1. Introduction
Dowling-Degos disease (DDD) is a rare autosomal dominant inherited genodermatosis with variable penetrance and female preponderance (1, 2). It is clinically characterized by flexural brown pigmented reticulate macules, comedo-like papules on the back and neck, as well as pitted perioral or facial scars (3).
There are some reports in the literatures of the coexistence of DDD with other diseases, including adenitissuppurativa (HS), squamous cell carcinomas (4, 5), seborrheic keratosis (6), reticulate acropigmentation of kitamura (7), multiple epidermal cysts (8), multiple keratoacaonthomas (9), and Darier disease (10).
In this article we report a rare association of DDD and HS, which has not been reported in the Iranian literature to date, while also discussing an effective new treatment for DDD.
2. Case Report
In September 2015, a 42-year-old woman was presented to our department of Rasoul Akram hospital, complaining of gradually progressive hyper-pigmented lesions of the face and body. Brownish macules first appeared on her face 1 year prior to her presentation, and several months later, some lesions became distributed within the intramammary, groins, and axillary sites. Furthermore, abscess-like lesions were reported over the breasts (Figures 1 - 3). The patient initially went to the surgeon for these lesions, and after performing a core needle biopsy, the surgeon made the diagnosis of severe acute suppurative inflammation (abscess-formation). Following this diagnosis, the patient received treatment in the form of oral antibiotics, however, with no improvement. A second core needle biopsy was performed along with an axillary lymph node biopsy, however, no significant pathologic changes were noted (Figure 4).
The patient reported similar facial lesions on her mother and 1 sister but reported the absence of such lesions on her father, other siblings, as well as her 6-year-old daughter.
No history of consanguinity was reported.
A cutaneous physical examination of the patient revealed that she had skin type 4 in Fitzpatric scale, with numerous small, deeply dark macules of 5 – 10 mm in diameters, round or oval in shape, and with a homogeneous pigmentation. These macules were observed in a reticulate pattern over the face and flexoral sites (Figure 1). Pitted scars of sizes varying from 1 - 3 mm were also seen in the perioral and cheeks (Figure 2). In addition, atrophic breast scars and double comedone were observed.
A general physical examination was normal.
One specimen was taken from a comedo-like lesion and a 2nd specimen was taken from a hyper pigmented macule on the intermammary fold skin.
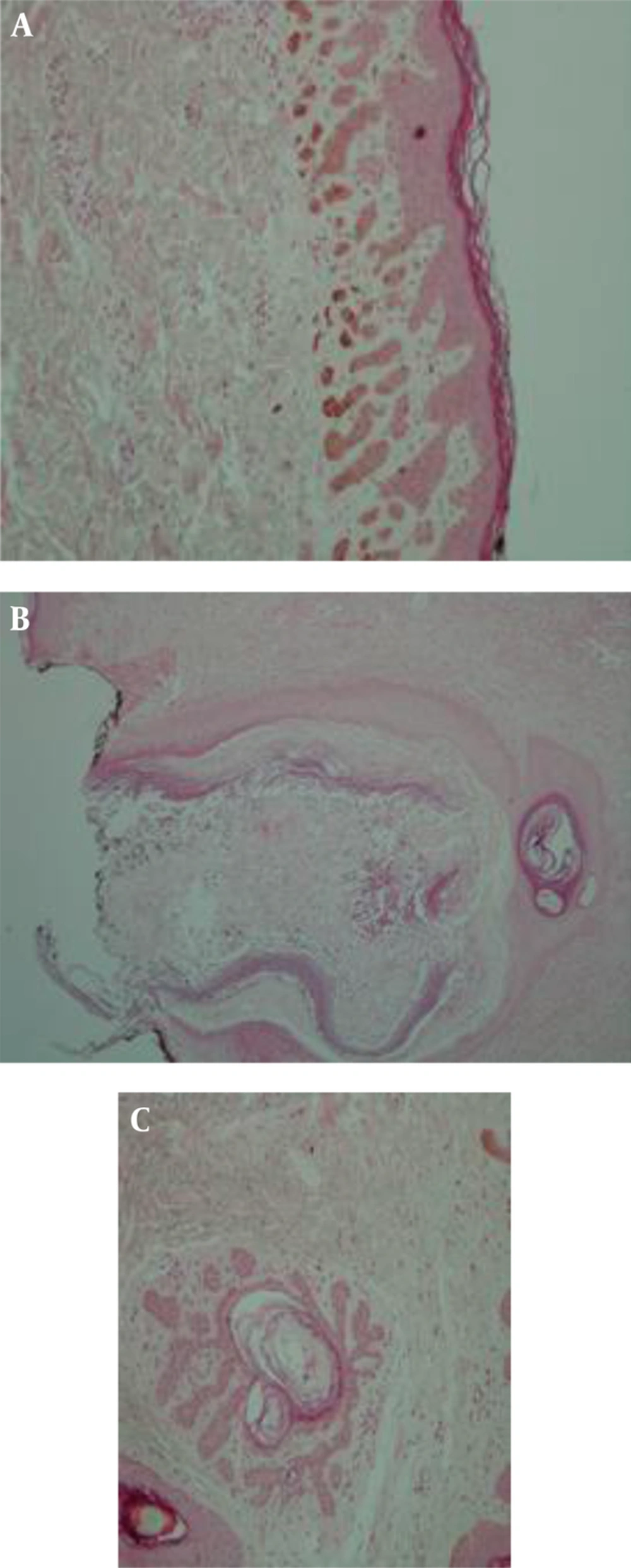
A histopathologic examination showed filiform epithelial strands growing down from the epithelium. In addition, diffuse basal layer hyperpigmentation was observed, which resembled the histology of the reticular seborrheic keratosis, and also dilated hair follicles containing lamellar keratinous material with foreign body type giant cell reaction as well as mixed inflammation with neutrophilic inflammation resembling abscess-like lesions.
An antler-like pattern in the pathology of skin resulted from thin epithelial strands extending into the dermis from the hair follicles.
Perivascular inflammation was observed in the upper dermis (Figure 3).
Laboratory tests, including CBC, FBS, renal, liver, and thyroid function tests were each reported as normal.
