1. Introduction
Intravenous (IV) drug use, particularly involving heroin and other opioids, is an escalating public health issue globally, with a broad spectrum of medical complications. Among these, dermatologic manifestations are frequently the first visible sign of substance abuse, often providing essential diagnostic clues in both clinical and forensic settings. The spectrum of cutaneous findings in IV drug users is vast, ranging from simple needle marks and abscesses to more complex presentations such as chronic ulcerations, panniculitis, and granulomatous dermatoses (1). In individuals using opioids like heroin, the risk of encountering deep fungal, bacterial, or atypical mycobacterial infections is significantly increased due to the use of non-sterile injection techniques, contamination of injectable material, and repeated trauma to the skin and subcutaneous tissues (1).
However, not all lesions in these patients are infectious. Non-infectious inflammatory reactions, especially those caused by injected insoluble foreign substances, represent an underdiagnosed yet critical differential. Insoluble adulterants such as talc, starch, silica, and other fillers are commonly added to heroin to increase its bulk, mimic purity, or modify its appearance and texture (2). When inadvertently injected into subcutaneous tissues or vasculature, these materials may incite robust granulomatous inflammatory responses, which can clinically mimic infectious processes, including sporotrichoid nodular lymphangitis (1). This pattern, typically seen in infectious etiologies such as sporotrichosis and atypical mycobacterial infections, involves the linear arrangement of nodules along lymphatic drainage channels and is often mistaken for classical nodular lymphangitis (3). We present a rare and compelling case of such a granulomatous reaction, wherein polarized light microscopy played a pivotal diagnostic role.
2. Case Presentation
A 21-year-old unmarried male, with a known history of opioid dependence, presented to our dermatology outpatient department following referral from the psychiatry de-addiction unit. He complained of multiple, painful, slowly progressive skin lesions over both forearms and upper arms for the past three months. These lesions had started as firm nodules that gradually enlarged, became erythematous, tender, and in some instances, ulcerated with seropurulent discharge. The distribution of the lesions was notably linear, following the course of superficial veno-lymphatics, in a classic sporotrichoid lymphangitic pattern.
The patient admitted to injecting heroin intravenously for over a year, often using multiple and unconventional sites due to difficulties accessing veins. His injection practices were inconsistent, frequently performed without sterile techniques. He reported no associated systemic symptoms such as fever, malaise, night sweats, joint pain, or weight loss. There was no recent travel or history of exposure to fish tanks, animals, or soil that might suggest an environmental fungal or atypical bacterial infection. He denied any other comorbidities and was not taking any medications other than those prescribed in the de-addiction program.
On clinical examination, both upper limbs exhibited multiple nodules ranging from 0.5 to 2 cm in diameter, with overlying erythema, tenderness, and crusting. A few lesions had broken down to form ulcers with seropurulent discharge. The nodules and ulcers were distributed in a linear fashion along the lymphatics of the forearms and arms (Figure 1A and B). There was evidence of chronic injection site scarring, skin thickening, and post-inflammatory hyperpigmentation. No regional lymphadenopathy or systemic signs were evident at the time of evaluation.
Based on the clinical history and examination findings, the differentials included deep mycoses (sporotrichosis, histoplasmosis, blastomycosis), atypical mycobacterial infections (fish tank granuloma/infection with environmental mycobacteria including rapid growers), nocardiosis, actinomycosis, and botryomycosis. Laboratory investigations, including complete blood count, liver, and renal function tests, were within normal limits. Serological tests for human immunodeficiency virus (HIV), hepatitis B surface antigen (HBsAg), and hepatitis C virus (HCV) were non-reactive. Given the clinical suspicion of an infectious etiology, a punch biopsy was obtained from an active nodule, and samples were sent for bacterial, fungal, and mycobacterial cultures.
