1. Background
Cognitive impairment is among common complications in patients undergoing CABG. Deep hypothermia is significantly more effective in reducing the risk of cognitive impairment than normothermia and mild hypothermia. However, other factors, such as the duration of cardiopulmonary bypass (CPB) contribute to the severity of cognitive impairment (1). Kiabi et al. stated that cognitive deficits have a direct relationship with the low mean arterial pressure and an increase in the duration of CPB (2). Typically, H-CPB (28 - 30°C) is more prevalent than N-CPB (35 - 37°C) (3). The main reason for the cooling of the body is to protect vital organs, such as the brain, kidneys, and the heart from ischemic injury by lowering basal metabolism, thereby reducing oxygen consumption (4). Many physiological and neurological complications occur following cardiac surgery (5). Post-operative cognitive deficits are defined as deficits in the memory, attention, and psychomotor function, which occur in more than one-third to four-fifths of the patients (6). Thus far, interventions have not been proven to be effective in preventing these effects (7). Experimental studies show that during cooling with the hypothermic method, the increase in blood concentration and the decrease in the plasma volume lead to plasma entrapment in parts of the vascular bed or cause plasma to penetrate into the interstitial space. In the normothermic method, the patient's temperature automatically decreases to 35°C without topical cooling (8). Research in the review study shows that postoperative complications in the normothermic method are less frequent than in the hypothermic method (9). Therefore, in this study, it is assumed that postoperative cognitive impairment is less severe in the normothermic method than in the hypothermic method. Today, cardiac surgery, including CABG, is performed using the two methods of hypothermia and normothermia. However, there is no broad consensus over a method with less severe cognitive impairment.
2. Objectives
This study aims to compare the effects of hypothermia and normothermia on postoperative complications in patients undergoing CABG.
3. Methods
The objective of this cohort observational study was to compare the effects of hypothermia and normothermia on cognitive functions of patients after CABG during hospitalization. This study was extracted from an MSc dissertation, after it was approved by the University Research Council and the Ethics Committee of Rajaie Cardiovascular, Medical, and Research Centre affiliated to Iran University of Medical Sciences. Besides, it was carried out in Tehran from 2018 to 2019. The statistical population of this study included all patients who were candidates for CABG, who referred to Rajaie Cardiovascular, Medical, and Research Centre. After performing quota sampling to classify the two variables of age and sex, 65 people were included in the study in each of the hypothermic and hyperthermic groups. The inclusion criteria were volunteer CABG patients of both sexes, adults within the age range of 18 to 75, being able to communicate, experiencing at least six days of hospitalization, and having no cognitive impairment in the past. The exclusion criteria included cardiac arrest during or after surgery, hemodynamic instability during and after surgery, carotid stenosis greater than 50%, history of alcohol use, and patients in need of emergency surgery. Besides, all participants were informed of the purpose of the study and signed informed consent forms to participate in this study. All surgeries were performed by two surgeons. After transferring the patients to the operating room and monitoring them, an arterial line was inserted, and brain oximetry monitoring was performed. Besides, induction and maintenance of anaesthesia were performed with midazolam, sufentanil, and atracurium. After intubation, the central venous line was inserted. Accordingly, nasopharyngeal temperature monitoring was performed, and patients received 300 u/kg of heparin 10 minutes before cannulation. In addition, a suitable oxygenator was selected according to the patient's BSA and required flow. Next, the cardiopulmonary bypass pump device was primed with the Ringer's lactate serum. In addition, other materials, such as menthol 0.5 to 1 g/kg and heparin 100 mg/kg were added to the priming solution. Mild hemodilution to hematocrit 20 and intermittent cold-blood cardioplegia (ICBC) were performed for all patients. The cardioplegia solution as an anti-gradient and the retrograde were injected at the ratio of 4: 1 at 30 mL/kg, with half of this value repeated every 40 to 60 min if needed. In the hypothermic group, the temperature was decreased to 32°C, and in the normothermic group, the temperature was decreased to 35°C. After performing the surgery and transferring the patients to the ICU, demographic data, such as age, sex, and educational level were obtained. At the same time, the Mini-Mental State Exam (MMSE) questionnaire (10) was completed from day 2 to day 6 postoperatively at the ICU. The questionnaire was made up of 6 sections that measured different cognitive domains, which could be completed in less than 10 minutes by a trained physician or a technician. The main use of the cognitive status assessment tool is to compare cognitive status changes over time. Scores between 20 - 24, 11 - 19, and 0 - 10 indicated mild cognitive impairment, moderate cognitive impairment, and severe cognitive impairment, respectively. After data collection, data were normalized using the Kolmogorov-Smirnov method. Besides, data were analysed using descriptive statistics (frequency distribution, mean, and standard deviation) as well as inferential statistics (the independent t-test and a chi-square test) in SPSS version 25 (IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). In addition, P < 0.05 was considered statistically significant.
