1. Background
Sudden cardiac arrest is a common health predicament associated with extraordinary levels of mortality. Cardiopulmonary resuscitation (CPR) is a therapeutic intervention that develops the opportunity of survival for a patient experiencing cardiac arrest or heart failure. Otherwise, CPR is a combination of interference carried out to provide an appropriate amount of oxygen and blood flow to the patient during cardiac arrest. Cardiac arrest may be because of a medical condition such as pulmonary dysfunction, a variety of strokes, heart disease, cancers, poisoning, electrocution, drowning, or frostbite (1-3).
Essential issues in prediction and consequences of cardiac arrest are the time of beginning CPR, the situation of cardiac arrest, underlying disorder, first electrocardiogram (EKG) rhythm, defibrillation, and the state of CPR (4, 5). In a previous study, we evaluated the effect of different practical factors such as age group, gender, season, present of witnesses, location, ward of the hospital, and working shift on the CPR success rate. The mentioned comparison did not explicate any significant progress in CPR success rate in the presence of witnesses, location of cardiac arrest, season, and gender. Against, the main factors contributing to advanced rate of CPR were age, work shift, and hospital wards (6). In the continuation of the previous study, we will examine the outcome of resuscitation and its relationship with underlying diseases, patients’ first cardiac rhythm in the first monitoring, and the effects of using a cardiac defibrillator.
2. Objectives
This study aims to determine the eventual success rate of CPR in subjects who had a cardiac arrest at a referral hospital in southwestern Iran.
3. Methods
The retrospective examination explained the medical histories of any in-hospital cardiac arrest patient, which sustained CPR through two years between January 2017 and June 2018. The Ethical Committee approved this investigation of Ahvaz Jundishapur University of Medical Sciences. Well-to-do CPR described by subjects that have a return of spontaneous circulation (ROSC) after CPR, subject alive for longer than 24h. According to the American Heart Association, when CPR causes the patient’s heart rate to return spontaneously, it is called a successful CPR (7, 8). This cardiovascular and trauma center is equipped with 700 beds and an emergency department (ED). Throughout the historical study period, more than 80,000 patients were admitted to the hospital, of which 594 patients underwent cardiac arrest. The obtained data, includes the success rate of CPR, patients’ past medical history, primary detected cardiac rhythm, and use of defibrillator.
Inclusion criteria: patients (age > 10 years) who sustained either cardiac arrest, or those who experienced CPR in the hospital. Exclusion criteria: Subjects that presented dead at arrival, those with excellent guidance of no CPR (NCPR), or those missing documents or inadequate data.
Statistical analysis. Simple logistic regression and chi-square tests were used to describe qualitative variables. The data were analyzed using SPSS version 22.0 (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.), and P-value < 0.05 was considered significant.
4. Results
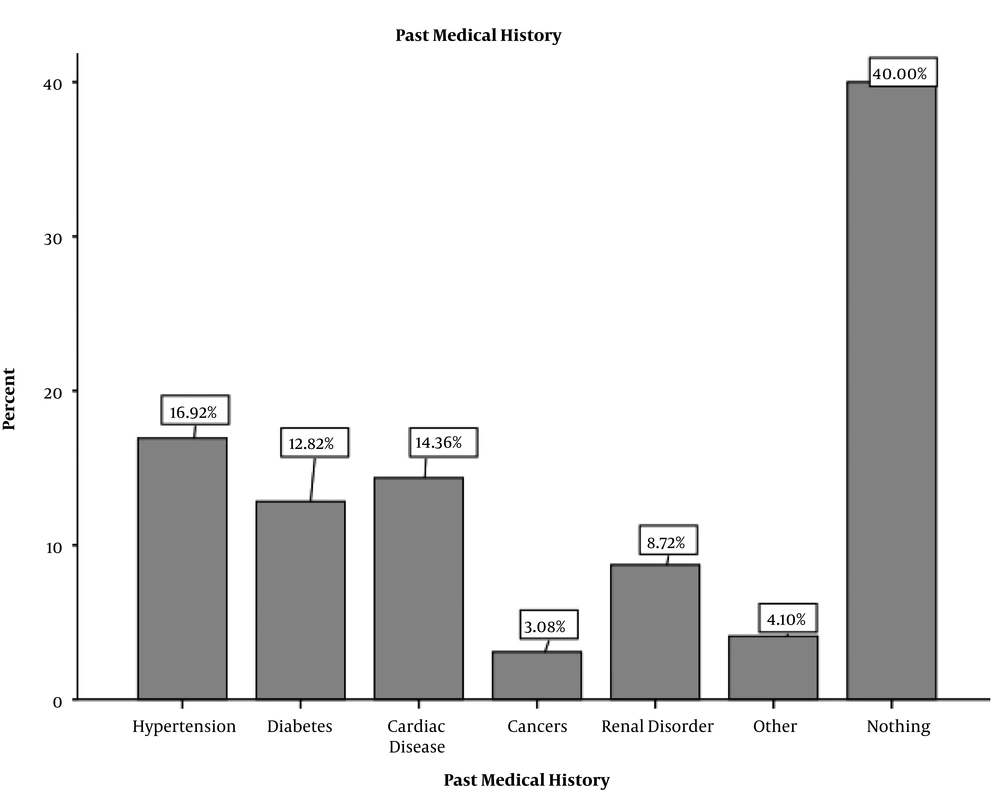
Overall, 594 CPR operations were carried out of which 155 (26.3%) were successful, and 439 other operations (73.7%) were unsuccessful. Sixty percent of patients with cardiac arrest had an underlying disease, including hypertension, diabetes, cardiac disease, malignancies, renal and other diseases (Figure 1).