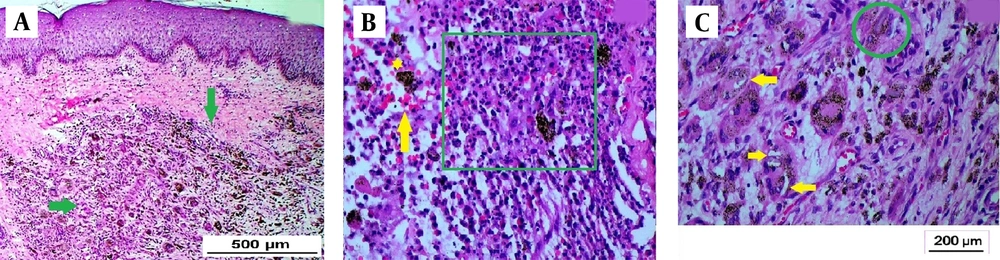
Hematoxylin and eosin-stained examination of the biopsy specimen revealed a dense dermal infiltrate composed of pyogranulomatous inflammation with areas of central suppuration (Figure 2A). Numerous hemosiderin-laden histiocytes and foreign body-type giant cells were observed. The pigment was identified as hemosiderin rather than melanin, as evidenced by its golden-brown, refractile appearance and the presence of extravasated red blood cells, supporting hemosiderin deposition over melanin (Figure 2B). Within the cytoplasm of histiocytes and giant cells, multiple refractile, needle-shaped, tubular, and occasionally curved unstained structures were seen (Figure 2C). These structures raised suspicion for foreign material deposition.
Photomicrograph showing mid and deep dermal granulomatous infiltrate (green arrows; H and E, 4x) (A). Suppurative granuloma (green square), hemosiderin deposition (yellow star), red blood cell extravasation (yellow arrow; H and E, 20x) (B). Foreign body giant cells which have engulfed- curved, spicule-like refractile, unstained structures; seen as empty spaces (yellow arrows) and tubular/quadrangular structures (green circle; H and E, 40x) (C). These structures represent foreign bodies.
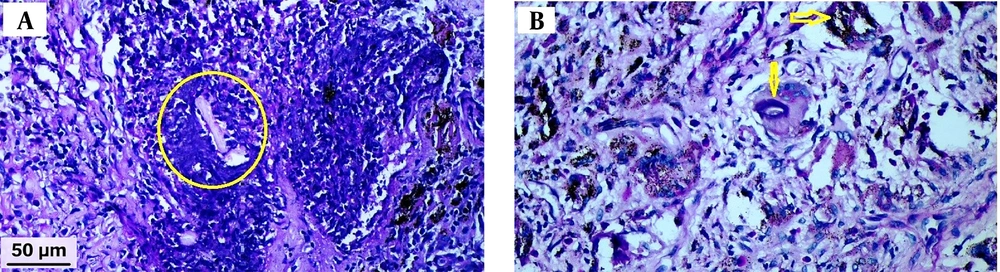
To investigate further, special histochemical stains were performed. Periodic acid-Schiff (PAS) (Figure 3A and B), Gomori methenamine silver (GMS), Ziehl-Neelsen (ZN), and Gram stains were all negative. Tissue cultures for bacteria, fungi, and mycobacteria also yielded no growth. These findings significantly reduced the likelihood of an infectious etiology.
Photomicrograph with periodic acid-Schiff (PAS) stain showed absence of magenta staining of the tubular structures (yellow circle) (A). The PAS stain did not show positivity in the curved empty-looking spaces within histiocytes (yellow arrows) (B). These findings are indicative of foreign body granuloma, ruling out fungal aetiology.
