1. Background
Helicobacter pylori (H. pylori) is a Gram-negative bacillus that causes gastritis and ulceration (1). H. pylori predisposes to gastric cancer, which is the second most common cause of death due to cancers (1). The pathogenesis of this microorganism thought to have multifactorial etiology (2). Bacterial virulence factors, host genotypes, immune response, and environmental factors are thought to play a role in the pathogenesis of this microorganism (2). Several reports have linked H. pylori to a variety of extra-gastric diseases (3). These include ischemic heart disease, skin diseases such as idiopathic urticaria, autoimmune thyroiditis, thrombocytopenic purpura, iron deficiency anemia in pediatrics, Raynaud’s phenomenon, scleroderma, migraine, and Guillain-Barre’ syndrome (3). The exact mechanism behind this is not fully understood. However, activation of the cascade of coagulation, stimulation of atherosclerosis formation, and antigenic mimicry between the microorganism and host epitopes have been proposed as hypothetical mechanisms explaining the relationship between H. pylori and extra-gastric disorders (3).
Chronic urticaria is a dermatological disorder that is characterized by widespread, temporary wheals that occur on a daily basis for at least six weeks (4). Several causes have been proposed to explain chronic urticarial; this includes infections including bacteria, viral, fungal, or protozoan infection. Additionally, auto-immune antibodies are detected in about 50% of the cases suggesting inflammatory mechanisms as an etiology of this disorder (4). Several studies showed a possible relationship between H. pylori infection and chronic urticarial; however, such a relationship remains controversial. H. pylori infection was studied thoroughly in our locality (5-7).
2. Objectives
No study has been conducted investigating the association of H. pylori with chronic urticaria in Duhok city. Therefore, this study was designed to investigate the association between infection with this microorganism and chronic urticaria.
3. Methods
3.1. Study Design
This case control study was carried out between June 2018 and March 2019. The study was conducted at the Dermatology Consultation Unit, Azadi Teaching Hospital, Duhok, Iraq. During the survey, enrolled subjects were interviewed using a standardized questionnaire information that included age, gender, and address. The questionnaire composed of questions regarding demographical data about patients including age, gender, place of residency, and family members number (Appendix 1 in Supplementary File).
3.2. Studied Population
During the study period, all subjects who were presented to the dermatology unit with chronic urticaria were enrolled in the study. The inclusion criteria included patients with chronic urticaria, as defined as temporary wheals that occur on a daily base for at least six weeks, and agreed to be involved in the study by signing informed consent. Patients with acute urticaria, inducible (physical) urticaria, who received antibiotics in the prior two weeks, and who did not agree to sign the consent were excluded.
3.3. ELISA
A 5cc syringe and needle were used to obtain 5 mL of blood from each subject. Then, the blood samples were centrifuged at 1500 rpm for 3 min to obtain the serum. The HCV AB (fourth generation) with 100% sensitivity and specificity and the hepatitis B-specific HBsAg with a 100% sensitivity and 97.5% specificity were studied by commercial DIA.PRO diagnostic Bioprobes ELISA kit (Italy), following the manufacturer’s instruction. Anti-H. pylori IgG ELISA (EUROIMMUN Germany) was utilized for the detection of the presence of H. pylori-specific IgG, according to the manufacturer’s instructions. The recommended cut-off values were used.
3.4. Statistics
Linear regression was used to explore such a relationship between variables and outcomes when the variables were continuous while chi-square test was used for categorical data. P value of < 0.05 value was considered as significant.
3.5. Ethics
This project and the consent were approved by the Ethics Committee of the College of Medicine, University of Duhok. Informed consent was obtained from all recruited subjects.
4. Results
4.1. Characteristics of Patients
During the study period, 49 patients with chronic urticaria were recruited in the study. Among the recruited samples, 10/49 (20.4%) were male. The average age of participants was 36.5 ± 11 years. All patients were examined for HBsAg and HCV-AB. All patients were negative for these two viral infections. Complete blood count was normal in 47/49 (95.9%) of the recruited samples. Thyroid function was normal in all patients. Additionally, during the study period, 95 subjects were recruited as a control. Among them, 30/95 (31.6%) were male and the average age of the control group was 32.6 ± 11.4 years.
4.2. H. pylori Positivity
The overall H. pylori positivity was 106/144 (73.6%). Then, H. pylori positivity was compared between the patients’ group and control group. The positivity was 38/49 (77.6%) positive for the patients’ group versus 70/95 (73.7%) for the control group (P = 0.7; OR = 1.16; CI = 0.53 - 2.57). Then, we studied the association between H. pylori positivity and risk factors. No associations were found between H. pylori positivity and age, gender, and residency. A significant association was found between family members number and H. pylori positivity (P = 0.04; OR = 1.15; CI = 1 - 1.3) (Table 1). In addition, the prevalence of H. pylori positivity was higher in subjects residing in the city compared to rural areas (76.3% for city vs. 50.9% for rural areas, P = 0.013).
