1. Introduction
Pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH) is a rare hereditary autoinflammatory syndrome (1, 2). It is generally due to mutations in the PSTPIP1 gene and initiated in first years of life; but sometimes may be seen in older ages and after some causes such as surgical procedures (2, 3).
Presence of suppurative hidradenitis and other inflammatory disease such as acne has been reported in different studies (4-7). Treatment is generally with immunosuppressants and biological drugs such as infliximab (8, 9). To the best of our knowledge, there is no reported case of PASH syndrome from Iran and with this clinical manifestation.
2. Case Presentation
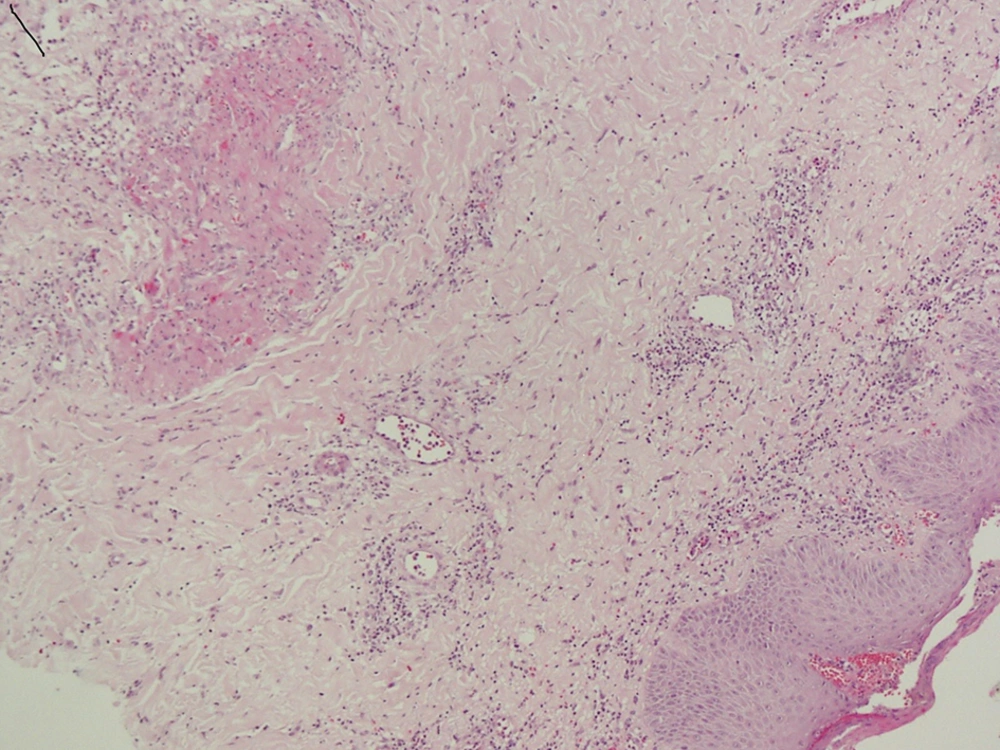
A 44-year-old obese female presented with ulcers in leg area since 8 months before to the dermatology clinic of Bahman hospital. Dermatohistopathology of a biopsy specimen from the ulcer revealed pyoderma gangrenosum (PG). Her skin manifestation was first suppurative hidradenitis when she was 16 years old, (Figures 1 - 3) then acne and now PG.
She had history of anal fistula and constipation when she was 16 years old that underwent surgery. History of acne, hypothyroidism and abnormal menstrual cycles with polycystic ovaries was present when she was 28 that had undergone treatment. There was a mass in the pituitary gland when she was in 38 that was diagnosed as prolactinoma. Isotretinoin 40 mg daily and 30 mg prednisolone was prescribed for about 6 months. She was followed for 3 years, and no recurrence has occurred.
3. Discussion
PASH syndrome is one of the newly described dermatological disorders (10, 11). It is stated in previous reports that the level of pro-inflammatory markers such as cytokines and interleukins increased in PASH syndrome (7). We could not assess these biological markers in the reported patient, though. The serum levels of the pro-inflammatory cytokines, including TNF-α, IL-1β, and IL-17 are normal in this syndrome (7). On the other hand, the importance of inflammation in pathophysiology of PASH syndrome as an auto-inflammatory pustular neutrophilic disease has been shown (12). Different diseases with disordered immunity regulations are accompanied with PASH syndrome.
Braun-Falco et al. presented two cases of PASH. First one was a man with severe cystic acne lesions and draining sinuses and PG that received isotretretinoin and the IL-1 receptor antagonist anakinra (2) .The other study reported a patient with multiple large ulcers with history of severe cystic acne. The combination of low-dose prednisolone and azathioprine was prescribed for a year and the ulcer´s size decreased significantly (2).
In another study GMA (Granulocyte and Monocyte Adsorption Apheresis) was prescribed for a patient with this syndrome for 10 consecutive weeks. After 2 sessions, the ulcers were reduced (13).
In this study we have reported a patient with PASH syndrome and hormonal problems hypothyroidism, abnormal menstrual cycles and obesity that wasn’t reported in previous cases of PASH. Treatments such as anti-tumor necrosis alpha antibodies, anti-IL-1 receptor antibodies, cyclosporine and systemic steroids have also been reported (14). One study showed complete remission with the infliximab, cyclosporine and dapsone (8). Mizutani et al. showed that GMA was effective for treating PASH syndrome (13). In our study, we prescribed low dose prednisolone(30 mg and tapered in 6 months) and systemic isotretinoin (40 mg as starting dose and tapered in 6 months). It should be noted that no any sign of remission and recurrence was seen in this case 2 years after stopping drugs.
Finally, according to the reported case in this study it may be concluded that PASH syndrome despite rarity should be considered as a possible cause of complex skin manifestations. Further studies are being performed on the reported patient to achieve a better presentation of this disease and report the case in further papers especially with focus on laboratory and therapeutic information.