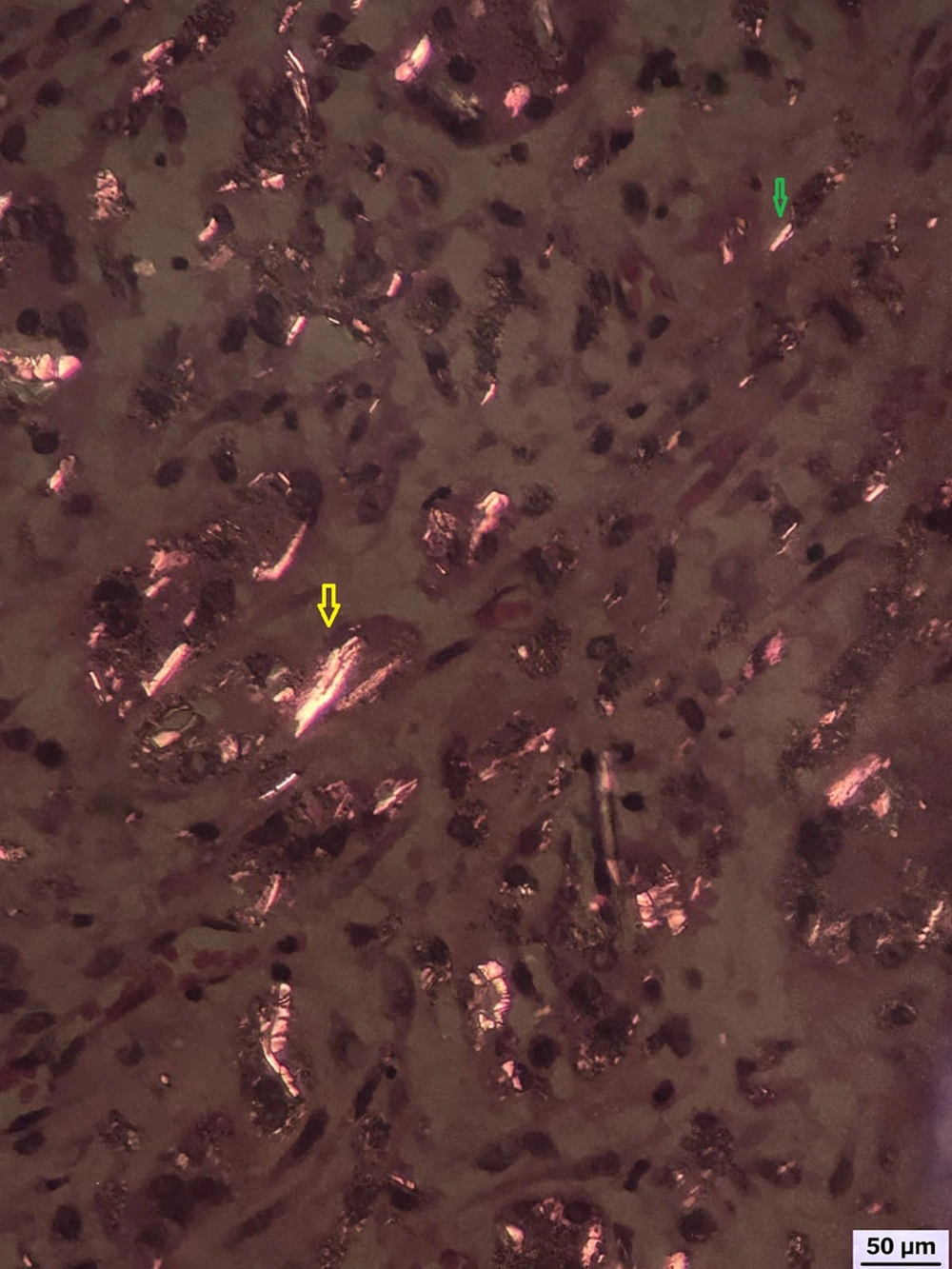
Subsequently, polarized light microscopy was employed to evaluate the refractile structures observed histologically. Under polarized light, numerous birefringent, needle-like, and rod-shaped structures were identified within histiocytes and multinucleated giant cells (Figure 4). These structures exhibited bright birefringence, characteristic of talc and silica particles, thereby confirming the diagnosis of a foreign body granulomatous reaction induced by adulterants introduced during IV heroin injection.
The patient was initiated on a combination of anti-inflammatory therapy. Oral doxycycline (100 mg once daily) was prescribed for its anti-inflammatory and antimicrobial properties. Colchicine (0.5 mg twice daily) was added for its efficacy in reducing neutrophil-mediated inflammation. Intralesional corticosteroids were administered to a few selected non-suppurative nodules to further reduce the granulomatous response, whereas the suppurative nodules and ulcers were treated with topical antibiotic (mupirocin 2% ointment) for a short duration of 7 days, to prevent secondary infection. The above treatment was planned for a period of approximately six months, with tailored therapeutic modifications during sequential interim follow-up visits. Concurrently, the patient continued to receive opioid de-addiction therapy, including psychosocial counseling and maintenance pharmacotherapy. Over the next four weeks, significant improvement was noted, with a reduction in tenderness, erythema, and nodule size. The ulcerated lesions began to heal with scarring. Unfortunately, the patient defaulted from follow-up after one month, limiting long-term assessment of therapeutic response.
