1. Introduction
Gout is a metabolic disorder caused by hyperuricemia, leading to the abnormal accumulation of monosodium urate crystals in joints, skin, and soft tissues. Chronic gouty tophi present as intradermal or subcutaneous asymptomatic swellings, appearing as erythematous or skin-colored nodules predominantly distributed over less vascular areas such as the ears, olecranon process, pre-patellar bursae, or juxta-articular locations (1). Tophi typically develop up to ten years after recurrent episodes of acute or chronic arthritis and may serve as a clinical marker for underlying hyperuricemia. Large tophi can result in significant functional and cosmetic impairment (2).
We present a rare case of a middle-aged man who developed chronic, grotesque gouty tophi over multiple joints, along with an intriguing presentation of alopecia caused by perifollicular urate crystal deposition. This case highlights a unique instance of non-scarring alopecia associated with gout, characterized by uric acid crystal deposition around hair follicles, which led to reduced hair growth and potentially disrupted hair physiology. Remarkably, the condition exhibited a significant response to uric acid-lowering therapy, making it the first documented case of its kind in medical literature.
2. Case Presentation
A 45-year-old male watchman presented with a five-year history of progressive, asymptomatic, skin-colored, firm nodules over both hands, forearms, elbows, feet, and knees, leading to deformities and restricted movements. He also reported a progressive patch of hair loss on the occipital scalp over the past six months. On further inquiry, he disclosed a history of chronic, intermittent joint pain and swelling involving the small joints of the hands, elbows, knees, and ankles for the past 15 years. He denied any history of early morning joint stiffness, ulceration, or extrusion of chalky white material from the nodules. The patient was a chronic alcoholic but had no family history of gout or metabolic syndrome and no systemic complaints.
Cutaneous examination revealed multiple, skin-colored, firm-to-hard, non-tender, dermal, and subcutaneous nodules, along with large globose tumoral lesions ranging in size from 1 cm × 1 cm to 10 cm × 8 cm in diameter. These were located over the dorsal surfaces of the hands, interphalangeal joints, forearms, elbows, knees, dorsal feet, ankles, and interphalangeal joints of the feet, accompanied by joint deformities (Figure 1A - C). The overlying skin was mobile, without signs of inflammation or ulceration.
Scalp examination revealed a single, smooth, alopecic patch measuring 2 cm × 2 cm on the occipital region, with an indurated feel on palpation (Figure 1D). Mucosal and systemic examinations were unremarkable. Based on clinical findings, the highest suspicion was tophaceous gout, with a differential diagnosis including tuberous xanthomas, calcinosis cutis, and rheumatoid nodules.
The occipital alopecia was initially considered as either alopecia areata or lipedematous alopecia. A hair pull test from the patch was negative, and no dimpling was observed on pressure. Trichoscopy revealed multiple small and large white dots corresponding to eccrine ostia and empty hair follicles, respectively. There was an absence of black dots, broken hairs, exclamation mark hairs, and linear telangiectasias, which ruled out alopecia areata and lipedematous alopecia.
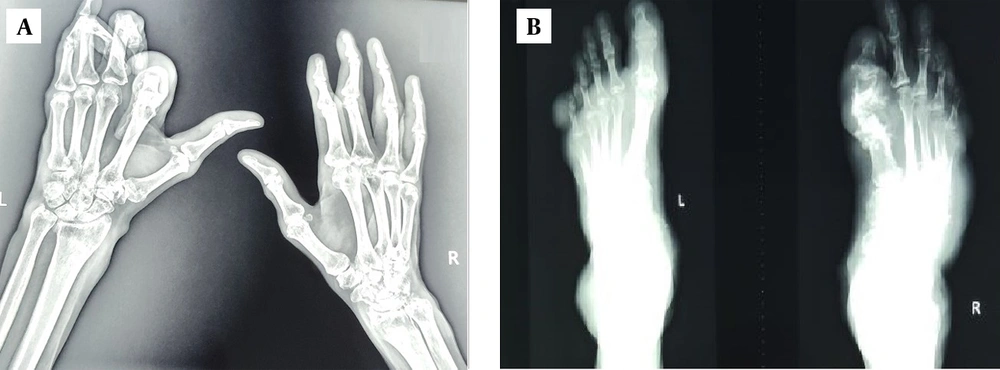
Hematological investigations revealed a normal hemogram, hepatic function tests, and serum lipids. Serum uric acid was elevated (10.3 mg/dL; normal range 2.5 - 7 mg/dL), while the rest of the renal function tests were normal. The arthritis panel, including rheumatoid arthritis (RA) factor, anti-cyclic citrullinated peptide (anti-CCP) antibody, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR), was unremarkable. Radiological examination of the ankles, knees, elbows, and hands showed soft tissue densities, cortical erosions in juxta-articular locations, and phalangeal resorption (Figure 2A and B). Ultrasonography of the abdomen revealed nephrolithiasis.
