1. Introduction
The occurrence of myocardial injury in COVID-19 patients, as verified by high levels of cardiac enzymes or ECG and TTE problems is not clear and has been shown to be associated with many variable presentations. However, it is associated with a more severe type of disease and a poor prognosis, especially when accompanied by the complications (1-7). Here we report a case of acute MI (myocardial infarction) in the setting of COVID-19, complicated with flail of the posterior mitral valve leaflet in which the patient was treated accordingly and discharged in a relatively good condition.
2. Case Presentation
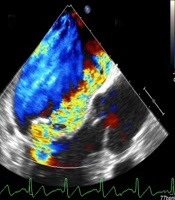
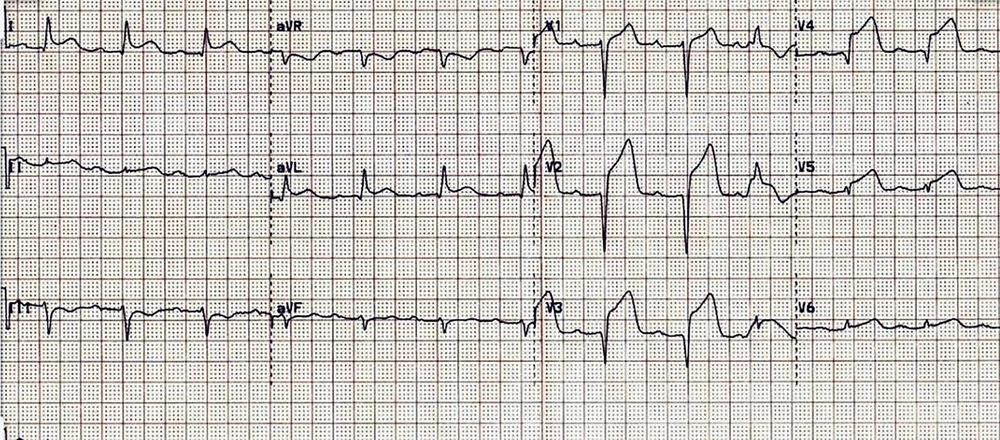
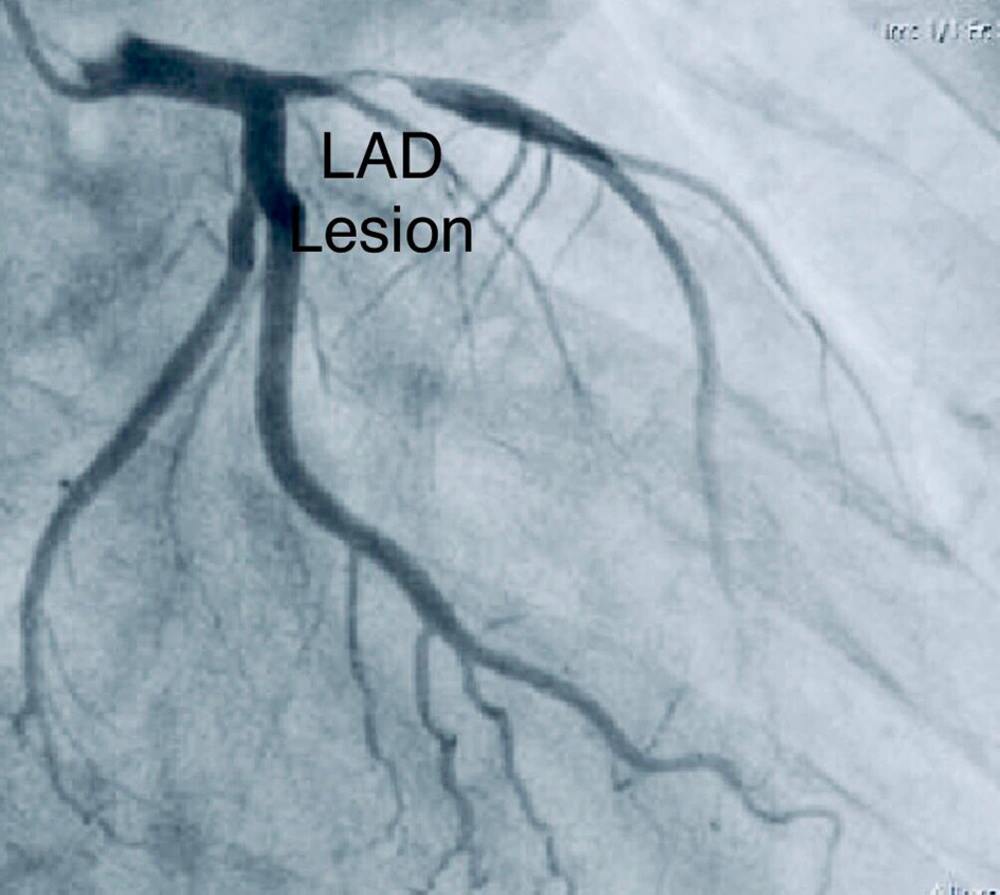
