1. Introduction
Self - healing juvenile cutaneous mucinosis (SHJCM) is a rare disease in dermatology, characterized by sudden onset of papules and nodules located primarily on the face and peri - articular areas of juvenile patients (1). It was described by Colomb (2) and Bonerandi (3) and in the 2 following decades, many other similar cases have been reported (4-12). Cutaneous mucinosis has various clinical types, such as SHJCM and congenital forms (13). In previous studies, different types of SHJCM, such as the nodular type (14-16), focal type (6, 17), familial type (10), recurrent type (18) with different lesion site presentation (1, 15), have been report. Proper approach to this disorder and its mimickers have been presented (3, 19, 20). Rarely, there has been recognized cases of self - healing cutaneous mucinosis in adult patients (18, 21, 22). The association between self - healing cutaneous mucinosis and underlying disorders, like nephroblastoma and epilepsy, has been proposed (5, 21). Approximately 20 case studies have been written about SHJCM (14, 23). The current patient had 3 major clinical presentations of cutaneous mucinosis, including nodular and papular lesions, and periorbital edema. Hard nodular lesions are slowly converted to the superficial soft papular lesions after alcohol cessation. The current report describes a new developmental pattern of cutaneous mucinosis lesions in an adult patient during a 3 - year follow - up with alcohol consumption as one of the probable underlying associations or triggering factors in the setting of self - healing cutaneous mucinosis.
2. Case Presentation
A 23 - year - old male referred with 2 months history of changes in facial shape and severe itching of the body, in June, 2014. An early skin examination revealed 2 types of cutaneous lesions in addition to periorbital swelling: hard asymptomatic nodules located around large joints like the knee, elbows, and wrist. Face (bridge of the nose, forehead, and temples), back, and flanks were also involved (Figures 1 and 2). The second lesions were numerous, extremely pruritus, 2 to 3 mm, firm and waxy, closely spaced papules, which were locally distributed. The most common sites of involvement were the scalp, upper trunk, and fingers. The overlaying skin was shiny, hyperpigmented, and indurated (Figure 3).
Hair loss in the affected area of the scalp was prominent (Figure 4). Systemic examination was normal. He had a history of alcohol consumption before skin lesions. A punch biopsy was performed from a papular lesion as well as a deep excisional biopsy from a nodular lesion of the forearm.
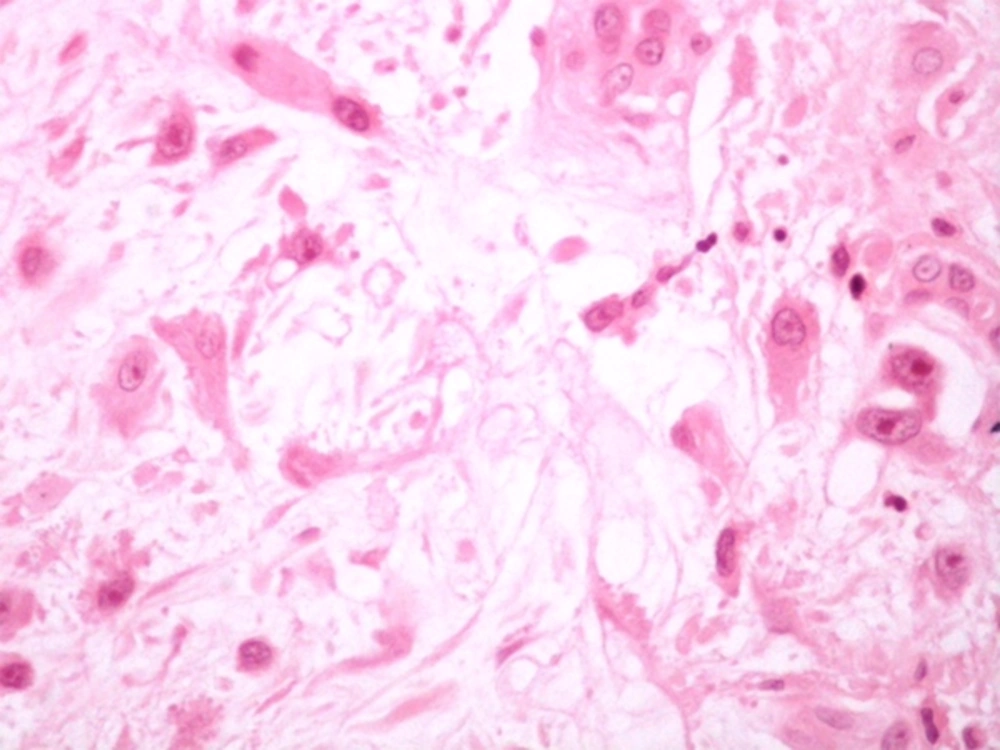
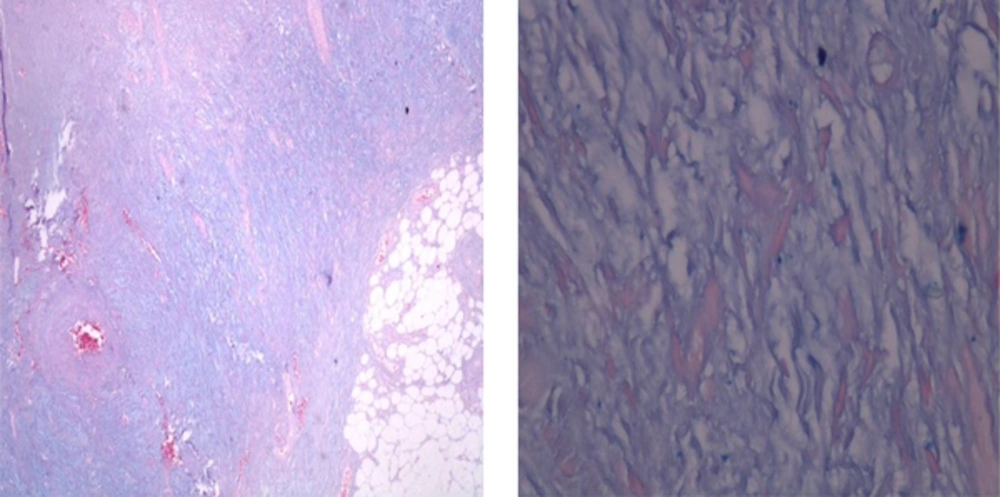
Histopathologic features of the papular lesion revealed focal epidermal parakeratosis and accumulation of mucinous material in the upper and mid portion of the dermis, and also a mild increase in fibroblast cells (Figure 5). Nodular lesion in pathologic examination showed multiple areas of mucin deposition in deep dermis and increased number of fibroblast cells with ganglion - like features (Figure 6). Atypia and mitoses were not found. Mild perivascular infiltration of chronic inflammatory cells was also evident. The deposited material in the 2 samples were positively stained by alcian blue at pH 2.5 for mucin and stained negatively for amyloid on congo - red stain (Figure 7).
To rule out probable underling disorders associated with mucinosis, a baseline lab evaluation was conducted. A complete blood count, liver and renal function tests, thyroid stimulating hormone, serology of viral hepatitis, HIV, serum and urine protein electrophoresis, erythrocyte sedimentation rate, C - reactive protein, antinuclear antibodies and X - ray of the wrist (for the rule out calcium deposition disorders) were done with all results being normal.
