2, 3). It is a rare and chronic morphological subtype that occurs in untreated cases due to chronic inflammation, soft tissue hypertrophy, and fibrosis (2, 3). Phymas are named according to their location, such as rhinophyma (nose), mentophyma/gnathophyma (chin), metophyma (forehead), otophyma (ears), blepharophyma (eyelids), and zygophyma (cheeks) (4). Rhinophyma is the most common and is often the initial presentation. It is rare to observe multiple facial phymas in the same patient, where diffuse nodularity distorts the face, leading to cosmetic embarrassment (4). This kind of facial appearance is called leonine facies, as it resembles the face of a lion due to diffuse skin infiltration (5). Conditions such as lepromatous leprosy, leishmaniasis, scleromyxedema, actinic reticuloid, mycosis fungoides, and lymphomas can also present with this appearance (5).
Phymas with a giant pedunculated or pendulous appearance have not been reported in the literature until now. We present a case of a young Indian male farmer with rosacea who subsequently developed multiple facial phymas resembling leonine facies. Later, he presented with a grotesque, pedunculated tumor over his right cheek, mimicking a soft tissue tumor. The combination of these two rare clinical scenarios (phymatous rosacea resembling leonine facies and a pedunculated tumor-like mass on the cheek) necessitated histopathological analysis of the surgically excised mass, which revealed granulomatous rosacea. This case is being reported to highlight the giant pedunculated variant of phymatous rosacea, which can pose a diagnostic challenge in distinguishing it from soft tissue tumors.
2. Case Presentation
A 28-year-old male farmer from a rural area presented with a history of recurrent episodic facial flushing over the cheeks, chin, nose, and forehead for the past two years. He also experienced flares of reddish, elevated skin lesions associated with occasional burning sensations upon sun exposure in the same facial areas. On further questioning, he reported that his symptoms worsened after photo-exposure, consumption of hot and spicy foods, excessive alcohol intake, and emotional stress. He was previously treated for rosacea by a private practitioner with oral doxycycline (100 mg/day) and topical clindamycin 1% gel, along with advice for sun protection. However, the patient did not follow the recommendations and discontinued the treatment due to minimal relief at the start of therapy. He also continued working outdoors as a farmer without using sunscreens or physical sun protection. His lesions had a fluctuating course.
Over the past year, he developed progressive facial skin thickening and multiple irregular, skin-colored to yellowish nodules over the nose, cheeks, chin, forehead, and ears, resulting in facial disfigurement. Over the past six months, he developed a large, asymptomatic, progressively enlarging mass over his right cheek, causing a dragging sensation over his right lower eyelid. None of the nodules showed ulceration, and there was no history of weight loss or systemic symptoms.
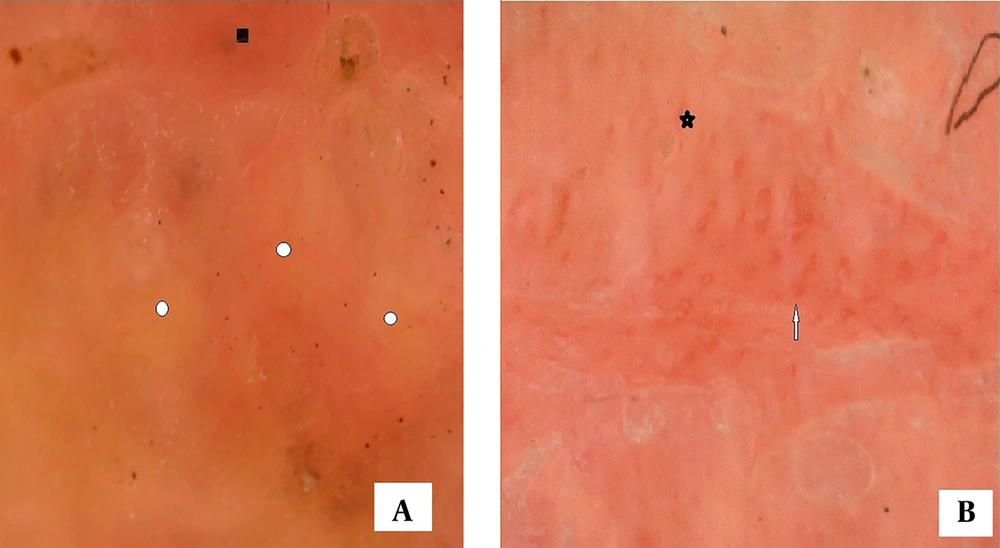
On examination, diffuse facial skin infiltration was noted, with seborrhea, dilated follicular ostia, and irregular nodularity resembling leonine facies (Figure 1A). A single, firm, non-tender, pedunculated, globose, skin-colored mass measuring 8 cm by 10 cm was present on the right cheek, with shiny overlying skin and patulous follicular ostia (Figure 1A). This mass could be lifted from the underlying skin and appeared pendulous (hanging like a pendulum). Upon lifting, it was observed that the skin beneath the mass was relatively spared from nodularity and infiltrative changes compared to the rest of the face (Figure 1B). The remaining cutaneous, sensory, and nerve examinations (conducted to rule out leprosy) were unremarkable. Systemic examination was within normal limits.