3. Discussion
The cutaneous manifestations of IV drug use are multitudinous and often provide the first clues in identifying substance abuse in patients who may otherwise conceal their addiction. Common dermatologic signs include puncture marks, thrombosed veins, chronic ulcers, abscesses, and more complex presentations such as panniculitis or granulomatous lesions (1, 4). The practice of "skin popping", where substances are injected intradermally or subcutaneously due to inaccessible veins, often results in chronic inflammatory responses, scarring, and pigmentary changes (1, 2). In cases where IV access becomes difficult due to repeated trauma or thrombosis, patients may resort to using less accessible sites like the groin or neck, increasing the risk of serious complications (1).
Among the more elusive presentations in IV drug users are granulomatous reactions to injected foreign materials. Heroin is frequently adulterated with a wide array of substances to increase volume, mimic the consistency of pure heroin, or alter its appearance. These adulterants include both pharmacologically active agents such as quinine, procaine, and morphine, and inert fillers like talc, starch, silica, mannitol, and lactose (2). Many of these agents are poorly soluble and can precipitate in tissues, leading to chronic granulomatous inflammation. The clinical presentation may resemble infectious dermatoses, resulting in extensive workup and sometimes inappropriate antimicrobial therapy.
One particular diagnostic challenge is posed by lesions arranged in a sporotrichoid pattern — characterized by linear nodules along lymphatic channels, typically seen in infections such as sporotrichosis, atypical mycobacteriosis, and nocardiosis (3). Table 1 provides a detailed summary of infectious agents known to produce this pattern, highlighting their typical exposures, incubation periods, diagnostic methods, and treatments. In our patient, extensive investigations, including cultures and special stains, failed to isolate any pathogen. The presence of foreign body-type granulomas and a negative microbiologic workup shifted the diagnostic focus towards a non-infectious etiology.
| Etiology | Exposure/Region | Incubation | Clinical Features | Diagnosis | Treatment |
|---|---|---|---|---|---|
| Sporothrixschenckii | Soil, plants, and cats (tropics) | 1 - 12 (wk) | Painless ulcerated nodules | Sabouraud culture (25 - 32°C) | Itraconazole and SSKI |
| Mycobacterium marinum | Fish tanks and pools | 1 - 6 (wk) | Mildly tender ulcers/nodules | LJ or Middlebrook culture (30°C) | Rifampin + Ethambutol |
| Nocardiabrasiliensis | Soil and agriculture | 3 (d) - 6 (wk) | Nodules with purulent discharge | Routine culture | TMP-SMX and amikacin |
| Leishmaniabrasiliensis | Travel to endemic zones | 2 - 24 (wk) | Painless ulcers with indurated borders | Biopsy + NNN culture | Antimonials and amphotericin B |
| Francisellatularensis | Ticks, hunting, and cats | 1 - 6 (d) | Painful ulcers with necrosis | Serology | Gentamicin and streptomycin |
Infectious Causes of Sporotrichoid (Nodular Lymphangitis) Pattern (3)
Polarized light microscopy emerged as a decisive tool in this context. Various foreign substances exhibit distinct appearances under polarized light (5). Talc typically appears as white, quadrangular birefringent crystals, while silica presents as sharp, doubly refractile spicules (5-7). Starch shows a Maltese cross configuration, easily distinguishable from the linear or curved appearance of other particles (6). Notably, silicone is refractile but non-birefringent, allowing differentiation from silica or talc (8). These differences are summarized in Table 2. In our case, the detection of doubly refractile, needle-shaped spicules and tubular/quadrangular particles conclusively indicated the presence of silica and talc, respectively, corroborating the diagnosis of foreign body granulomatous dermatitis.
| Foreign Material | Appearance Under Polarized Light |
|---|---|
| Talc | Oval/quadrangular birefringent particles |
| Silica/glass | Sharp, doubly refractile, and birefringent needle-like structures |
| Starch | Maltese cross pattern |
| Wood splinters | Honeycomb or stepladder pattern |
| Silicone | Refractile but non-birefringent vacuoles |
Polarized Light Microscopic Appearance of Various Foreign Bodies (6)
Heroin has rarely been reported to crystallize in the renal tubules of patients with metabolic alkalosis, leading to heroin-induced nephropathy (9). These crystals have been labeled either as fluffy deposits within the renal tubules or as broomstick-shaped crystals in the urinary sediment of opioid abusers (9). In our case, the foreign material was identified as adulterants rather than heroin itself.
