1. Introduction
2. Case Presentation
A 57-year-old female referred to the outpatient clinic with multiple asymptomatic to painful, erythematous, rubbery dermal nodules with smooth surfaces on her face and left arm. These lesions were 0.5 - 2 cm and developed when the patient was 25 years old (Figure 1). Size and number of the lesions gradually increased. She had a history of severe menorrhagia when she was 30 years old, which resulted in hysterectomy in her 40s. Also she had history of hypothyroidism, hypertension, hyperlipidemia, and renal stone. She was on atorvastatin, methoral, and levothyroxine therapy.
She had three children; two daughters and one son. Her son was 37 years old and had similar lesions on similar sites in a clustered pattern from four years ago. Her older daughter was 34 and had only multiple uterine leiomyomas and severe menorrhagia. Her younger daughter was 32 and had multiple cutaneous lesions on mid-chest from six years ago with a history of severe menorrhagia. The current study patient had a cousin with similar problems. She had no history of renal carcinoma in her family.
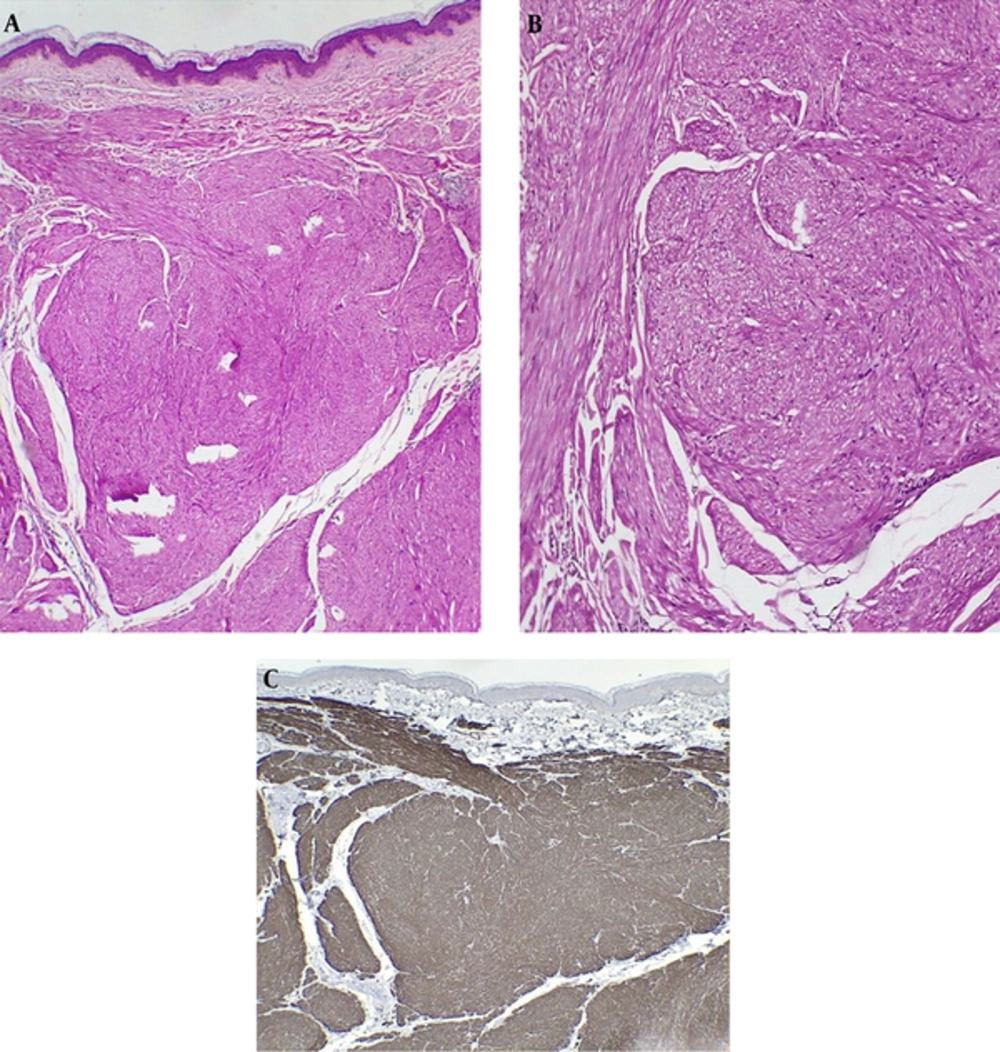
An incisional biopsy was performed from facial skin lesions. Histopathologic evaluations showed a poorly demarcated neoplastic proliferation consisted of interlacing bundles of bland smooth muscle fibers, which had smooth muscle actin (SMA) positivity in immunohistochemistry. These fibers surrounded follicular structures and sweat glands; therefore, diagnosis of piloleiomyoma was proposed (Figure 2). Ultrasound imaging showed two simple cysts (22 and 7 mm) in the left kidney and a liver hemangioma measured 21 mm in diameter.
