1. Introduction
Pulmonary fistula is a relatively rare congenital malformation that occurs due to a direct connection between venous and arteries without a superseding capillary bed (1).
This disease is seen sporadically in approximately 5 - 20% of cases, but in most cases it is seen as syndromic and a part of diseases such as Osler-Weber Rendu syndrome or hereditary hemorrhagic telangiectasia (HHT) (2).
Studies show that in 56% of cases, the disease has no symptoms, but, fistulas may enlarge as the patient gets older and cause symptoms such as dyspnea, cyanosis and clubbing (1).
On the other hand, there is a brain AVM that is usually seen sporadically and asymptomatic (3). The prevalence of this disorder is about 15 per hundred thousand. It is usually seen equally in all age groups and both sexes (4) with the most common manifestation is intracerebral hemorrhage, but it can present with seizures, headache or neurological disorders (5).
Given that the occurrence of both of these disorders simultaneously and sporadically is very rare, we focused on the coexistence of these two idiopathic anomalies in a unique patient with no recognized syndromes who developed a brain abscess in this article. In addition, the manifestations of the disease and its course and treatment are described.
2. Case Presentation
Our patient is a 16-year-old adolescent known case of pulmonary arteriovenous (AV) malformation who referred to our clinic due to persistent and refractory headaches from two months ago, with a history of brain CT scans revealing intracranial hemorrhage (ICH) and multiple AV malformation in cerebellum and cerebral in another center. At the beginning of the visit, the patient has central cyanosis and obvious clubbing. Blood oxygenation (SO2) was about 59%.
The beginning of the problems of the patient was in 7 years old, that started by progressive cyanosis. After workup in our hospital we found multiple bilateral pulmonary AV malformation. Evaluation studies on that time have shown no signs of inherited syndromes. Due to the progression of symptoms and severe shortness of breath with the diagnosis of sporadic pulmonary disorder, we decided to performing intervention for the malformations, we have closed the malformations three times at the ages of 7 (Figure 1), 8 and 12 years with coil and Occluder devices.
However, due to the progression of symptoms (dyspnea and cyanosis), angiography was performed again at 13 years of age, which showed that the lesions had progressed (Figure 2) and we believed that the intervention could not help any further, and that the patient was a candidate for lung transplantation.
The patient referred to our center again at 14 years of age by fever and severe headache. After performing the necessary examinations, she was diagnosed with a brain abscess and underwent medical treatment and abscess drainage. After two months, she was discharged in a relatively good general condition.
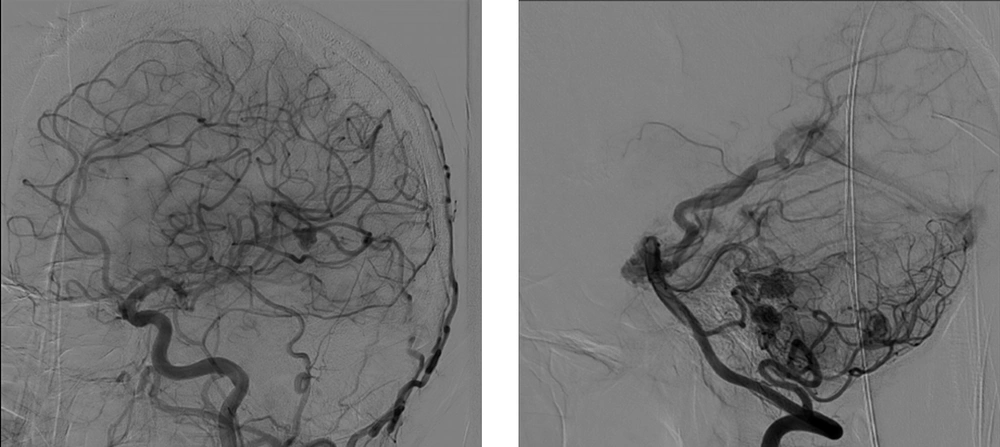
At the current visit, with a severe resistant headache and intra cranial hemorrhage (ICH), a brain CT scans examination was performed, which showed that the patient had multiple cerebral and cerebellum bilateral AVMs and due to the disseminated of brain lesions (Figure 3), it was decided to close them with interventional procedure and three of the largest lesions were closed using Onyx adhesive glue. The patient had temporary dysarthria which was completely resolved after two days. She was listed for lung transplantation in the near future.