| Factors | H. pylori Positive | H. pylori Negative | P Value | Odd Ratio | Confidence Interval |
|---|---|---|---|---|---|
| Family number | 7.3 ± 3 | 7.2 ± 3 | 0.04 | 1.15 | 1.01 - 1.32 |
| Age | 33.8 ± 11.3 | 34 ± 11.4 | 0.65 | 1 | 0.97 - 1.04 |
| Gender | 0.15 | 0.56 | 0.25 - 1.23 | ||
| Female | 24/38 (63.2%) | 80/106 (75.4%) | |||
| Male | 14/38 (36.8%) | 26/106 (24.5%) | |||
| Residency | 0.013 | 0.36 | 0.16 - 0.81 | ||
| City | 29/38 (76.3%) | 54/106 (50.9%) | |||
| Rural | 9/38 (23.7%) | 52/106 (49.1%) |
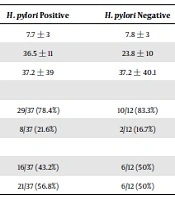
Then, the associations between H. pylori and risk factors were studied within the patients’ group. No association was found between H. pylori and age, gender, family member number, or the duration of urticaria (Table 2).
| Factors | H. pylori Positive | H. pylori Negative | P Value | Odd Ratio | Confidence Interval |
|---|---|---|---|---|---|
| Family number | 7.7 ± 3 | 7.8 ± 3 | 0.8 | 1.02 | 0.82 - 1.23 |
| Age | 36.5 ± 11 | 23.8 ± 10 | 0.93 | 1 | 0.94 - 1.07 |
| Duration of disease in months | 37.2 ± 39 | 37.2 ± 40.1 | 0.9 | 0.99 | 0.98 - 1.02 |
| Gender | 0.71 | 1.38 | 0.25 - 7.61 | ||
| Female | 29/37 (78.4%) | 10/12 (83.3%) | |||
| Male | 8/37 (21.6%) | 2/12 (16.7%) | |||
| Residency | 0.67 | 0.76 | 0.20 - 2.81 | ||
| City | 16/37 (43.2%) | 6/12 (50%) | |||
| Rural | 21/37 (56.8%) | 6/12 (50%) |
5. Discussion
Infection with H. pylori is common and the colonization of gastric mucosa with H. pylori is not a disease in itself (1). However, such an infection carries risk of developing various conditions ranging from gastritis to gastric adenocarcinoma (8). In addition, infection with H. pylori has been linked to extra-gastric disease such as parkinsonism, asthma, heart diseases, and urticaria (9).
H. pylori infects around 50% of the world’s population (1). The prevalence of infection is ranging from 20% in developed countries to up to 80% in developing countries (1). In a study conducted in Duhok, the prevalence of H. pylori was studied in different age groups (5). The prevalence of infection was 36% in children younger than 18 years old. In the same study, the prevalence of H. pylori was 78% in the adult population (5). In agreement with this, the overall H. pylori prevalence was 73.6% in our study. In a study conducted in Iran, the prevalence of H. pylori was nearly 90% of the adult population and estimated to be > 50% of children (10). Then, we investigated H. pylori associated with various risk factor and we found that H. pylori positivity was associated with a higher family number. The same result was found when H. pylori was studied in the pediatric age group in Duhok (11). Additionally, we found a higher H. pylori positivity in subjects residing in the city. This is difficult to explain and further studies are needed to investigate this. No association was found between H. pylori infection and age, gender, or residency. In a study conducted in Turkey, the prevalence of H. pylori infection was less in females, elderly, and unmarried subjects (12). In studies conducted in Iran, low socioeconomic status and education level, higher family member number, and poor oral hygiene were found to be risk factors for H. pylori infection (13). In another study conducted in Nigeria, around 82% of the recruited samples were positive for H. pylori. Low socioeconomic status, unclean water source, overcrowding, and smoking were significant risk factors for H. pylori infection (14). In another study conducted in China, H. pylori prevalence rate was 63.4%, and women had higher infection rate (15). In the same study, no significant association between H. pylori prevalence and smoking was found (15).
The association between H. pylori infection in chronic urticaria has been studied with controversial results. Several studies showed that H. pylori eradication led to a better treatment outcome with a better remission of urticaria symptoms (16, 17), suggesting a possible role for H. pylori in the pathogenesis of urticaria. On the other hand, the prevalence of H. pylori positivity in subjects with chronic urticaria was not significantly higher than that in the control group (17). However, the severity of urticarial was higher in patients with the H. pylori infection. Additionally, after the eradication of H. pylori therapy, more than eighty percent of the H. pylori-positive urticaria group experienced complete remission after receiving eradication therapy for H. pylori (17). One project from Germany showed a better outcome and remission of symptoms after H. pylori eradication (18). On the other hand, another study showed that the symptoms of urticaria was triggered by H. pylori eradication (19). Large, randomized, double-blinded, controlled studies are required to study the therapeutic effect of H. pylori eradication in subjects with chronic urticaria. In our study, no significant difference in H. pylori positivity was found between the patients’ group and control group. In a study conducted in Basrah, Southern Iraq, the prevalence of H. pylori was significantly higher in patients with urticaria than the control group (20). The discrepancy between the two studies could not be explained precisely. However, the discrepancy might be due to a small sample size used in our study, patient’s genetic makeup, and the virulence of the microorganism.
To conclude, the prevalence of H. pylori positivity was high in our city. No association was found between H. pylori and chronic urticaria. Further studies are needed to investigate the effect of H. pylori eradication on the treatment outcome of chronic urticaria.