4. Results
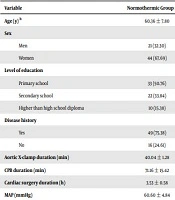
From a total of 130 patients who participated in this study, 65 were evaluated by the normothermic method, and 65 others by the hypothermic method. The results of the Kolmogorov-Smirnov test showed that the data had normal distribution (P > 0.05) at seven time points. Table 1 shows individual-educational characteristics of the patients. Accordingly, the mean ± SD age in the normothermic and hypothermic groups was 60.36 ±7.80 and 60.60 ±7.50, respectively. Besides, most of the participants were women [44 (67.69%) and 45 (69.23%) in the normothermic and hypothermic groups, respectively]. Regarding the variable of the education level in the normothermic group, 33 (50.76%) had primary education, 22 (33.84%) had secondary education, and 10 (15.38%) had high school diplomas and above. Besides, in the hypothermic group, 43 (66.15%) had primary education, 13 (20%) had secondary education, and 9 (13.84%) had high school diplomas and above. Besides, the two groups were quite similar in their history of disease. However, the results showed no significant difference between the two groups in educational and social demographic characteristics (P > 0.05). Therefore, the two groups were homogeneous in this respect (Table 1). In addition, there was no significant relationship between preoperative cognitive function scores between the two groups (P = 1.000). Moreover, none of the patients in the two groups suffered from mild cognitive impairment. The results showed that on the second day after surgery, there was a significant relationship between the two groups in cognitive scores (P = 0.003). Additionally, patients suffered from less cognitive impairment in the normothermic group than in the hypothermic group. Besides, the results of the third day after surgery showed a significant relationship between the two groups in cognitive scores (P = 0.000). Thus, patients in the normothermic group suffered from less severe cognitive impairment than those in the hypothermic group. In addition, the results of the fourth day after surgery showed a significant relationship between the two groups in cognitive scores (P = 0.023). Thus, patients in the normothermic group had less severe cognitive impairment than those in the hypothermic group. Besides, the results of the fifth postoperative day showed no significant relationship between the two groups in cognitive scores (P = 0.079). In addition, the results of the sixth postoperative day showed no significant relationship between the two groups in cognitive scores (P = 0.11). However, although the number of people with cognitive impairment was lower in the normothermic group than in the hypothermic group (Table 2), there was no significant differences in the cognitive scores between the normothermic and hypothermic groups on the fifth and sixth days. The results also showed that in other clinical outcomes, including 24-hour blood drainage (P = 0.000), length of stay at the ICU (value = 0.005), and the transfusion rate (P = 0.004), there were significant differences between the two groups (Table 3). Thus, patients in the normothermic group had better clinical outcomes than those in the hypothermic group.
| Variable | Normothermic Group n = 65 | Hypothermic Group n = 65 | P-Value | df |
|---|---|---|---|---|
| Age (y) b | 60.36 ± 7.80 | 60.60 ± 7.50 | 0.749 | 128 |
| Sex | 0.850 | 1 | ||
| Men | 21 (32.30) | 20 (30.76) | ||
| Women | 44 (67.69) | 45 (69.23) | ||
| Level of education | 0.159 | 2 | ||
| Primary school | 33 (50.76) | 43 (66.15) | ||
| Secondary school | 22 (33.84) | 13 (20) | ||
| Higher than high school diploma | 10 (15.38) | 9 (13.84) | ||
| Disease history | 1.000 | 1 | ||
| Yes | 49 (75.38) | 49 (75.38) | ||
| No | 16 (24.61) | 16 (24.61) | ||
| Aortic X-clamp duration (min) | 40.04 ± 1.28 | 47.23 ± 19.57 | 0.12 | 102.29 |
| CPB duration (min) | 71.16 ± 15.42 | 86.12 ± 26.98 | 0.000 | 101.79 |
| Cardiac surgery duration (h) | 3.53 ± 0.58 | 3.90 ± 0.49 | 0.000 | 128 |
| MAP (mmHg) | 60.60 ± 4.84 | 60.67 ± 6.75 | 0.941 | 116.09 |
Abbreviations: CPB, cardiopulmonary bypass; MAP, mean arterial pressure.