The results showed that 40% of the patients under CPR had no underlying medical conditions. Also, 55.9% of them had conditions, including renal or cardiac disorders, diabetes, cancer, and hypertension (Table 1). Notably, the highest percentage of successful resuscitations occurred in individuals who did not reported any history of underlying disease. As you can see, resuscitation’s success rate is significantly correlated with underlying diseases of hypertension, diabetes, and cardiac and renal disease. In patients with the mentioned diseases, the success rate of resuscitation was considerably lower.
| Past Medical History | CPR, % | P-Value | |
|---|---|---|---|
| Unsuccessful | Successful | ||
| Hypertension | 72.7 | 27.2 | 0.000 |
| Diabetes | 64 | 365 | 0.001 |
| Cardiac disease | 57.1 | 42.8 | 0.000 |
| Cancers | 83.3 | 16.6 | 0.91 |
| Renal disorder | 76.5 | 23.55 | 0.009 |
| Other | 62.5 | 37.5 | 0.47 |
| Nothing | 9 | 91 | 0.000 |
aValues expressed as frequency %. P-value < 0.5 assign as significant.
Another case study checked the first cardiac rhythm seen in arrested patients. The first rhythm of asystole had the highest percentage, and the lowest was pulseless electrical activity (PEA). Data analysis showed that there was no significant correlation between the success rate of resuscitation and the first recorded cardiac rhythm (Table 2).
| First Detected Cardiac Rhythm | Frequency % | CPR Rate, % | P-Value | |
|---|---|---|---|---|
| Unsuccessful | Successful | |||
| Asystole | 77.2 | 56.1 | 21 | 0.086 |
| PEA | 10.7 | 6.8 | 3.9 | 0.149 |
| VF & VT | 12.1 | 6.9 | 5.17 | 0.062 |
aValues expressed as frequency %. P-value < 0.5 assign as significant.
Despite this, the use of implantable cardioverter-defibrillator (ICD) shock has a specific indication, but one of the actions in the CPR process is a defibrillator. In this investigation, it was found that 594 people under CPR, defibrillator, used for 125 people. The analysis explains that the use of defibrillator has no significant correlation with CPR outcomes (Table 3).
| Use of Defibrillator | Frequency % | CPR Rate, % | P-Value | |
|---|---|---|---|---|
| Unsuccessful | Successful | |||
| Yes | 21.1 | 65.2 | 34.2 | 0.419 |
| No | 78.9 | 73 | 26.7 | |
aValues expressed as frequency %. P value< 0.5 assign as significant
5. Discussion
The present study was designed to determine the effect of some necessary conditions on the CPR success rate. As noted, CPR results were significantly unsuccessful in individuals suffering from hypertension, diabetes, and heart and kidney disease. Survival after resuscitation can be affected by factors such as the quality and urgency of the procedure and the treatment team skill, patient’s age, underlying disease, and individual characteristics (9-11). A retrospective study in Switzerland in 2018 revealed the success rate of CPR, and the survival of patients for 30 days was 13%. In this study, similar to the results of our survey, the most common underlying diseases that caused resuscitation defeat were cardiac failure, myocardial infarction (MI), diabetes, kidney disease, and finally metastatic malignancies, respectively. The study also reported that the higher the patient’s complexities, the lower the chances of survival after CPR (12). In 2015, a study in the United States reported a success rate of resuscitation of 21.9 percent, with the lowest success rate for dialysis patients (13). In review literature following in several articles, the importance of underlying diseases was discussed, and similar to our investigation, the most common underlying diseases were hypertension, heart disease, and diabetes (14).
As seen in the results section, the first detected cardiac rhythm did not significantly correlate with the success rate of CPR, but the highest success rate was detected in VF and VT, PEA, and ASYSTOLE rhythm, respectively. A 2018 study reported a 29% survival rate of CPR for 30-day. It went on to say that in 45% of people with a positive resuscitation results, their initial cardiac rhythm was VF and VT, 40% had a PEA rhythm, and 15% had no rhythm (15). Similarly, in the present research, in the subjects whose first detected cardiac rhythm after monitoring was VF and VT, the success rate of CPR was almost 43%. Another study reported a first post-cardiac arrest monitoring rhythm of 62.6% asystole, 28.7% PEA, and 8.8% non-shockable rhythm. The success rate of CPR was 25.6%, but survival at discharge was 2.4% (16). Comparable to our results, an investigation in 2020 noticed that people with an initial rhythm of asystole or PEA were less likely to survive after CPR confront characters with VF and VT initial rhythm. The study also reported a success rate of 27.8% for the restoration and return of spontaneous circulation (17).
In this experiment, the cardiac defibrillator application had no significant response to the success rate of resuscitation. The factors affecting the outcome of resuscitation and successful result of using a cardiac defibrillator could be affected by age, weight, a past time of cardiac arrest, the cardiac rhythm, affected area, etc. (18, 19). The optimal time to use cardiac shock is the first zero to 4 minutes of cardiac arrest. So in many cases where the resuscitation team arrives late at the patient’s bedside or the cardiac arrest occurs outside the hospital, using a defibrillator is not as effective (20).
5.1. Conclusions
The current study is the second epidemiological study of cardiac arrest at this center and revealed that past medical histories are an essential issue in CPR outcomes. Moreover, people without the underlying disease have a significantly higher chance of survival. Specific criteria are necessary to predict better outcomes of CPR.
5.2. Limitation
Since the present study is retrospective and based on pre-completed forms, change of many cases is beyond the scope of this work. Also, some of the questionnaires were not completely filled out, and this was one of the critical limitations of our work.