Diffuse facial nodularity on a background of seborrhea and patulous follicular ostia giving an appearance akin to leonine facies. There is a giant globose pedunculated mass over right cheek (A); upon lifting the mass, underlying skin looks relatively spared i.e. free from nodularity and infiltration (B).
A differential diagnosis of phymatous rosacea, scleromyxedema, actinic reticuloid, leprosy, leishmaniasis, and lymphoma was considered for the leonine facies, while neurofibroma, lipoma, fibroma, and giant acrochordon were considered for the pedunculated mass. Dermoscopy of the skin over the mass revealed yellow-orange structureless areas, telangiectasias, and some follicular plugs (seen as yellow dots) (Figure 2A and B). Routine hematological tests and urinalysis were normal. A slit skin smear test was negative (performed to rule out leprosy). There were no paraproteins in either blood or urine (paraproteinemia can be associated with scleromyxedema). A serum rk-39 antibody test (immunochromatography) was negative (performed to rule out leishmaniasis).
Dermoscopy: Orange-yellow structureless areas (white circles), background erythema (black square) (A); telangiectasias (white arrow) and follicular plugging (black star) (B); (yellow-orange structureless areas indicate underlying granulomatous aetiology/sebaceous component, telangiectasias indicate dermal vasodilatation and follicular plugs suggest infundibular occlusion. (Seen as yellow dots).
In the clinical context of phymatous rosacea (rhinophyma, metophyma, gnathophyma, otophyma, and zygophyma), the patient was advised strict photoprotection and avoidance of triggers. He was prescribed doxycycline 100 mg once daily (to be taken at night) along with topical metronidazole 0.75% gel. For the pathological diagnosis and treatment of the giant pendulous mass, the patient was promptly referred to plastic surgery, where he underwent cold-knife debulking with flap reconstruction (Figure 3).
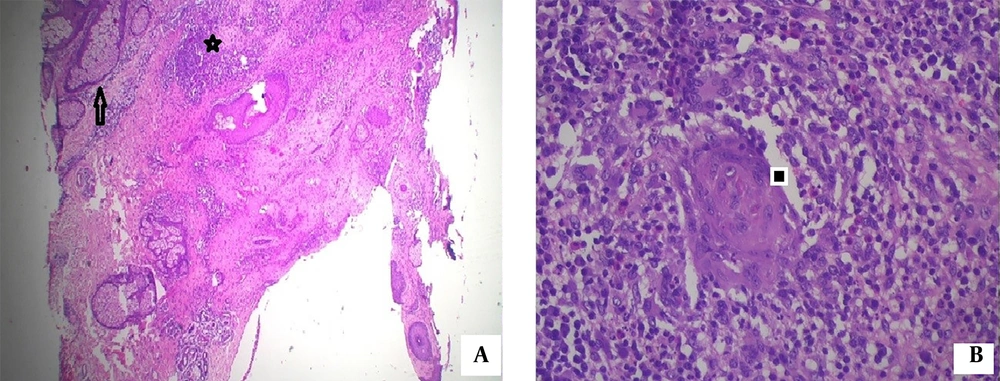
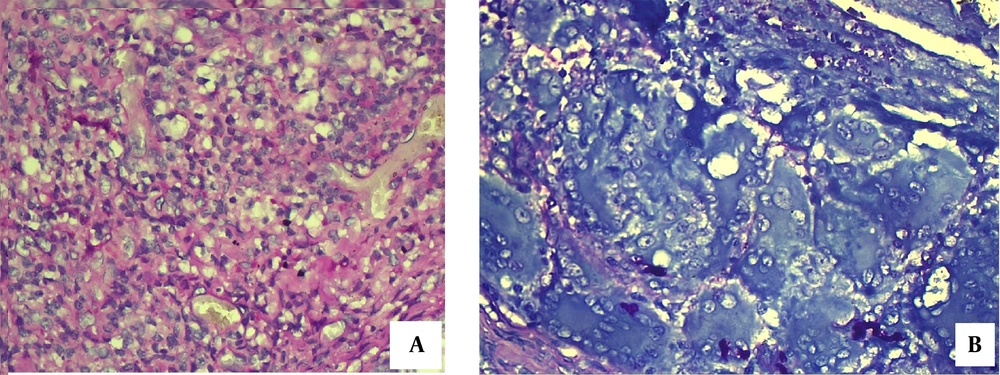
Histological evaluation (hematoxylin and eosin stain) of the excised specimen revealed sebaceous hyperplasia with dermal granulomas surrounding pilosebaceous units (Figure 4A), and higher magnification (40X) showed granulomas composed of epithelioid cells, giant cells (foreign body and Langhans' type), lymphocytes, and plasma cells (Figure 4B). These findings confirmed a diagnosis of granulomatous rosacea. Special stains, including Periodic acid-Schiff (PAS), showed no fungal elements within the granulomas (Figure 5A), and Giemsa stain did not reveal any leishmania parasites (Figure 5B).