This patient met the criteria of Dowling-Degos-disease according to all of the clinical and histopathological findings, although no confirming molecular genetics study could be conducted due to the lack of facilities.
The patient suffered from hyperpigmented lesions but refused topical therapy. Despite the usefulness of topical tretinoin, it was decided to place the patient on an oral isotretinoin regimen.
A total of 20 days after beginning the oral isotretinoin regimen, most of the facial hyperpigmented lesions had disappeared and the patient continued this treatment.
After 90 days, 90% of the patient's facial pigmented lesions and scars had disappeared, as is evident from the photographs. However, the lesions of the flexural sites did not respond well to this new treatment.
3. Discussion
DDD is a rare autosomal dominant disease with various penetration characterized by benign reticular pigmentations of flexural sites. It was first described by Behc et al. in 1932, as a variant of acanthosis nigricans (4). Dowling (1938) and Degos (1954) were the first to introduce the aspect of reticulate pigmentation called dark dot disease (11). Jones and Grice reviewed related literatures and suggested the name DDD (12). In 2006, Betz et al. illustrated that mutations of keratin 5 is responsible for pigmentary changes. Keratin 5 is a component of the intermediate filament in the basal layer of the keratinocytes and plays a role in the uptake and distribution of melanosomes in keratinocytes. The mutation of keratin 5 is also seen in Epithermolysis Bullosa simplex-mottled pigmentation (13).
Diagnosis of DDD is based on clinicopathologic data. The clinical criteria include: reticular hyper pigmentation of the flexural sites, Comedo-like papules on the back and neck, as well as Perioral pitted scars.
The histopathologic features showed: hyperpigmentation of the basal layer, thin epithelium with filliform elongated strands extending down to the superfacial dermis, horn cyst formations, and antler-like patterns (4).
According to clinical features, the differential diagnoses include multiple entities. Disorders with reticular and mottled pigmentation contain: acropigmentation of kitamura, Galli-Galli disease,acropigmentation of Dohi, acanthosis nigricans, and Haber disease. Most of the above is demonstrated with other clinical and histopathologic features (14).
The relationship between DDD and other disorders have been reported in some papers. This article reports a patient who had DDD in association with hydradenitis supprativa. The patient mentioned a few painful lesions with discharging pus in axillary and inframammary sites. Within that neutrophilic inflammation were observed some keratin flakes, which resembled abscess-like lesions.
There is no available evidence of association or co-occurrence between the DDD and hydradenitis supprativa or similar underlying pathogenesis.
No completely effective treatment was established. In addition to topical therapy like hydroquinone, adapalene, and tretinoin, different modalities were reviewed, including fractional Er:YAG laser, PUVA therapy and intense pulsed light (IPL). Additionally, oral retinoid (Isotretinoin 20 mg daily) was started as a novel management strategy; however, a thorough evaluation of the efficacy and safety of this treatment option requires additional studies involving numerous patients.