a Values are expressed as mean ± SD and No. (%) unless otherwise indicated.
bt = -0.17.
| Variable | Normothermic Group n = 65 | Hypothermic Group n = 65 | P-Value | χ2 | df |
|---|---|---|---|---|---|
| Preoperative cognitive score | 1.000 | a | - | ||
| Normal | 65 | 65 | |||
| Mild | 0 | 0 | |||
| Medium | 0 | 0 | |||
| Severe | 0 | 0 | |||
| Cognitive score two days after surgery | 0.003 | 13.6 | 3 | ||
| Normal | 51 | 37 | |||
| Mild | 6 | 19 | |||
| Medium | 8 | 5 | |||
| Sever | 0 | 4 | |||
| Cognitive score three days after surgery | 0.000 | 17.8 | 3 | ||
| Normal | 56 | 35 | |||
| Mild | 7 | 22 | |||
| Medium | 2 | 3 | |||
| Sever | 0 | 5 | |||
| Cognitive score four days after surgery | 0.023 | 9.5 | 3 | ||
| Normal | 56 | 42 | |||
| Mild | 7 | 15 | |||
| Medium | 2 | 4 | |||
| Sever | 0 | 4 | |||
| Cognitive score five days after surgery | 0.079 | 6.7 | 3 | ||
| Normal | 60 | 50 | |||
| Mild | 5 | 12 | |||
| Medium | 0 | 2 | |||
| Sever | 0 | 1 | |||
| Cognitive score six days after surgery | 0.111 | 1.03 | 1 | ||
| Normal | 58 | 54 | |||
| Mild | 5 | 11 | |||
| Medium | 2 | 0 | |||
| Sever | 0 | 0 |
| Variables | N.CPB | H.CPB | P-Value | df | t |
|---|---|---|---|---|---|
| 24-hour drainage (mL) | 364.61 ± 247.33 | 622.30 ± 457.91 | 0.000 | 98.41 | -3.99 |
| HB. post (mg/dL) | 10.03 ± 1.36 | 9.80 ± 0.900 | 0.254 | 128 | 1.14 |
| Intubation time (h) | 12.47 ± 2.16 | 11.18 ± 5.29 | 0.072 | 84.85 | 1.82 |
| Time of ICU stage (h) | 47.78 ± 8.23 | 52.06 ± 8.74 | 0.005 | 128 | -2.87 |
| FFP. post (u) | 1.73 ± 0.44 | 1.81 ± 0.391 | 0.296 | 126.06 | -1.05 |
| PRBCs. post (u) | 1.46 ± 0.502 | 1.7077 ± 0.458 | 0.004 | 126.93 | -2.91 |
Abbreviations: HB, hemoglobin; FFP, fresh frozen plasma; PRBCs, packed red blood cells.
a Values are expressed as mean ± SD unless otherwise indicated.
