1. Introduction
Vesiculobullous disorders are classified into various categories based on the type of antigen involved and the level of split observed on histopathological examination. Pemphigus vulgaris is characterized by a suprabasal split and falls under the group of autoimmune blistering disorders, primarily targeting desmoglein (Dsg) 3, Dsg1, and very rarely desmocollin. The incidence of pemphigus in India ranges from 0.09% to 1.8% (1). Neutrophilic dermatoses are characterized by the presence of a noninfectious infiltrate predominantly composed of mature neutrophils. Pyoderma gangrenosum is a type of neutrophilic dermatosis that predominantly involves the skin and is frequently associated with systemic diseases such as arthritides and enthesopathies (37%), ulcerative colitis, systemic lupus erythematosus, Crohn's disease, and myeloid leukemia. It is a very uncommon disease with a chronic and recurrent course, characterized by sterile ulcers. It has a general incidence of 3 to 10 cases per million per year (1). There are only three case reports showing the coexistence of vesiculobullous disorders with pyoderma gangrenosum. Of these, two cases demonstrate the coexistence of pemphigus vulgaris with pyoderma gangrenosum (2, 3), and there is a single case report of bullous pemphigoid with pyoderma gangrenosum (4).
2. Case Presentation
A 42-year-old female presented with oral intolerance to spicy food and erosions over the buccal mucosa for 2 months. She also had multiple fluid-filled blisters and erosions over the body for the last month. Based on history, the erosions had a small tendency to heal and easily progressed to the surrounding area. There was no history of fever, joint pain, photosensitivity, recent drug intake, or vaccination, and no similar complaints in the past or among family members. On examination, her vital parameters were within normal limits, and systemic examinations were unremarkable. Dermatological examination revealed multiple erosions with thick brownish-yellow adherent crusts over the face, chest, bilateral upper limbs, and lower limbs with an offensive