1. Background
Congestive heart failure (CHF) is a debilitating disorder that affects 1-2% of the general population and occurs due to the inability of the heart to pump blood to the bloodstream. Common symptoms include edema, tiredness and shortness of the breath that affects patient's quality of life and life expectancy. Despite recent advances in the evaluation and management of heart failure, symptomatic heart failure still has a poor prognosis (1). Thirty to 50 percent of CHF patients will die during the first year of the diagnosis, and 70% will not survive for more than three years. The recommended treatment for heart failure is the use of angiotensin converting enzyme (ACEI) inhibitors, angiotensin receptor blockers (ARBs), beta blocker, diuretics, and aldosterone antagonists (2, 3). Anorexia, malnutrition, old age, and frequent admission are all factors that contribute to increasing the risk of nutritional deficiencies in patients with congestive heart failure. Micronutrients and trace elements are dietary elements that are vital for the growth and prevention of disease (4).
The micronutrients are not produced in the body, but they should be taken in the required amount of diet, and their required amount is generally less than 100 mg per day. In previous studies, the role of serum levels of elements such as copper in the development of certain cardiac diseases, such as Keshan disease, cardiomyopathies and vascular atherosclerosis has been proven (5). On the other hand, copper deficiency leads to hypertrophic cardiomyopathies in several experimental models, which ultimately leads to systolic and diastolic cardiac function impairment. Copper deficiency is the only nutritional factor that increases cholesterol, blood pressure, homocysteine, and uric acid, leads to glucose intolerance, and increases thrombotic and oxidative damage (6).
Copper plays a role in regulating oxidative free radicals, and its deficiency increases the amount of peroxidation of the lipoprotein. Low copper levels can increase the risk of oxidative damage to muscle cells and may lead to increased plasma cholesterol accumulation. Long-term copper restriction can lead to mitochondrial dysfunction and fragmentation of mitochondria, and also contributes to cardiac dysfunction (7). Several studies have been conducted to investigate the serum level of micronutrients in heart failure patients. However, despite numerous studies, a study with appropriate sample size indicating the relationship between the serum level of the above elements and the severity of the symptoms and factors associated with the prognosis of the disease in these patients was not found by the authors, therefore the importance of this study have been approved.
2. Objectives
The aim of this assessment is to examine serum copper level in patients with heart failure hospitalized in Rajaie Cardiovascular, Medical and Research Center and its related factors in the period of 2017-18.
3. Methods
3.1. Study Setting
It was a cross sectional and hospital-based study that was conducted on patients with heart failure in Rajaie Cardiovascular, Medical and Research Center.
3.2. Study Population
The inclusion criteria were all patients with chronic heart failure diagnosis. Based on this in the study period, 80 patients with heart failure, were considered as the study group.
3.3. Measurements
The variable indices included serum copper levels at the beginning, information on the function class of the patient's dyspnea as NYHA, the etiology of heart failure (based on angiographic evidence that was excluded from the study if angiography was performed), EF according to echocardiography, as well as Pro-BNP and other laboratory variables. This information was obtained from patients through routine check-up tests for all patients with heart failure and were recorded in the checklist. The study cases were followed up for 3 months. After that time, EF, Pro-BNP, NYHA Functional Class were measured again and recorded. Based on the formula for SHFM, the 5-year survival rate of patients was calculated and the serum copper level in these groups, along with Pro-BNP, EF, and the degree of dyspnea of the patients were compared with each other before and after the 3-month period.
3.4. Ethical Considerations
Ethical issues were completely observed by authors. The study group adheres to the principles of medical ethics introduced by the Health Ministry and the declaration of Helsinki and legislation in medical ethics committee of Iran University of Medical Sciences. In addition, ethical committee of Iran University of Medical Sciences approved the protocol of study. In addition laboratory tests on copper level does not have an effect on the patient's treatment process and the results of the assessments are only reported to the patient.
3.5. Statistical Analysis
The data were analyzed by SPSS version 22 (Version 22.0. Armonk, NY: IBM Corp.) and P < 0.05 was considered as statistically significant. We considered t-test for quantitative variables and X2 test for qualitative variables.
4. Results
We evaluated 80 patients with heart failure as our study group, of whom 52 cases (65%) were male and 35 cases (28%) were female with the mean and standard deviation of 49.9 ± 16.2 years (Table 1). In addition we observed that the mean and standard deviation of serum level of copper was 189.2 ± 58.3. In the following, copper levels were evaluated in comparison with other indices in this study (Table 2).
| Variables | Values |
|---|---|
| Gender | |
| Male | 52 (65) |
| Female | 28 (35) |
| Age (years) | |
| Mean | 49.9 |
| Standard deviation | 16.2 |
| Serum Copper Level | Values |
|---|---|
| Mean | 189.2 |
| Standard deviation | 58.3 |
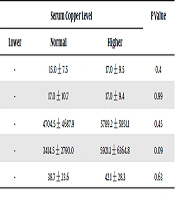
In copper serum level with NYHA function class we found that there is no statistically significant correlation between them (Table 3). However there were statistically significant correlations between copper serum level and etiology of heart failure (Table 3). In addition, other indices including ejection fraction, Pro BNP and SHFM 5, did not have any statistically significant correlation with serum level of copper (Table 4).