Post-surgery, the patient was advised strict avoidance of potential triggers and photoprotection during the day, including the use of broad-spectrum sunscreens, full-sleeved clothing, a face mask, goggles, an umbrella, and a wide-brimmed hat. Pharmacotherapy with oral isotretinoin capsules was initiated at a dose of 20 mg every night, and he was administered a single dose of ivermectin (12 mg) for its anti-demodex action. The continuation of topical metronidazole 0.75% gel at night was recommended.
The interdisciplinary management approach included supportive care from ophthalmology (lubricating eye drops, use of goggles) and rhinoscopic and otoscopic examinations by otorhinolaryngology, which were unremarkable. Occupational therapy sessions were arranged to counsel the patient about transitioning to an indoor job from farming. This multipronged approach led to gradual improvement in seborrhea and diffuse facial nodularity after six weeks of continued treatment.
The patient is currently under regular follow-up, highly satisfied with the treatment, and is working as a watchman at a private firm (indoor job). There have been no recent disease flares.
3. Discussion
Rosacea, a condition characterized by its centrofacial distribution, can lead to significant cosmetic embarrassment in untreated cases. Phymatous rosacea typically presents with the characteristic "potato nose" (rhinophyma), marked by prominent, patulous follicular pores and mild swelling. In advanced cases, pronounced facial erythema, skin thickening, irregular nodularity, and distortion of facial architecture are common late-stage manifestations (6). Various factors contribute to the pathogenesis, including dysregulated neurohumoral inflammation, impaired vascular function, heightened innate immune responses, cytokine production, toll-like receptor activation, mononuclear cell activation promoting angiogenesis via vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF), and Demodex folliculorum infestation (3, 7). Histologically, phymatous rosacea can be classified into glandular, fibrous, fibroangiomatous, and actinic variants (1).
In our case, phymatous rosacea presented as a clinical combination of leonine facies and a giant pedunculated mass. The clinical similarities of phymatous rosacea with other conditions presenting with leonine facies were systematically ruled out. Lepromatous leprosy was excluded, as there were no nodular lesions elsewhere on the body, nor were there any sensory loss or neural symptoms. A slit skin smear for Mycobacterium leprae was negative. Histologically, there was no evidence of foamy histiocytes, perineural involvement, or involvement of the arrector pili muscles, further ruling out leprosy.
Scleromyxedema was ruled out based on the absence of paraproteins in both blood and urine, along with the lack of mucin deposition and spindle cell proliferation on histology. Deep mycoses were excluded due to the absence of fungal elements or suppurative granulomas on histological examination, a finding further supported by the Periodic acid-Schiff (PAS) stain, which showed no fungal elements.