3. Discussion
Reported patient in this article is a rare case of simultaneous brain and pulmonary AVMs that presented in different ages with unusual symptoms.
The prevalence of sporadic congenital brain AVMs in retrospective studies has been about 1 - 5 in 1000 (3). Most of them become symptomatic during life at different ages and will require careful attention and care even if they are accidentally diagnosed. Furthermore, 43 to 71% of these patients present with cerebral hemorrhage, 18 to 40% have seizures and 5 - 14% present with headaches (6).
Our patient's symptoms were only headaches, which is one of the very rare manifestations of the disease. Another problem in this patient is the coexistence of progressive and extensive pulmonary AVMs, which is a very rare association and have caused such complications. In general, due to the severe complications seen in patients with PAVMs, most studies recommend the treatment of these lesions (7, 8). However paradoxical emboli which may lead to stroke or brain abscess is a concern that indicate the need for intervention for patients with pulmonary AVMs (9).
In general, 15 to 30% of brain abscesses are cryptogenic in nature, which can be caused by heart problems (10).
However, due to the presence of a resistant blood-brain barrier and abundant cerebral circulation, the probability of these abscesses following pulmonary AVM is about 5% (11), which was also observed in our patient, that can be due to the spread, reanalyzed and new lesion with a high volume of the shunt inside the lungs (12).
Recurrence in pulmonary AV malformation after successful treatment is due to recanalization or reperfusion via pulmonary and bronchial arteries in about 25% of patients, and both of them have been reported in previous studies (13, 14). In our case also both reperfusion and recanalization cause recurrence of AV malformation after 10 coil and 2 occluder device during three sessions of intervention.
Today, the standard treatment for these lesions is endovascular ligation, which has been performed in our patient over the years due to the recurrence of the disease, and the use of this number of devices in one patient has rarely been reported in studies.
The important thing in such a case is the timing and treatment of AVMs that has been one of the most challenging topics for the last 30 years. Several treatments such as surgical resection, embolization through intra-arterial, stereotactic radiosurgery (SRS) or a combination of methods have been proposed that vary based on the risk of cerebral hemorrhage as well as the risk of surgery (3).
Large and diffuse lesions and those that are located in certain parts of the brain or have deep venous drainage have a high risk of surgery and complications, so alternative therapies such as endovascular can be used (6).
But due to the unknown nature of the disease and the low annual rupture rate, it is very difficult to decide when to remove the brain AVMs. Due to the fact that mortality and morbidity due to cerebral hemorrhage following the rupture of these AVMS are high. However it is generally recommended to decide on the treatment of the patient immediately after diagnosis (6).
Our patient was also a candidate for endovascular method with Onyx glue due to the presence of extensive lesions in different areas of the brain and presences of lung AVMs with cyanotic nature that increased the risk of surgery.
Endovascular treatment is one of the relatively new methods in closing these disorders in which materials such asn-butyl 2-cyanoacrylate (NBCA) and ethylene vinyl alcohol (EVOH) or Onyx adhesives are used. This method has fewer side effects and is used in cases where the lesions are large and diffuse. This is due to the fact that removing such lesions has the risk of mortality and irreversible brain complications (3).
Safety and efficacy of endovascular methods in patients with AVMs has been proven, but due to high prevalence of complications and the risk of recurrence of long-term follow-up lesions, it is recommended to undergo high resolution CT scans every three to five years for lung lesions (11). Furthermore, the use of anticoagulants have been reported to prevent brain damage, nevertheless whether these drugs are safe or not should be further investigated (15).
To our best knowledge, our patient is the first reported case of simultaneous pulmonary and brain AV malformation with unusual presentations and no specific syndromic disease.
3.1. Conclusion
It can be concluded that patients with pulmonary AVMs, although sporadic, need careful examination for other congenital disorders and it is necessary to pay attention to the presence of these anomalies in other organs, even though it is rare. Another important issue is the risk of recurrence of these lesions as a result of recanalization, reperfusion or the formation of new lesions, which also makes endovascular treatment difficult. In general, due to the unknown nature of the disease and its progression, the treatment of these lesions is completely based on patients’ characteristics and varies according to each patient. Assessing the risk of surgery and its complications and comparing it with the endovascular method can also help the number of lesions in deciding the type of treatment.