| Variables | Serum Copper Level | P Value |
|---|---|---|
| NYHA (primary) | 0.908 | |
| I | - | |
| II | 196.8 ± 39.1 | |
| III | 192.2 ± 62.0 | |
| IV | ||
| NYHA (3 months later) | 0.324 | |
| I | 212.1 ± 117.5 | |
| II | 183.6 ± 42.4 | |
| III | 193.0 ± 56.0 | |
| IV | 213.4 ± 40.4 | |
| Etiology of heart failure | 0.025 | |
| ICMP | 193.1 ± 51.9 | |
| DCM | 184.4 ± 51.1 | |
| Other etiologies | 247.6 ± 13.5 |
| Variables | Serum Copper Level | P Value | ||
|---|---|---|---|---|
| Lower | Normal | Higher | ||
| Ejection fraction (primary), mean ± SD | - | 15.0 ± 7.5 | 17.0 ± 9.5 | 0.4 |
| Ejection fraction (3 months later), mean ± SD | - | 17.0 ± 10.7 | 17.0 ± 9.4 | 0.99 |
| Pro BNP (primary), mean ± SD | - | 4704.5 ± 4687.9 | 5789.2 ± 5851.1 | 0.45 |
| Pro BNP (3 months later), Mean ± SD | - | 3414.5 ± 2790.0 | 5921.1 ± 6364.8 | 0.09 |
| SHFM 5, Mean ± SD | - | 38.7 ± 23.6 | 42.1 ± 28.3 | 0.63 |
5. Discussion
We found that the mean and standard deviation of serum level of copper was 189.2 ± 58.3. We have also observed that there was no statistically significant correlation between serum copper levels and NYHA function class, ejection fraction, Pro BNP and SHFM 5. In a study in 2008, Kazi et al. evaluated the effect of several micronutrients on the cardiac status of patients with heart failure and stated that Fe and Cu concentrations in these subjects increased by 0.83% and 3.12%, respectively (8). In another study, Arroyo et al. tested the serum selenium levels and the level of copper in African-American patients with long-term, short-term, and compensated heart failure, and stated that, in the long-term group, copper deficiency were positive in 70% and lower than normal levels were positive in 100% of patients. These values were 50% and 60% in the short-term group, and 50% and 100% in the compensated group, respectively. The study concludes that low levels of nutritional value of the elements examined will not only affect heart failure, but also can affect its severity (9). Also Kosar et al. in another study in Turkey, measured serum zinc (Zn), copper (Cu) and selenium (Se) levels in 54 patients with chronic heart failure and 30 healthy individuals, and stated that heart failure was associated with low concentrations of Se and Zn and a higher concentration of Cu (10) which are partly consistent with the results of our assessment. Topuzoglu et al. studied the concentration of trace elements (Cu, Zn, Mg) in the serum of patients with cardiomyopathy, and found that patients with dilated cardiomyopathies had higher copper and zinc concentrations than healthy ones (11). In another study by Shokrzadeh et al. (cited in Tabari et al.) zinc and copper levels were measured in 30 patients with ischemic heart failure and 27 healthy volunteers, suggesting that the mean serum copper level in patients with ischemic heart failure has significantly exceeded copper levels in healthy volunteers (12). Saleh et al. studied a group of patients with cardiomyopathy and reported that the mean level of serum copper in patients with coronary artery disease and normal EF has significantly decreased compared to the control group (13). In another study by Nouraei et al. the serum levels of zinc and copper in patients with advanced chronic heart failure were measured and indicated that there was no significant difference in serum levels of zinc and copper in patients with normal sinus rhythm and AF. However, both groups showed a significant shortage of zinc and a reduced ratio of Zn / Cu compared to the control group (14). Zeraatkar et al. in a study, have observed that behavioral interventions had a short-term impact on quality of life and its psychological components (15). Accordingly, most studies in this field have been consistent with the results of our assessment, which indicates that there are not any significant correlation between this microelements and condition of patients with heart failure.
5.1. Conclusion
Based on the results obtained from this study and also with regard to the results obtained from other studies in this field, because none of the patients’ serum copper level were not under the base line we could not found a significant effect on the status of patients with heart failure, and the only difference was observed in the etiology of heart failure which has a statistically significant correlation with serum copper levels and therefore, further studies are needed to confirm these results.
5.2. Limitations of the Study
Due to small sample size in a single center and short follow up we could not find any significant effect on the status of patients with heart failure since copper level did not go under the baselinein our study group. We believe further studies with larger sample size in multiple centers and longer follow-ups are required to approve the results of this study.