A 58-year-old male came to the emergency department due to dyspnea and severe crescendo type chest pain since 48 hours ago. On initial presentation he was diaphoretic and tachypneic, and O2 saturation in ambient air was 92%. The patient mentioned a previous history of hypertension and hyperlipidemia which he was being treated for. Also, he had a positive family history for coronary artery disease and his father had undergone cardiac bypass at a rather young age of 49. Initial electrocardiogram (ECG) (Figure 1) showed acute antero-lateral ST segment elevation myocardial infarction (STEMI) and trans-thoracic echocardiography (TTE) revealed severe left ventricular systolic dysfunction with mild mitral regurgitation (MR). The patient was immediately transported to the catheterization laboratory and a primary coronary intervention (PCI) procedure was performed on a significant proximal lesion of the left anterior descending artery (Figure 2).
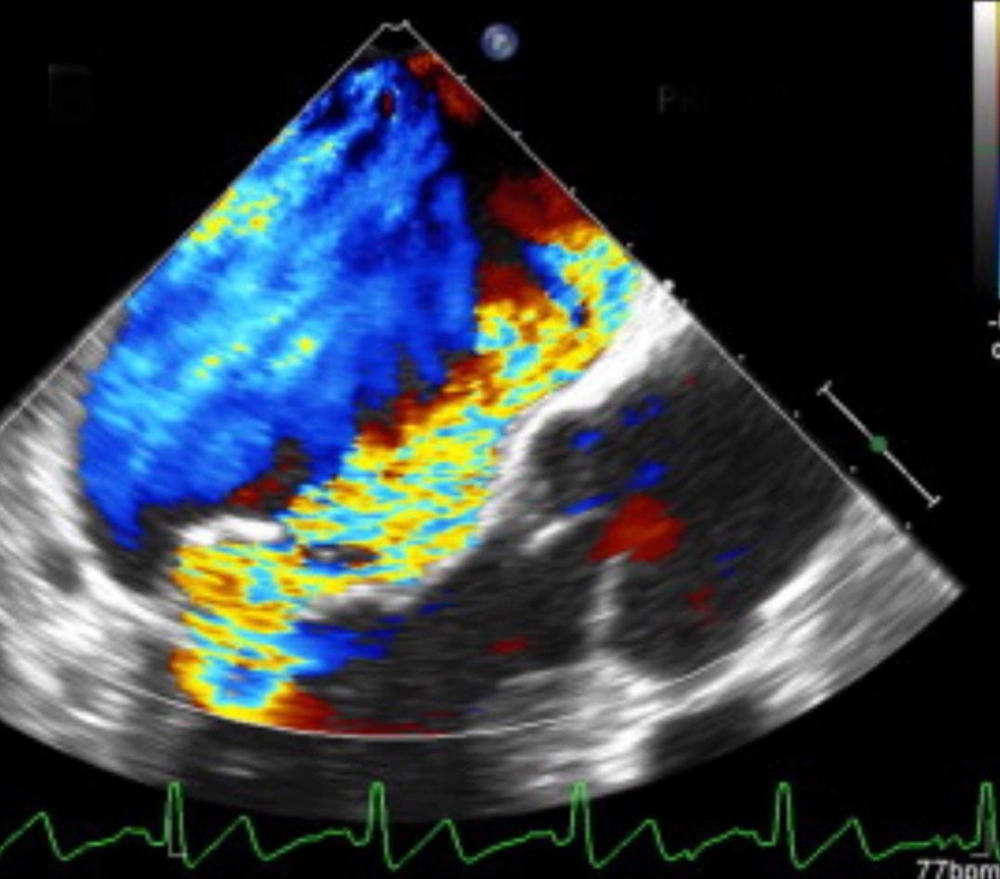
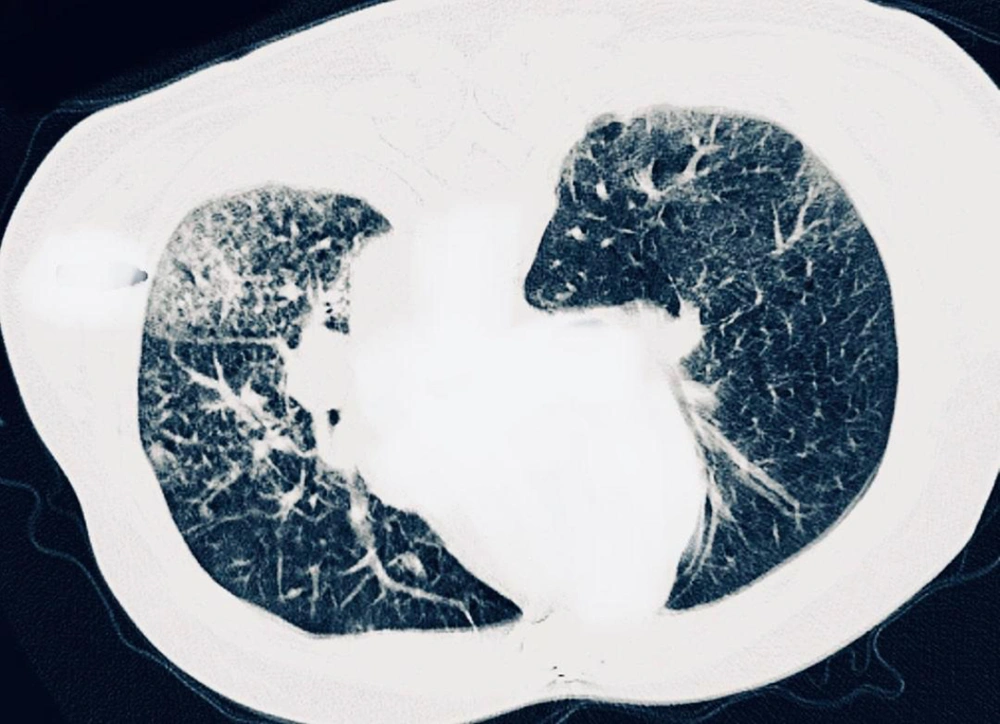
Twenty four hours later, while in recovery, patient suddenly complained of exacerbation of dyspnea. For this reason, TTE was repeated and a chest CT scan was performed. Echocardiographic examination revealed a left ventricular ejection fraction of 20%, severe regional wall motion abnormality in the anterior circulation and a severe anterior directed MR due to rupture of posterior mitral valve leaflet (Figure 3) which was confirmed by trans-esophageal echocardiography (Figure 4). Furthermore, CT-scan was in favour of viral pneumonia and highly suggestive for COVID-19 (Figure 5). A high level of C-reactive Protein and severe lymphopenia, was also seen and the diagnosis of COVID-19 was later confirmed by real time polymerase chain reaction test.