odor. There were multiple ulcers present over the bilateral buttocks and right elbow. Extensive erosions were present over the back with areas of pinpoint bleeding (Figure 1). The scalp showed crusted erosion with matting of hair. Direct and marginal Nikolsky’s signs from the trunk were positive. Mucosal examination revealed few erosions over the buccal mucosa and inner aspect of the lip, vulval and perianal region, as well as labia majora and minora. Ocular examination showed congestion. There were no lesions on the palms and soles, and nails were normal. A clinical diagnosis of pemphigus vulgaris was considered based on history and clinical findings.
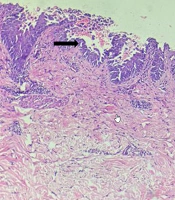
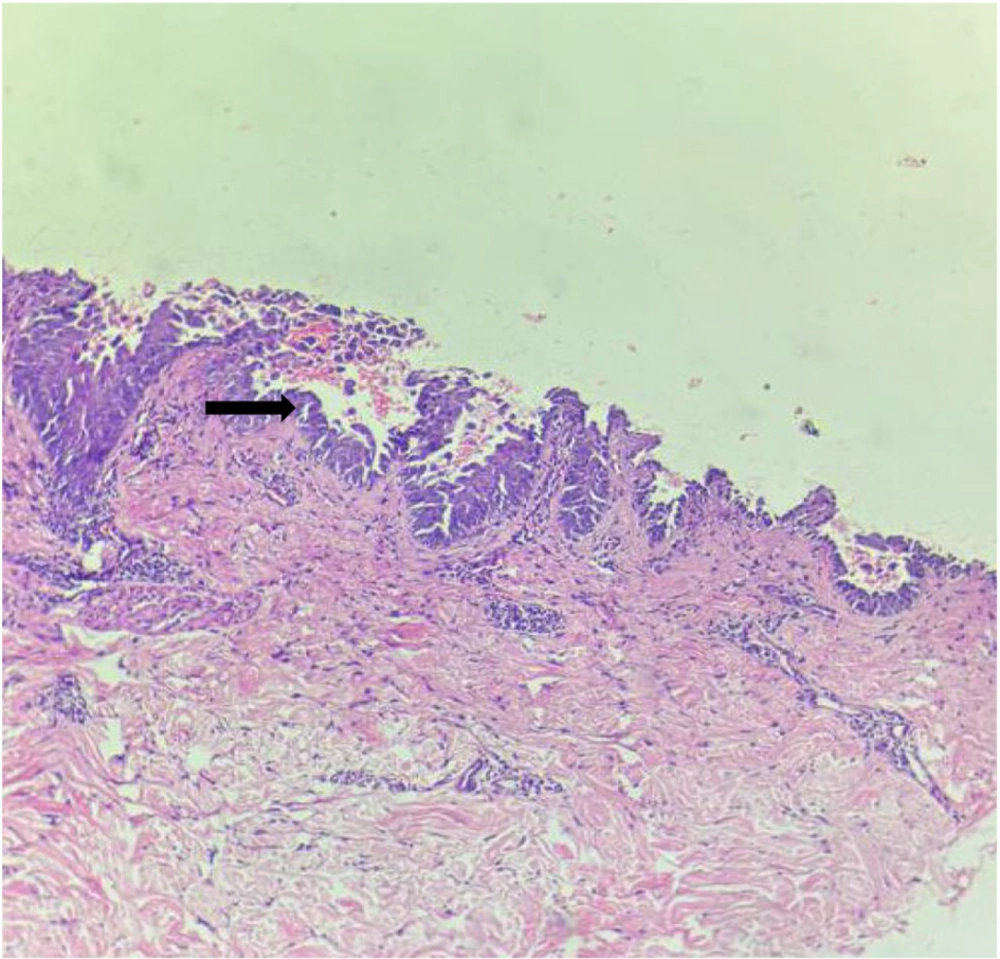
Hematological investigations revealed decreased hemoglobin (8.6 gm/dL), deranged liver function tests with elevated serum transglutaminase (300 IU/dL) and serum transaminase (256 IU/dL). Other routine investigations were within normal limits. Serological viral markers were negative. Radiological investigations and electrocardiogram (ECG) were also normal. A skin biopsy from the margin of an erosion (chest) was performed, showing a suprabasal cleft with a row of tombstone appearance of the basal layer with multiple acantholytic cells (Figure 2). Thus, the final diagnosis of pemphigus vulgaris was made.
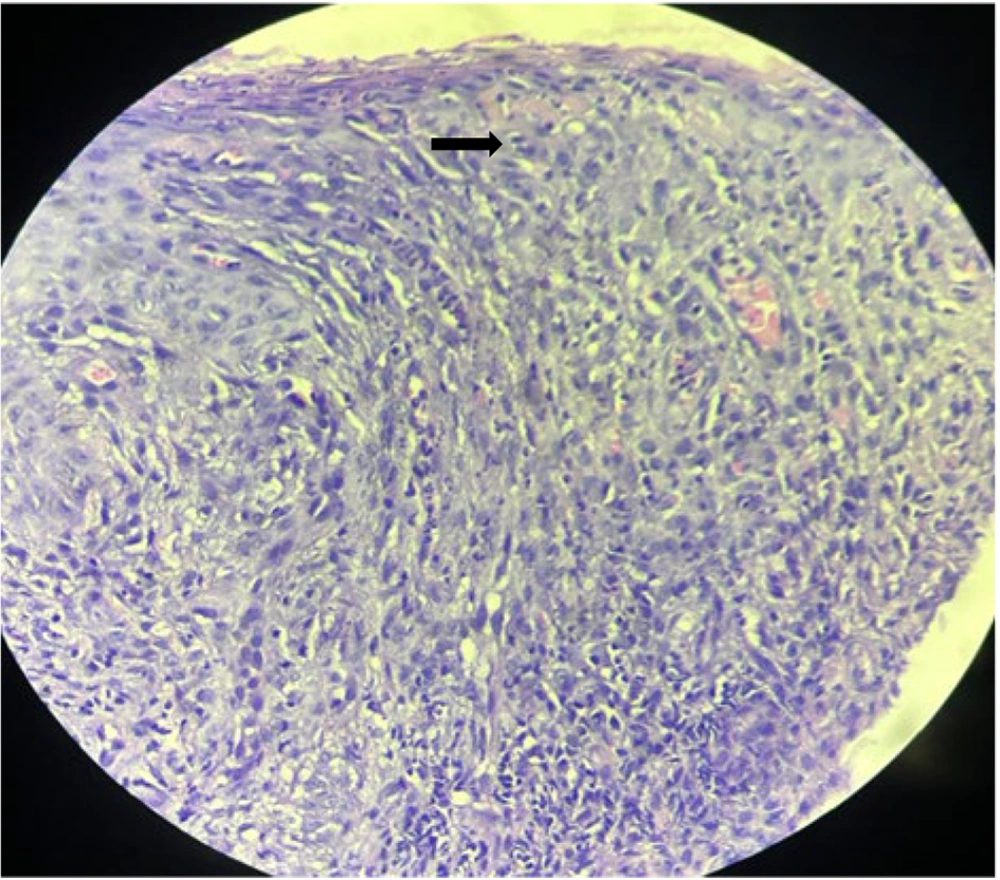
The patient was treated with intravenous antibiotics (piperacillin-tazobactam) according to the pus culture sensitivity report. Blood transfusion, i.e., two bags of packed cell volume (PV), was given for low hemoglobin. Local care included topical antibiotics with barrier nursing care, Condy’s compresses, normal saline compresses, along with triamcinolone acetonide (0.1%) buccal paste, Condy’s gargles, and clotrimazole mouth paint. The patient was started on injection dexamethasone 8 mg daily dose. However, the ulcers on the buttocks and right elbow were not healing, so a repeat biopsy from the ulcer margin over the buttock was sent, considering a possible diagnosis of pyoderma gangrenosum. Histopathology from the ulcer margin showed hyperkeratinized acanthotic epidermis with ulceration up to the superficial dermis with dense polymorphonuclear cells and deeper dermis having periadnexal and perivascular collection of polymorphs and lymphocytes, confirming the diagnosis of pyoderma gangrenosum (Figure 3).