5. Discussion
The results of this study showed that patients in both normothermic and hypothermic groups suffered from cognitive impairment after surgery (11). The results also showed that on the first, second, third, and fourth days after surgery, cognitive impairment was less strong in the normothermic method than in the hypothermic method. Although cognitive scores on the fifth and sixth days after surgery were somewhat better in the normothermic group than in the hypothermic group, no statistically significant differences were found between the two groups. In searching valid sources, such as PubMed, Cochrane Library, Scopus, ProQuest, and Google Scholar, no observational cohort study was found to have evaluated and compared cognitive status of patients after CABG using normothermic and hypothermic methods. Consistent with the results of the present study, Baos et al. reported that cognitive impairment in the normothermic method was less severe than in the hypothermic method (12). In most of the studies, including the present study, cognitive functions are measured using psychometric tests (13-15). However, in the study by Grimm et al., they did not use psychometric tests in hospitalized patients (16). In this study, the findings of the p300 auditory device showed that patients in the normothermic group had better cognitive functions than those in the hypothermic group (the traditional method), being consistent with findings of the present study. In the aforementioned study, the p300 auditory device was used to identify cognitive impairment. Since the methodology used in the mentioned study had higher validity and reliability than psychometric tests, being consistent with the results of the present study, it could verify validity of our study. Poncelet et al., in their clinical trial study, found out that the normothermic method was more effective than the hypothermic method in terms of neurological status (17). The hypothesis of Grigore et al.'s study that the hypothermic approach would reduce cognitive impairment was rejected (13). Boodhwani et al. (2006) reported that cognitive functions of the hypothermia group improved one week after surgery (18). However, in another study in 2007, being consistent with the results of the present one, they reported no significant differences between normothermic and hypothermic methods at the time of discharge, with the difference that the hypothermic method was employed without rewarming in the present study (19). Consistent with the results of the present study, other studies showed no significant differences in cognitive functions between the two normothermic and hypothermic methods at the time of discharge (19-22). Hiraoka et al. used the MMSE questionnaire to survey cognitive functions of patients after aortic arch replacement surgery. The results of their study were inconsistent with those of the present study; accordingly, cognitive impairment after three weeks and six months from surgery was less severe in the hypothermic group than in the normothermic group. This difference could be attributed to the type of surgery, timing of postoperative cognitive function measurements, as well as the use of deep hypothermia in their study; however, in the present study, the hypothermic temperature of 32°C was utilized. It could be argued that deep hypothermia might have a protective effect on the nervous system. Besides, based on cognitive function assessments for the periods of two weeks and six months after surgery, cognitive impairment would gradually improve over time in both groups, indicating that more noticeable cognitive impairment occurred during hospitalization (15). The reason is that most studies have shown that severity of cognitive impairment decreases over time compared to the first days of hospitalization (15, 21, 22). The present study also showed a decrease in cognitive impairment in the last two days, i.e. on the fifth and sixth days. Many studies confirm that when rewarming slows down gradually, cognitive functions improve. Since rewarming did not slow down in the hypothermic group of the present study, cognitive impairment status in the hypothermic group could be attributed to this condition as against in the normothermic group (23-25). Another result of this study was the comparison of clinical outcomes in the two groups, which showed that clinical outcomes were better in the normothermic group than in the hypothermic group. Consistent with the results of the present study, research on warm heart surgery at the University of Toronto showed that cognitive impairment and other clinical outcomes after surgery were less severe in the normothermic method than in the traditional hypothermic method (26). Haddadzadeh et al., in their study, showed that clinical outcomes were more satisfactory in the normothermic group than in the hypothermic group (8). Similarly, Corno et al.'s study showed that the need for transfusion of blood products and ICU hospitalizations were less urgent in the normothermic method than in the hypothermic method. Respiratory status improved better in the normothermic method than in the hypothermic method (27). In addition, in the study of Pouard et al., clinical outcomes, such as length of stay at the ICU and the intubation duration were consistent with the results of the present study (28). In the same vein, the study of Caputo et al. showed that the normothermic method was more effective than the hypothermic method, yet there were no significant differences in clinical outcomes between the two methods (29). However, there was a significant difference in clinical outcomes between the two groups in the present study. Accordingly, based on the improvement in cognitive functions, clinical outcomes were better in the normothermic group than in the hypothermic group. Clinical outcomes are among those factors affecting cognitive functions in patients undergoing CABG (30).
5.1. Conclusion
The results of this study showed that cognitive impairment was less severe in the normothermic group than in the hypothermic group during hospitalization. In addition, the results showed that ICU length of stay, 24-hour drainage of chest tubes, and the transfusion rate were better in the normothermic group than in the hypothermic group.
5.2. Limitations
This study was conducted on elderly candidates for CABG at a hospital. Therefore, caution must be exercised in generalizing the results to other age groups and heart surgeries. Besides, the MMSE questionnaire was used in this study because it was not recommended to conduct long interviews and use other tests due to the age conditions of the patients in the early days of hospitalization. Accordingly, there was a need for a tool to allow the researchers to obtain cognitive status information with the least patient involvement in the present study; thus, we used the MMSE questionnaire in this study. The main strengths of this study included the sample size and homogeneity between the two groups of the study.