A skin punch biopsy from a cutaneous nodule (Figure 3A) showed pale eosinophilic amorphous deposits surrounded by histiocytes (tissue macrophages) and foreign body giant cells, consistent with monosodium urate crystals, confirming tophaceous gout. Biopsy from the occipital alopecic patch surprisingly revealed similar amorphous material (urate crystals) in a parafollicular location (Figure 3B and D). A final diagnosis of chronic tophaceous gout with gouty alopecia was established.
A, [H&E,10X]-gouty tophus (green arrow) with histiocytic palisading; B, tophi on scalp (green star) with amorphous pale eosinophilic material; C, perifollicular urate deposition (red arrow) with bluish appearance; D, [H&E-40 X]-para-follicular amorphous pale eosinophilic urate material (red circle).
Multidisciplinary consultations were sought from orthopedics and plastic surgery for joint deformities and from nephrology for nephrolithiasis. The patient was started on oral allopurinol at 100 mg three times a day, along with short courses of non-steroidal anti-inflammatory drugs (NSAIDs) for managing acute arthritic pain. He was advised to follow a purine-restricted diet, avoid alcohol, and maintain adequate hydration.
After six months of continuous therapy, the patient experienced marked symptomatic relief from joint pain, and his serum uric acid level decreased from 10.3 mg/dL to 7.9 mg/dL. Although the tophi persisted post-treatment (Figure 4A and B), the occipital alopecia showed complete hair regrowth (Figure 4C).
3. Discussion
Gout can result from excessive uric acid production or impaired excretion. Various underlying factors increase the risk, including a high-purine diet (primarily non-vegetarian food), chronic diuretic or cyclosporine therapy, chronic alcoholism, postmenopausal status, and the inability to consume hypouricemic drugs due to allergy or impaired renal clearance of uric acid. Male gender and postmenopausal females (due to low estrogen levels) are predominantly affected by gout (2). Our patient had a history of chronic alcoholism.
Tophaceous gout typically occurs after a latency of 3 - 42 years (mean 12 years) of untreated disease, resulting from the accumulation of monosodium urate crystals (1, 2). It preferentially involves joints, bursae, ligaments, and tendons, especially the olecranon bursa, infrapatellar and Achilles tendons. Subcutaneous deposits may also occur over the wrists and hands (1, 2). Unusual sites of involvement include the ear helix, nasal cartilage, eyelids, cornea, and even tricuspid and mitral valves (3, 4). Beier et al. reported rare cases of erosive intraspinal and paravertebral lesions, as well as carpal tunnel syndrome resulting from tophi accumulation (5). Negbenebor et al. and Pattanaprichakul et al. described rare presentations of gouty panniculitis (6, 7).
Morphologically, cutaneous tophi appear as cream-colored to yellowish firm nodules that are mobile, with overlying skin that is often thin and reddish. A diverse array of morphologies has been reported, including bullous, fungating, and ulcerative variants (8). An intriguing variant of cutaneous gout characterized by generalized milia-like eruptions of tophi is termed miliarial gout (9).
Our patient presented with multiple disseminated peri-articular, intradermal, and subcutaneous gouty tophi. A range of differential diagnoses, including multicentric reticulohistiocytosis, rheumatoid nodules, and tuberotendinous xanthomas, was ruled out based on clinicopathological analysis. Additionally, the patient exhibited an enigmatic presentation of gouty occipital alopecia caused by urate crystal deposition in the parafollicular region, which showed a favorable response to uric acid-lowering therapy (allopurinol). This rare presentation, to the best of our knowledge, has not been previously reported.
A thorough literature search revealed several intriguing case reports. Song et al. described a case of gouty tophi in the head and neck region, with urate crystal deposits on the pinna and nasal septum, treated successfully with plastic reconstruction (10). Emanuel and Paul reported a case resembling erosive pustular dermatosis of the scalp with alopecia, where histopathology revealed pale-eosinophilic urate-like crystal deposits in the epidermal crust (11). This condition showed satisfactory resolution with systemic minocycline and topical calcipotriol.