Along with a daily dose of injection dexamethasone, she was given injection dexamethasone 100 mg daily pulse for 3 days, after which the daily dose of dexamethasone was tapered slowly. Corticosteroids are the primary immunosuppressants for pyoderma gangrenosum and pemphigus vulgaris. They cause immunosuppression by sequestering CD4+ T lymphocytes in the reticuloendothelial system and by inhibiting the transcription of cytokines IL-1, IL-2, IL-6, IFN-alpha, TNF-alpha, and GM-CSF (5). Other immunosuppressives like azathioprine, mycophenolate mofetil, or cyclophosphamide were not given due to deranged lab parameters (low hemoglobin, high WBC, and deranged liver function tests). Hence, after completion of 3 weeks of injection dexamethasone pulse therapy, the patient was given 1 gm of injection rituximab. Rituximab acts by depleting CD20+ B cells, which produce antibodies pathognomonic to pemphigus vulgaris (6). Rituximab binds to the CD20 on circulating as well as tissue-based B-cells and induces apoptosis by complement-dependent cytotoxicity and antibody-dependent cellular cytotoxicity. As per the rheumatoid arthritis (RA) protocol, the patient was given two doses of 1 gm injection rituximab 15 days apart, with stringent monitoring.
After 8 weeks, most of the erosions healed with hyperpigmentation, and the ulcers over the buttocks and elbow healed by cribriform scarring. A few of the erosions over the back and buttocks healed by hypertrophic scar formation (Figure 4). Complete resolution of the existing lesions with no appearance of new lesions was achieved by the end of 4 months. She is currently under regular follow-up, being maintained on gradually tapering doses of prednisolone with stringent monitoring. Even after the follow-up period of one year, the patient is still in remission.