Leishmaniasis was ruled out based on the absence of a history of kala-azar or travel to endemic areas, alongside a negative serum rk-39 antibody test. This diagnosis was further ruled out by Giemsa-stained tissue sections, which did not demonstrate any Leishmania parasites. Lymphoma, pseudolymphoma, and actinic reticuloid were excluded due to the absence of nodular or diffuse lymphocytic infiltrates, and no presence of atypical, activated, or large lymphocytes.
Regarding the giant, pedunculated tumoral zygophyma, which mimicked a soft tissue tumor, differential diagnoses included giant neurofibroma, lipoma, fibroma, or giant acrochordon. Microscopic analysis of the mass revealed granulomatous rosacea, effectively ruling out all these differentials.
Pharmacotherapy for severe phymatous rosacea, as in our case, has limited efficacy. Treatment options include oral isotretinoin (for its sebostatic and anti-inflammatory action), anti-inflammatory antibiotics like doxycycline, minocycline, and metronidazole (oral and topical), and ivermectin (for its anti-demodex action). However, the mainstream treatment approach for phymatous rosacea is surgical, as the disfiguring tissue hypertrophy and fibrosis are irreversible processes that are not corrected by medical therapies.
Various surgical treatment modalities are available for managing phymatous rosacea, including ablative carbon dioxide laser, radiofrequency ablation, and cold-knife surgery (2, 8, 9). Carbon dioxide laser and radiofrequency ablation offer advantages such as a bloodless surgical field, a shorter learning curve, and reduced post-operative downtime compared to cold-knife plastic surgery. However, these techniques are limited in treating larger surface areas (such as the full face in our case), which may require flap reconstruction, and they do not preserve tissue architecture, often creating artifacts in the tissue, making histopathological analysis difficult.
In our case, cold-knife surgical debulking with flap reconstruction was chosen to preserve tissue architecture for necessary microscopic examination, as histological analysis was crucial to rule out clinical mimics of soft tissue tumors. Additionally, a rotational flap was required to close the large facial defect created after excision of the giant pedunculated zygophyma, which was made possible by the conventional cold-knife approach.
Sakhiya et al. successfully treated rhinophyma with an ultra-pulsed carbon dioxide laser (1). Chen et al. reported a rare association of vestibulophyma and giant rhinophyma, managed by surgical debulking, turbinectomy, and flap reconstruction (2). Blairvacq et al. reported a rare combination of otophyma, zygophyma, and giant rhinophyma, which was treated with surgical debulking and dermabrasion (9).
Our case presented with a rare combination of various phymas, including rhinophyma, metophyma, blepharophyma, gnathophyma, otophyma, and a giant pedunculated zygophyma. Pedunculated phymas have not been previously reported in the literature. Interestingly, we observed that the skin beneath the pendulous phyma was relatively spared from nodularity and infiltrative changes, while the remainder of the face exhibited diffuse nodularity. This sparing could be attributed to the natural "umbrella effect" of the overlying giant mass, which protected the skin underneath from sun exposure. This observation underscores the importance of photoprotection as an integral part of treatment.
This case also highlights the need for early and prompt plastic surgical intervention in phymatous rosacea to prevent facial distortion and cosmetic embarrassment. Avoidance of rosacea triggers and adherence to medical therapy further enhance aesthetic outcomes.
5.1. Conclusions
Phymatous rosacea may present as diffuse facial nodularity resembling leonine facies, necessitating clinicopathological differentiation from conditions such as leprosy, leishmaniasis, lymphoma, deep mycoses, and scleromyxedema. A rare presentation of phymatous rosacea, as seen in our case, involves a large pedunculated phyma that can mimic soft tissue tumors such as neurofibroma, lipoma, giant acrochordon, or even more serious malignancies. Therefore, sound clinical judgment, a high index of suspicion for diagnosing this rare entity, thorough investigative support (including bedside tools like dermoscopy, hematological and biochemical tests), and crucial histopathological analysis (with special stains) are all essential for effective management.
An early and prompt cold-knife excisional approach with plastic flap reconstruction proves to be a valuable treatment strategy, ensuring better cosmetic outcomes. Delayed surgical intervention can lead to significant architectural distortion of the face, including the facial skeleton. Furthermore, counseling on the strict avoidance of potential triggers and a commitment to continued medical therapy are vital pillars for achieving long-term therapeutic success.