A previously described entity, necrotizing infundibular crystalline folliculitis (NICF), presents with urate-like crystalline deposits within the follicular infundibulum but without hyperuricemia or gout. Clinically, NICF manifests as waxy follicular papules, with the deposits linked to local microorganisms or cellular debris (12). Lucke et al. (as cited in Emanuel and Paul) suggested that disrupted epidermal or follicular tonofilaments embedded in an amorphous matrix may contribute to NICF pathogenesis (11, 12). Walsh et al. (as cited in Emanuel and Paul) observed urate-like crystals associated with dermal xanthomas, supporting the hypothesis that a reaction to lipid or sebum-rich contents may also lead to crystallization (11).
Conditions such as erosive pustular dermatosis of the scalp, NICF, and xanthomas require histopathological differentiation from urate crystals, as they can produce amorphous deposits resembling urate crystals in the scalp. However, these entities have distinct clinical features, are not associated with hyperuricemia, and require different therapeutic strategies. Colchicine-induced alopecias, as reported by Duff et al. and Malkinson and Lynfield, are unrelated to urate crystal deposition and are instead attributed to colchicine's anti-mitotic effects (13, 14).
The dermoscopic features of alopecia areata include yellow dots, vellus hairs, black dots, exclamation mark hairs, and broken hairs (15). Trichoscopy of lipedematous alopecia reveals linear telangiectasias (16). In our case, small and large white dots corresponding to eccrine and empty follicular ostia were observed. These findings were non-specific for gouty alopecia but effectively ruled out alopecia areata and lipedematous alopecia (16).
The treatment of chronic tophaceous gout involves a combination of dietary, medical, and surgical strategies. Dietary modifications include adherence to a low-purine diet, avoiding meat, seafood, and alcohol. Medical treatment encompasses the use of NSAIDs or colchicine for acute joint pain relief, alongside hypouricemic agents such as allopurinol or febuxostat and uricosuric drugs like probenecid and sulfinpyrazone as disease-modifying agents. Our patient responded well to allopurinol and episodic NSAID therapy for acute pain relief. Surgery is generally reserved for tophi located in critical areas, chronically draining nodules, or those causing severe joint pain or articular deformities. Conventional enucleation is typically avoided as it may lead to complications like skin necrosis or exposure of underlying tendons or joints. A “shaver technique” for managing deformities has been described by Lee et al. (17). In this case, a plastic surgical consultation was sought for the debilitating tophi.
The unique features of this case include the unusual presentation of disseminated gouty tophi and gouty alopecia (confirmed by biopsy showing parafollicular urate crystal deposition). To the best of our knowledge, this is the first reported case of gouty alopecia caused by urate crystal deposition in the scalp. The authors hypothesize that this alopecia may result either from the pressure effect of urate crystals or from metabolic or tonofilament-related alterations caused by gouty tophi. This hypothesis warrants validation through further studies involving larger sample sizes.
Gouty alopecia was initially confounded with alopecia areata and lipedematous alopecia; however, biopsy findings provided a definitive diagnosis. Both the arthritic symptoms and alopecia showed a remarkable response after six months of allopurinol therapy, with the alopecia demonstrating complete hair regrowth.
5.1. Conclusions
A combination of disseminated cutaneous tophaceous gout and alopecia due to urate crystal deposition presents a challenging diagnostic enigma. Accurate diagnosis necessitates thorough clinical evaluation, supported by hematological, radiological, and histopathological investigations. Clinical mimics such as xanthomas, rheumatoid nodules, and multicentric reticulohistiocytosis may complicate the diagnosis of gouty tophi, while alopecia areata and lipedematous alopecia (both non-cicatricial alopecias) can resemble gouty alopecia, a very rare presentation of gout.
An early biopsy of such alopecic patches is crucial to identify the underlying cause and enable timely therapeutic intervention. The alopecia observed in this case may be attributed to factors such as mechanical pressure exerted by urate crystals, tonofilament alterations within the follicle, or disruptions in hair cycle dynamics. These findings underscore the need for further research to elucidate the pathophysiology of gouty alopecia.


![A, [H&E,10X]-gouty tophus (green arrow) with histiocytic palisading; B, tophi on scalp (green star) with amorphous pale eosinophilic material; C, perifollicular urate deposition (red arrow) with bluish appearance; D, [H&E-40 X]-para-follicular amorphous pale eosinophilic urate material (red circle). A, [H&E,10X]-gouty tophus (green arrow) with histiocytic palisading; B, tophi on scalp (green star) with amorphous pale eosinophilic material; C, perifollicular urate deposition (red arrow) with bluish appearance; D, [H&E-40 X]-para-follicular amorphous pale eosinophilic urate material (red circle).](https://services.brieflands.com/cdn/serve/3170b/3b00629c11be4677ddad30090186296b12ef9e12/jssc-157440-g003-F3-preview.webp)
