1. Introduction
Darier disease is an autosomal dominant hereditary disease. The sex incidence is equal (1). This disease was first described by Darier and White in 1889. In 1993, the first case with vulvar lesion was reported in a 5 year old girl (2). The main organ that is involved is skin. Skin presentation includes warty papules on trunk, face and inguinal region. Mucous membranes are affected in 15% of patients (3). Female genital tract involvement is uncommon. Pathologic features of a darier lesion include suprabasal clefts in the epithelium, with acantholysis and dyskeratotic cells presented as “corps ronds” and “corps grains “in the granular layer.w). We present a case of vulvar involvement.
2. Case Presentation
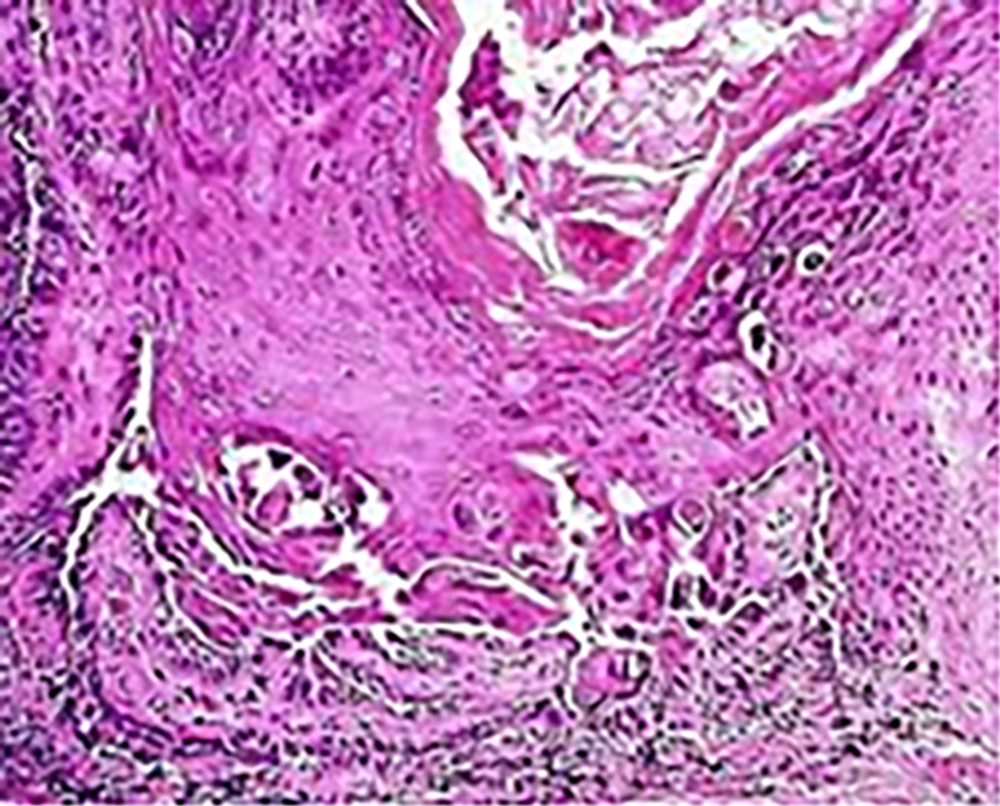
A 59-year-old female with history of hyperkeratotic papule on labia major and minor since three months ago (Figure 1). She complains about pruritus, dysuria and progressive dyspareunia. Sexually transmitted disease and autoimmune screens were negative .In gynecology examination by gynecologist, abnormal Pap smear showed features consistent with a low grade squamous intraepithelial lesion. The skin and cervix biopsy was obtained with differential diagnosis of genital wart. Cervicovaginal smear report was: ASC-USA (atypical typical squamous cells of undetermined significance). The pathology report of this disease include acantholytic dyskeratotic pattern consistent with Darier ( Figure 2).
In physical examination, mucous membrane and nails were normal.
Primary laboratory analysis of cell blood count, liver enzymes and kidney function were normal, and the patient’stest of transferable infectious disease such as hepatitis B, C and HIV were normal. Acitretin tablet with dose of 25 daily was prescribed for patient about 6 months. Topical clotrimazol, emollient and bethametasone cream were applied for extragenital lesions. Symptoms of patient improved completely after treatment and in 3 years follow up, no recurrence was seen.
3. Discussion
In approximately 70% of patients, the disease begins between the ages of 6 and 20 years, with a peak onset during puberty (ages 11 - 15 years). The primary lesions are keratotic, sometimes crusted, red to brown papules, which develop preferentially in a “seborrheic” distribution involving the trunk (4). The lesions tend to become confluent and may form papillomatous masses. Most patients complain of moderate itching. Equally distressing are the appearance and the odor, which can lead to social isolation. The prevalence of oral manifestations has varied in different cohorts. In one study, painless whitish papules of varying severity were present in 50% of patients with Darier disease; the palate was the most common site of involvement (3, 4). Involvement of the female genital tract by Darier’s disease is rare. In previous studies, they reported a 39-year-old woman with abnormal Pap smear by Darier’s disease. They showed, the correct interpretation of cytologic findings is not possible and a low grade squamous intraepithelial lesion cannot be ruled out (5). ASCUS is a finding of Pap smear indicating that some flat (squamous) cells look unusual and may or may not be pre-malignant. It is advised that ASCUS should not be ignored and requires more attention.
In another study, it was reported that Darier disease can mimic genital warts (6). They suggested all dermatologist and gynecologists to consider Darier’s as a differential diagnosis of warts. In our study, we report a patient with a verrucous papule like wart but with pruritus and dyspareunia. The lesions were biopsied. After confirming Darier disease and receiving treatment, all symptom and signs of patient healed. Atypical location, age and clinical manifestation of disease can lead to misdiagnosis and mismanagement of disease.