The patient underwent an intra-aortic balloon pump insertion procedure, while being treated medically for pulmonary edema and soon after, an emergent surgery for mitral valve replacement was performed. Treatment with COVID-19 was also initiated and azithromycin and hydroxychloroquine were prescribed, while Kaletra was omitted due to history of recent MI. Treatment was continued for 3 days and after a QT prolongation close to 500 mili-seconds on the 3rd day of treatment, Azithromycin was withheld and hydroxychloroquine 200 mg, continued every 8 hours by ECG monitoring.
After a long period of admission, finally the patient was discharged in relatively good condition and advised to follow-up with a cardiologist.
3. Discussion
The incidence of myocardial injury in patients affected by COVID-19, as verified by elevated cardiac enzymes or electrocardiographic and echocardiographic abnormalities is not exactly known; however it has been associated with a variety of presentations. Also, it is associated with a more severe type of disease and therefore a poor prognosis. Myocardial infarction in COVID-19 is not always due to thrombotic events and the reason for cardiac injury during the infection has been hypothesized to be due to various factors including plaque rupture, cytokine storm caused by severe end-stage disease, hypoxic injury from lung infiltrations, coronary spasms, micro-thrombi induced by the inflammation of the endothelium during infection, or even direct endothelial or vascular injury. Myocardial interstitial edema has been shown on magnetic resonance imaging (MRI) in such patients, confirming the incidence of injury (5-9).
While several cases of patients affected with COVID-19 who had presented with acute coronary syndrome (ACS) due to rupture of atherosclerotic plaques have previously been described (type I MI), such cases have also been previously mentioned in patients with influenza or other viral illnesses, displaying a strong association between viral respiratory infections and myocardial infarction. This has been endorsed to a combination of factors including localized vascular or plaque inflammation during viral infection, activation of smooth muscles, macrophage motivation and tissue factor expression in the atherosclerotic plaque; and activation of platelets. In other words, it could be said that the risk for ACS in afflicted patients with COVID-19 may be high due to the heightened thrombotic activity, as evidenced by significantly elevated D-dimer levels in some studies. Hence, it is important to consider that type 2 MI is the most common sub-type of myocardial injury in viral conditions, therefore the use of an invasive management with a view toward coronary revascularization (particularly in type 2 MI) is limited and the decision for invasive vs. non-invasive management of patients presenting with ACS and COVID-19 should be carefully considered (1, 2, 10-12).
The American College of Cardiology (ACC) states that the treatment of MI is controversial in COVID-19 patients. It is mentioned that although the use of fibrinolytics can be considered in the patients with a low risk STEMI (such as inferior STEMI, with no right ventricular contribution or a lateral MI without compromising hemodynamics), percutaneous coronary intervention (PCI) is more commonly performed in most establishments and is still the treatment of choice in the setting of an acute MI. If PCI is chosen, all the staff in the laboratory should be equipped with suitable personal protective equipment, and complete de-contamination of the laboratory must be accomplished soon after the procedure. For cases that are suspected of having COVID-19 in the setting of Non-STEMI, it is recommended to perform diagnostic testing prior to performing catheterization. The ACC also states that, in some patients with confirmed COVID-19 who have been appropriately selected, conservative treatment may sometimes suffice and on the other hand, Non-STEMI patients who are hemodynamically unstable are to be managed just as those with an STEMI (13).
3.1. Conclusions
Myocardial infarction is one of the important and serious complications of COVID-19 illness and further complications of MI is seen in many of the afflicted. The future review of other affected patients and the use of advanced imaging modalities including advanced echocardiography, mardiac MRI and obtaining tissue biopsies from the patients seem to be essential in order to increase our knowledge of the pathophysiology in which this new viral infection affects the cardiovascular system.