Laboratory evaluations including complete blood count, erythrocyte sedimentation rate, and renal function tests were within normal limits. Diagnosis of Reed syndrome was made for this family. Therefore, all the affected family members were screened by renal ultrasound for possible renal cell carcinoma. Gabapentin capsule 100 mg daily was administered for the current study case to relieve occasional painful episodes of her lesions.
3. Discussion
Cutaneous leiomyoma is a benign skin tumor originated from dermal smooth muscles. Three subtypes of this tumor are described as follows: piloleiomyoma (originated from arrector pili muscles), leiomyoma of the external genitalia (originated from vulvar and mammary smooth muscles), and angioleiomyoma (originated from dermal blood vessels). The most common subtype is angioleiomyoma followed by piloleiomyoma (1, 2).
Piloleiomyoma is a skin-colored, pink or brown, asymptomatic to tender nodule usually observed on the extremities. It could be solitary or multiple with a clustered or dermatomal pattern. These lesions are usually observed in patients aged 10 to 30 years (1, 3).
Clinical differential diagnoses of leiomyoma are other skin tumors that could be painful such as spiradenoma, glomus tumor, fibrous or neural tumors (3, 4). Histopathologic evaluation differentiates leiomyoma from other tumors.
Total excision is the best method for the solitary lesion, but for multiple lesions some medications such as nifedipine, gabapentin, and doxazosin or CO2 laser irradiation could be useful (1, 3).
Reed syndrome is a syndrome with three clinical components as follows: (1) multiple cutaneous leiomyomas (mainly piloleiomyoma), (2) uterine leiomyomas or leiomyosarcomas with abdominal pain, menorrhagia, dysmenorrhea and sometimes infertility, and (3) increased risk of papillary renal cell carcinoma (3-5). It is caused by heterozygous mutation in fumarate hydratase (FH) gene, an enzyme involved in mitochondrial Krebs cycle. This gene is located on chromosome 1q42 (4-6). This mutation is related to papillary renal cell carcinoma type 2, with a high mortality in young age (4, 7).
There were signs of this syndrome in several members of this family, similar to the report by Mandal et al. (3), and similar to the current case report they did not report renal cell carcinoma. The relationship between renal cell carcinoma and multiple cutaneous and uterine leiomyomatosis is not high in studies; Alem et al. (7), reported this rate at 2% in 46 cases, Toro et al. (8), reported 6% in 35 patients, Martinez-Mir et al. (9), reported 0% in five patients and the current study observed no signs of malignancy in the case.
Screening is recommended for the patients with multiple leiomyomas including complete history and clinical examination, skin biopsy and histopathologic evaluation, periodic renal and pelvic ultrasound, complete blood count and metabolic panel, urine analysis, genetic analysis for mutation in FH gene and referring the patient to a gynecologist and nephrologist. The pelvic and renal ultrasound or computed tomography (CT) imaging should be repeated every two years. The family members should be completely examined and pelvic and renal ultrasound should be done if required (1, 4).
3.1. Conclusions
Cutaneous leiomyoma is a benign skin tumor, but multiple cutaneous leiomyomas could be considered as a sign of internal involvements such as uterine leiomyosarcoma or renal cell carcinoma, which requires more evaluations (1, 2).