Treatment in such a clinical scenario is complex. While surgical excision is effective for localized granulomas containing retained foreign material, it may not be practical for widespread lesions (1, 5). Anti-inflammatory agents such as colchicine and minocycline are commonly used to modulate the immune response. Colchicine, in particular, reduces neutrophil chemotaxis and has proven efficacy in conditions characterized by granulomatous inflammation (5). Colchicine (0.5 mg, orally twice a day) was one of the systemic drugs used in our case for its anti-inflammatory properties.
Doxycycline, as used in our case, serves the dual role of antimicrobial and anti-inflammatory agent. We utilized both the broad-spectrum antimicrobial and anti-inflammatory actions of doxycycline. Some of the nodules were suppurative (albeit culture-negative), and the possibility of secondary pyogenic infections could not be clinically ruled out — particularly in the context of IV drug abuse, where habits such as non-sterile injection practices and needle sharing predispose patients to skin and soft tissue infections caused by organisms like Staphylococcus aureus and group A Streptococci, among others (10). Additionally, doxycycline’s anti-inflammatory action can be attributed to its well-established ability to suppress inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-1 (IL-1), interleukin-6 (IL-6), and interleukin-8 (IL-8), thereby reducing both granulomatous and neutrophilic inflammatory responses (11).
Although the suppurative nodules were microbiologically sterile, topical antibiotic therapy (mupirocin 2% ointment) was administered for a short duration (7-day course) to treat the ulcers and suppurative nodules, with the intent to prevent or cover potential secondary pyogenic infections caused by Staphylococci and Streptococci — the most common cutaneous invaders in people who inject drugs (10). The choice of doxycycline for the aforementioned dual purpose may be particularly useful in uncertain or mixed presentations, such as those seen in IV drug users, where occult bacterial colonization or superinfection cannot be entirely excluded. Other anti-inflammatory agents, such as NSAIDs or systemic steroids, do not provide this dual benefit, and the latter may mask signs of potential infection. In cases with localized, non-suppurative nodules, intralesional corticosteroids may be beneficial in reducing the inflammatory milieu (5). Topical calcineurin inhibitors such as tacrolimus may be employed in milder cases or as adjunctive therapy. Other agents like allopurinol and isotretinoin have been reported anecdotally for their immunomodulatory benefits in foreign body reactions. Ultimately, a multimodal approach tailored to lesion severity and patient compliance provides the best therapeutic outcomes.
In our patient, we deployed tablet doxycycline and colchicine along with intralesional steroids (in a few of the lesions), albeit with partial relief. This case highlights a rare yet clinically significant presentation of foreign body granulomas mimicking sporotrichoid lymphangitis in an IV heroin abuser. The key diagnostic challenge lay in distinguishing these lesions from infectious etiologies, a task made possible by the use of polarized light microscopy. The detection of birefringent particles characteristic of adulterants such as talc and silica was pivotal in establishing the correct diagnosis.
3.1. Conclusions
This case underscores the critical need for heightened clinical awareness of foreign body granulomas induced by adulterants in IV heroin users, particularly when lesions mimic classic infectious patterns such as sporotrichoid nodular lymphangitis. The linear distribution of nodulo-ulcerative lesions along the course of superficial veins may closely resemble infections like sporotrichosis or atypical mycobacterial lymphangitis, potentially leading to misdiagnosis. Histopathology and special stain analysis remain central to diagnosis, helping to rule out clinical similes. The use of polarized light microscopy is pivotal in distinguishing among different foreign materials by recognizing their architecture and birefringence. Timely recognition of this entity not only prevents unnecessary antimicrobial use but also guides appropriate anti-inflammatory therapy and facilitates essential de-addiction support.