1. Introduction
Ruptured left ventricular pseudoaneurysm is per se a rare clinical entity and it would be low at the site of previous pseudoaneurysmorrhaphy (1). It needs high clinical suspicion index however planning a patient for surgery needs confirmation by imaging (2). In this case, cardiac MRI (CMR) provides excellent images essential for patient management (3).
2. Case Presentation
Our case was a 70-year-old male who presented with chest pain and dyspnea. In his past medical history, coronary artery bypass graft surgery and aneurysmectomy seven years ago was noticeable. Echocardiography data were as follows: Severe left ventricular (LV) systolic dysfunction (LVEF = 20 - 25%) with severe LV enlargement, scarred all apical segments, mid inferoseptal, mid anteroseptal walls, aneurysmal apex (6.15 cm × 2.19 cm) with a small rupture just at the most protruding part of it, to and from flow across this rupture site resulted in slow oozing of blood into pericardial sac with mobile clot in apex, clot formation in pericardial sac extended into biventricular apical parts and distorted apical and apicoseptal geometry without any communication with right ventricular cavity. Coronary angiography revealed three vessel diseases with patent grafts. Cardiac MRI images confirmed the presence of ruptured LV apex at the site of previous aneurysmorrhaphy patch and he underwent redo-pseudoaneurysmorrhaphy.
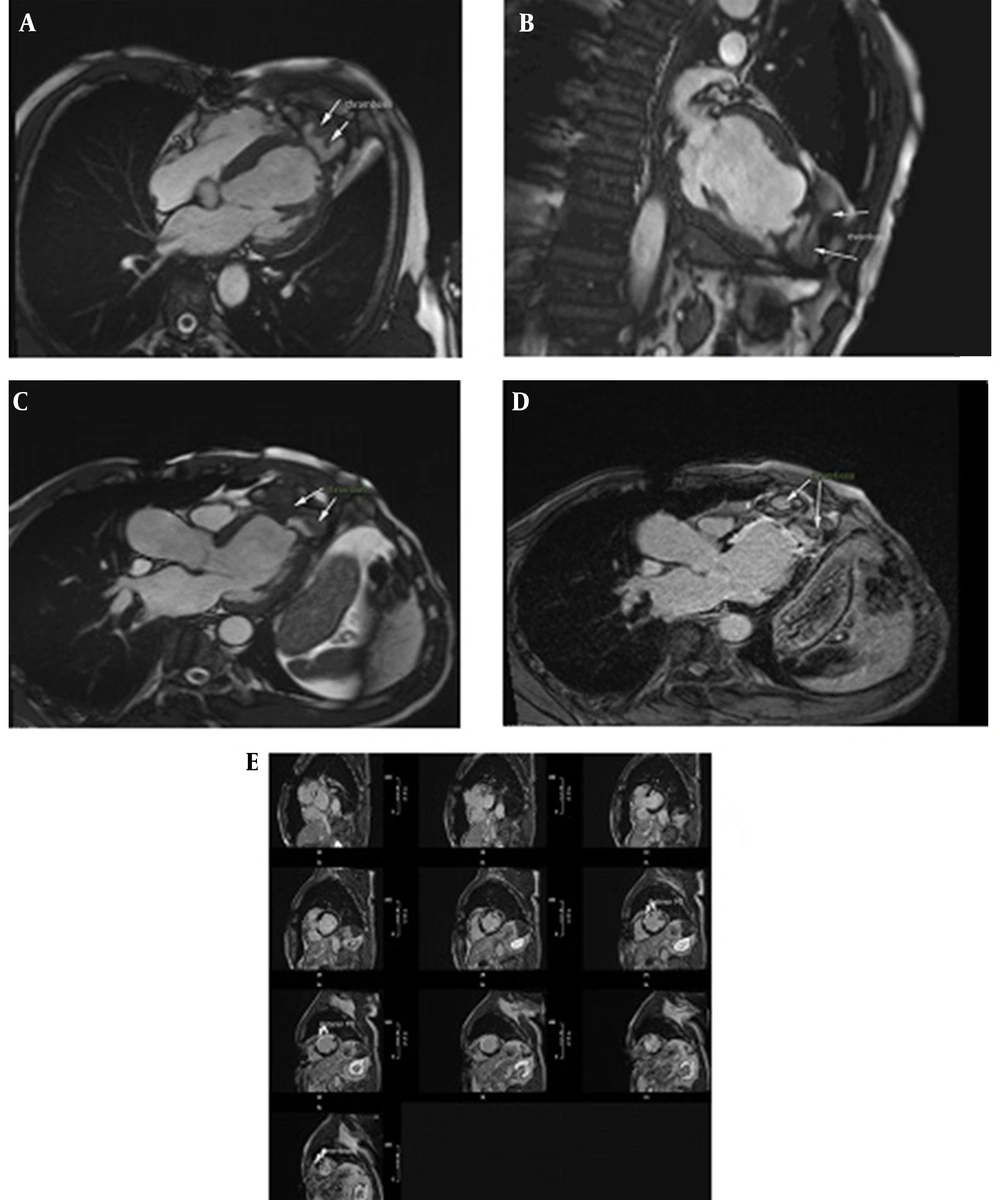
CMR data were as follows: Large pseudoaneurysm (depth: 46 mm, width: 60 mm), narrow orifice (5 mm), ruptured LV apical cap, septated LV apical outpouching surrounded by pericardial layers and included clots in different sizes and ages with no evidence of communication into RV cavity (Figure 1A and D). He underwent successful surgical resection of biventricular pseudoaneurysm.
(A), (B), (C): Cardiac MRI cine SSFP images in long axis views showed large left ventricular (LV) apical pseudoaneurysm with a free communication with the LV cavity (depth: 46 mm, width: 60 mm), narrow orifice (5 mm), ruptured LV apical cap, septated LV apical outpouching surrounded by pericardial layers and included clot (arrow) in different sizes with extension of pseudoaneurysm over right ventricle (RV) apex with no evidence of communication into RV cavity; (D), (E): Late gadolinium enhanced CMR images detected thrombus (arrow) within the pseudoaneurysm and also demonstrated enhancement within the wall of the pseudoaneurysm and surrounding akinetic segments indicative of anterior MI (arrow head).
3. Discussion
Recurrent rupture of LV pseudoaneurysm at the site of previous repair is a really rare but catastrophic clinical entity which occurs due to lack of myocardial support. This medical emergency condition leads to immediate collapse and electromechanical dissociation without prompt surgical intervention (4). Since most of the signs and symptoms are indistinguishable from ischemic ones, misdiagnosis rate would be high without enough clinical suspicion. In some instances, multiple imaging modalities are needed for a precise diagnosis. Cardiac MRI could determine the precise location of rupture and its extension with high sensitivity and specificity (5). In this case, extension of pseudo aneurysm to biventricular apices is determined using CMR which is really rare and is indicator of extensive myocardial rupture.
3.1. Conclusions
Recurrent ruptured pseudoaneurysm at the site of previous pseudoaneurysmorrhaphy is really a rare clinical entity especially in the case of biventricular apical extension. It needs high clinical suspicion index but planning a patient for surgery needs confirmation by imaging. In this case, CMR is really a good imaging modality for patient management.