Based on clinical features and histopathologic study, diagnosis of cutaneous mucinosis was confirmed. At first, Isotretinoin 20 mg daily was prescribed for the patient yet the therapy was interrupted after 3 weeks due to drug side effects. The patient was visited 3 months later. In the follow - up sessions, new nodular lesions were developing on his back yet not on the other areas. The newly formed lesions were more superficial and smaller than previous lesions. Old papular lesions disappeared gradually. After 2 years, in May 2016, all skin lesions were completely healed without any therapy. It should be noted that the patient stopped alcohol consumption prior to improvement.
3. Discussion
Self - healing cutaneous mucinosis is a rare disorder, which commonly appears in younger patients as the juvenile type (from 13 months to 15 years old), yet it could appear at any age (rarely after 20 years old as the reported case) (18, 20-22, 24). The skin manifestations are mainly characterized by sudden onset of asymptomatic papules and nodules on different cutaneous locations; mostly on the face, peri - articular areas, and the abdomen (15). One of the main unique features of SHJCM is complete resolution within weeks to months, although in some cases, the course may be longer (16).
Another interesting feature of this disorder is an association with extra - cutaneous manifestations, such as peripheral painful polyarthritis or signs of connective tissue disorders or autoimmune disease; thus some previous reports have recommended conducting antinuclear antibodies and complete blood cell counts in those with evidence of these accompanying associations (25). In most cases, the predominant histopathologic features are edema of the papillary and reticular dermis along with collagen bundles separation (due to mucin deposition), slightly increased number of fibroblast cells, and a mild perivascular infiltrate. Various reports of different histopathological features of SHJCM have been evident. In a report by Wadee et al. (5), mucin deposition in the mid and deep portion of reticular dermis, arborizing thin - walled vessels, and prominent spindle - shaped fibroblasts were exhibited. Cowen et al. (26) reported fibroblast cells in stellate, spindled shape, rhabdoid or strap - like figures. It seems that the differentiation of SHJCM from proliferative fasciitis/nodular fasciitis is critical (8). Despite various histological features, the diagnosis of SHJCM is mainly based on clinical presentations like sudden onset of papules and nodules located primarily on the face and peri - articular areas, which may disappear without any special treatment. As a rule, SHJCM may be differentiated from other forms of cutaneous mucinosis by some specific characteristics, including its early age of onset, the lack of systemic symptoms, spontaneous resolution, and the absence of dysglobulinemia or thyroid dysfunction (9). Until now, the nature of the disorder has remained unclear. It has been suggested that the ethological source of the disorder may be altered fibroblast cells function, which is triggered by viral infections or immune reactions (19).
In the current case, lesions developed after alcohol consumption and healed once stopped, so alcohol could be considered as a new triggering factor. The most prominent clinical feature of the current patient was slow conversion of hard nodular lesions to the superficial soft papular lesions. There were not any systemic disturbances or viral infection to be considered as a source of the disease onset. As shown in other cases, SHJCM may not require any therapeutic interventions due to its self - limiting nature (3, 19, 27-29).
Although there are various successful therapeutic modalities for cutaneous mucinosis (30-35) yet in probable cases of self - healing cutaneous mucinosis, the physician should prevent unnecessary diagnostic tests or aggressive therapies.