3. Discussion
Pemphigus is derived from the Greek word “pemphix,” which means “blister.” Among the pemphigus group of disorders, pemphigus vulgaris (PV) is the most common type. It is an autoimmune disease with mucocutaneous blistering characterized by antibodies against Desmoglein 3, Dsg1, and rarely desmocollin. It has a peak incidence between the fourth and fifth decades of life, mostly affecting individuals between 40 and 60 years, with a female preponderance. It has a racial predilection and is more commonly encountered in Ashkenazi Jewish populations and Eastern countries, such as India, Malaysia, China, and Japan. Pemphigus vulgaris usually presents as multiple vesicles, bullae, and crusted erosions mostly affecting the skin and mucosa with occasional itching. The bullae rupture easily to form erosions, which have little tendency to heal and spread easily to the surrounding skin. The lesions of pemphigus mostly heal by hyperpigmentation but usually without scarring (1). Our patient had thick adherent brownish crusted erosions with extensive involvement of the trunk and mucosa, with a positive Nikolsky’s sign.
Corticosteroids are the mainstay of treatment for pemphigus vulgaris, which can be combined with other oral immunosuppressive agents like azathioprine, mycophenolate mofetil, and cyclophosphamide. Another FDA-approved therapy is rituximab. In our patient, we administered daily injection dexamethasone 8 mg along with injection dexamethasone 100 mg pulse therapy for 3 days, followed by injection rituximab as per the RA protocol, 1 gm, 15 days apart after 3 weeks (7).
Pyoderma gangrenosum is a chronic, uncommon, recurrent, idiopathic, sterile, ulcerating condition predominantly involving the skin, with a neutrophilic inflammatory infiltrate, and frequently associated with systemic disease. The peak incidence is between 40-60 years of age, with a higher incidence among women. It is estimated that there are 3 cases of pyoderma gangrenosum per million population per year. The mechanism is based on the hypothesis that lymphocytic antigenic stimulation takes place in the skin with subsequent stimulation of clonal proliferation in the lymph node and recirculation to the skin, culminating with cytokine release and recruitment of neutrophils (1). Pyoderma gangrenosum is associated with systemic comorbidities in approximately 50% of patients. Rheumatoid arthritis is the most common association in adults, whereas in children it is ulcerative colitis. Other diseases associated with PG include Crohn’s disease, myeloid leukemia, multiple myeloma, systemic lupus erythematosus, HIV, Hepatitis C, solid tumors of the colon, pancreas, breast, carcinoid, sarcoidosis, diabetes mellitus, and Hashimoto thyroiditis (1). There are various morphological variants of pyoderma gangrenosum, namely, ulcerative, pustular, bullous, and vegetative. In our patient, there was a painful ulcer with violaceous and undermined borders present over the buttocks and the elbow. Histopathology of the lesion showed a dense neutrophilic infiltrate. The lesions later healed with cribriform scarring, satisfying the criteria for pyoderma gangrenosum.
Management of pyoderma gangrenosum includes local wound care, topical and systemic corticosteroids, and other immunomodulators like dapsone, azathioprine, and cyclosporine. However, in our patient, the corticosteroid started for pemphigus vulgaris was also effective in controlling pyoderma gangrenosum. After a thorough literature search, we found only three case reports showing the association of pyoderma gangrenosum with vesiculobullous disorders. Out of three, there were two case reports of pyoderma gangrenosum associated with pemphigus vulgaris (2, 3) and a single case report of pyoderma gangrenosum with bullous pemphigoid (4). The association between the two can be correlated by the autoimmune nature of both diseases and cross-reactivity of antigens. In pyoderma gangrenosum, there is a role of IL-8 as it attracts neutrophils and IL-16 in the pathogenesis. Whereas, in pemphigus vulgaris, it was found that the lesions showed increased levels of IL-8, contributing to the inflammatory responses around the bullae and attracting neutrophils and damaging the tissue (3). Though PG and PV have different primary mechanisms (neutrophilic vs. autoantibody-mediated), IL-8 may play a shared inflammatory role in both (2).